Evolving reproductive health indicators for rural areas in China
In 2001, the World Health Organization published a list of 17 indicators incorporating clinical, social and environmental factors to be used for monitoring reproductive health, assessing reproductive health needs, and monitoring and evaluating programmes. However, the collection of data can be problematic, especially in rural areas of less developed countries. China has developed its own indicators, which it has found to be practical, feasible and measurable for its vast rural population, using a three-step approach. First, 32 women and 20 men who were involved in some aspect of reproductive health were brought together and divided into groups to generate ideas for potential indicators. This resulted in a list of 180 indicators in seven main categories: family planning, safe motherhood, child health, sexual health, governmental action on policy, women's status and rural community development. Some indicators were eliminated as impractical and others by low importance ranking, leaving a list of 126 possible indicators.
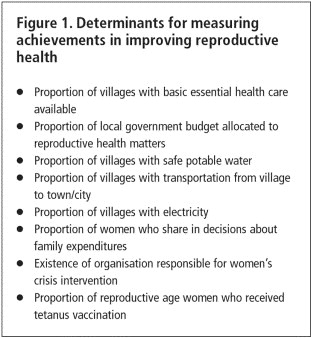
Next, 60 Chinese and 43 international experts, all with rural experience in developing countries, returned questionnaires rating the 126 indicators for practicality, feasibility and measurability, and ranking them in order of importance. This reduced the list to 50 indicators and generated 17 new ones. Six of the WHO's indicators, which had not been included, were added as well, and a second experts' survey was carried out on the 73 indicators. A list of determinants to measure achievements in improving reproductive health was also generated
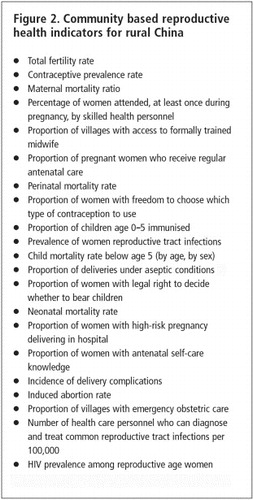
And a final list of 21 indicators was chosen, five that were identical to WHO indicators, three that were similar, and three new ones .The differences between the WHO indicators and those generated by this study reflect user as opposed to service provider perspectives, concerns relating to the status of women in the locality, and local custom and practice. It is interesting, however, that many indicators suggested in the first stage of the process, which related to wider issues of government policy and action, women's education and rural community development, were not included in the final lists.
Field tests of the process used were successful. Investigators were trained in the objectives of the study, the importance of keeping to procedures and the methods of recording data. Only about one-third of the data required were readily available from Maternal and Child Health Stations, and although the remainder could be collected from a variety of sources, reliability was difficult to ascertain. Nevertheless, the field trials showed it was possible, and the use of a standardised monitoring tool was seen to be an advantage for both health providers and decision-makers.
Although these indicators are unlikely to be usable in their entirety in other countries, many are relevant for large rural populations and adaptable to local conditions, along with the process used for generating them.1
| 1. | Wang CC, Wang Y, Zhang K et al. Reproductive health indicators for China's rural areas. Social Science and Medicine 2003;57:217–25. | ||||
Slow progress in reproductive health in Central and Eastern Europe
Only about 35% of the population of Central and Eastern European countries use modern contraceptives, with many others using withdrawal (18%) and the calendar method. Abortion is also often used. It has been estimated that in Russia about 60% of all pregnancies end in abortion. A variety of reasons account for these figures: family planning services are frequently under-funded; there is little integration of the services into primary health care programmes; there are few specialised family planning clinics or counsellors; counsellors are under-trained and often have misconceptions about the safety and efficacy of the full range of alternative contraceptives; religious views may make it difficult to counsel on contraception; and in Poland and Lithuania sterilisation is illegal. Even for those wanting to use modern methods, the costs can be high. Oral contraceptives are not normally subsidised and are therefore expensive, and in Romania, for example, these costs are not much less than the cost of an abortion. However, there are examples of good practice. In Armenia, 77 family planning clinics covering all administrative areas have been established over the last five years. In Romania, the government is committed to improving access to contraceptives. In Estonia, some groups of women, including students, those in the first three months post-abortion and those in the first year post-partum can get a 90% subsidy for contraceptives. This latter programme has been very effective in reducing the need for abortions.1
| 1. | Astra Network. Sexual and Reproductive Rights and Health in Central and Eastern Europe 2003;5. At: 〈www.astra.org.pl〉. | ||||
Applying STI syndromic management principles in Madagascar
At a health centre in Madagascar, 1,066 women presenting with vaginal discharge were tested for a range of STIs using simple laboratory techniques. These showed that 56% had bacterial vaginosis, 25% trichomoniasis and 6% syphilis. Using “high tech” ligase chain reaction (LCR) tests, 13% of the women were also shown to have gonorrhoea and 11% chlamydia. These detection rates were much higher than those obtained by more commonly used techniques for these infections, such as microscopy and culture. As most laboratories in the country do not have the facilities for these sophisticated techniques, it is recommended that patients who present with genital discharge should be treated syndromically for gonorrhoea and chlamydia, and screened for syphilis.1
| 1. | Behets FMTF, Andriamiadana J, Randrianasolo D, et al. Laboratory diagnosis of sexually transmitted infections in women with genital discharge in Madagascar: implications for primary care. International Journal of STD & AIDS 2002;13(9):606–11. | ||||
Combining contraceptive services and chlamydia screening in the UK
Chlamydia infection is often asymptomatic but it can lead to pregnancy complications, pelvic inflammatory disease and infertility. At an inner-city, community-based contraceptive and psychotherapy centre for young people, attendees were offered the opportunity to be tested for chlamydia when they came for other services. 73% took up this offer and of those with a positive or equivocal test, three-quarters returned for treatment. 87% of the treated patients returned for follow-up to confirm that treatment had worked. Most young people were willing to be tested, especially as a non-invasive urine test was used rather than a cervical swab. This study demonstrates that opportunities exist to monitor and treat STIs in clinics for young people.1
| 1. | Moens V, Baruch G, Fearon P. Opportunistic screening for chlamydia at a community based contraceptive service for young people. BMJ 2003;326(7401):1252–55. | ||||
Contraceptive use and the incidence of abortion
The relationship between contraceptive use rates and incidence of abortion depends on whether demand for fertility control methods is stable or rising. Intuitively it seems that as contraceptive availability increases, levels of abortion should fall, but this will only happen if demand is stable. If demand is on the increase, surveys suggest that both may rise simultaneously. A re-examination of information from 13 countries which have reliable data on both contraceptive use and the incidence of abortion shows both practices rising in six countries—Cuba, Denmark, Netherlands, United States, Singapore and Republic of Korea—but a rise in contraception and a fall in abortion in seven others—Kazakhastan, Kyrgyz Republic, Uzbekistan, Bulgaria, Turkey, Tunisia and Switzerland. The data suggest that rising contraceptive use and a fall in abortion incidence occur in those countries where fertility levels have stabilised. In comparison, simultaneous rises occur where contraceptive availability cannot keep up with the rise in demand, and abortion is used as a primary method of fertility regulation.1
| 1. | Marston C, Cleland J. Relationships between contraception and abortion: a review of the evidence. International Family Planning Perspectives 2003;29:6–13. | ||||
Making emergency contraceptive use easier
Over the last five years emergency contraception (EC) has been approved in over 80 countries and become increasingly available. How EC pills are accessed ranges from prescription by a health facility to supply by health workers to over-the-counter purchase from a pharmacy.1
The WHO-recommended regimen of the levonorgestrel-only pills is two doses of 0.75mg levonorgestrel taken 12 hours apart within 72 hours of unprotected intercourse. However, a recent trial2 has shown that a double dose, that is 1.5 mg levonorgestrel, taken all at once, is just as effective. Pregnancy rates were slightly higher among women who started treatment from 72–120 hours after unprotected sex, but the failure rates were far lower than have been reported in previous studies of the two-dose regimens. Although hormonal EC will never be as effective as insertion of an intrauterine device, this study suggests that levonorgestrel administered as a single dose up to 120 hours after unprotected sex has an important role to play in preventing pregnancy.1
| 1. | Webb AMC. Emergency contraception. BMJ 2003;326:775–76. | ||||
| 2. | von Hertzen H, Piaggio G, Ding J, et al. Low dose mifepristone and two regimes of levonorgestrel for emergency contraception: a WHO multicentre randomised trial. Lancet 2002;360:1803–10. | ||||
Predicting contraceptive demand in India
Childbearing intentions are often used to predict the need for contraceptive services but a follow-up study in India in 1999 of women who had participated seven years earlier in a National Family Health Survey suggests that this is a poor indicator. 61% of those who were not intending to have children nevertheless did so, almost as many as the 71% who had intended to have them. However, there was a better correlation of intention to use and use of contraception—49% of those intending to use contraception did so, compared with 29% of those who had not intended to do so. The woman's age and a history of child death were key factors leading to inconsistency between intention and behaviour. Contraceptive and childbearing intentions together were better able to predict actual contraceptive demand than either indicator alone, which may help programme planners to estimate future demand more accurately.1
| 1. | Roy TK, Ram F, Nangia P, et al. Can women's childbearing and contraceptive intentions predict contraceptive demand? Findings from a longitudinal study in Central India. International Family Planning Perspectives 2003;29:25–31. | ||||
Contraceptive implants perform well
Implantable contraceptives have been approved in more than 60 countries and are used by 14% of women choosing hormonal contraceptive methods, about 11 million women worldwide. A study of over 78,000 woman-years using Norplant shows a 1.5% pregnancy rate compared to 4.2% for copper-bearing IUDs over a five-year period. The two major drawbacks of implants are the cost and inconvenience of minor surgery for implantation and removal, and the well-documented side effect of irregular vaginal bleeding. Newer devices such as Jadelle and Implanon, which are safer and easier to insert and remove, are being studied to see whether they are as effective as Norplant and have fewer side effects. There is little doubt that implants are cost-effective in the USA and UK, but studies have not yet shown whether the same is true in developing countries.1
| 1. | Progress in Reproductive Health Research 2003;61. At: 〈[email protected]〉. | ||||
Failure to address post-partum anaemia in Uganda
Anaemia is a serious and common disorder which, when exacerbated by pregnancy, after can have serious consequences for both mother and child. In addition to immediate health problems it can lead to fatigue, reduced work performance and increased susceptibility to infection. It is therefore important that anaemia is addressed not only during pregnancy but also in the post-partum period when iron stores are low. This study investigated 349 post-partum women using both clinical signs and laboratory tests of haemoglobin levels. It found 64% of women to have anaemia—48.6% mild, 14.4% moderate and 1.4% severe. The women had not attended health clinics for post-partum check-ups, although 80 of the 349 presented at health clinics with other problems. This suggests two things: post-partum services should be increased and mothers should be checked and treated for anaemia at any post-partum clinical contact. The study also showed that the use of pallor as a clinical sign to detect anaemia was a sensitive method and detected most anaemic patients, but was not very specific, suggesting anaemia in some women who were not in fact anaemic.1
| 1. | Sserunjogi L, Scheutz F, Whyte SR. Postnatal anaemia: neglected problems and missed opportunities in Uganda. Health Policy and Planning 2003;18(20):225–31. | ||||
Training midwives in Afghanistan
Afghanistan has one of the highest rates of maternal and infant mortality in the world, the result of decades of conflict, chronic malnutrition, high fertility rates, the low status of women and a mainly rural population. A survey in 2002 estimated maternal mortality at 593 per 100,000 live births, and showed that only 10% of women received antenatal care, with less than 1% of births attended by a skilled attendant.1 Another survey suggested that most of the deaths were preventable, with 30% caused by haemorrhage and 23% by obstructed labour.2
In an effort to improve the country's maternal health indicators, the Ministry of Public Health in Kabul has prioritised the training of midwives. This is a major task. Since education of women was banned by the Taliban in 1996, there have been no new midwives trained or continuing education for trained midwives. Student midwives whose training was interrupted are now back in school and an innovative midwifery training programme, developed by Health Net International, has been started to train auxiliary midwives. This two-year programme trains rural women in the management of normal pregnancy, detection and referral of complications and high risk pregnancies, care of the neonate, health education for mothers and their babies, and training of traditional birth attendants. The programme is practical and competency-based, and uses WHO's Managing Complications in Pregnancy and Childbirth. The training of local women has additional advantages in that they are known to and come from the local community and unlike more highly trained health professionals, are likely to stay in the locality.1
| 1. | Gibson M, Mol D. Afghanistan: in the aftermath of conflict. International Midwifery 2002;15(6):6–8. | ||||
| 2. | UNICEF and Centers for Disease Control and Prevention joint study in Afghanistan. Associated Press. 6 November 2002. | ||||
Access to caesarean section still poor in sub-Saharan Africa
It is estimated that caesarean section is needed in about 5% of pregnancies to deal with obstetric complications and thereby decrease maternal and neonatal mortality. This figure is considerably exceeded in the West and in many Latin American and Asian countries, to a level where many caesareans are unnecessary. The situation in sub-Saharan Africa is quite different. With the exception of Kenya and possibly Ghana, the rate of caesarean sections is well below 5%, and has either remained low or actually fallen between the early and late 1990s. In Niger, less than 1% of births are by caesarean section and in Zambia the figure fell from 2.6% in 1992 to 1.6% in 1996. In all the countries studied, urban areas had a higher proportion of caesareans than rural areas, often as much as three times the rural rate (Table 1)
Table 1 Births by caesarean section (%)
| 1. | Buekens P, Curtis S, Alayon S. Demographic and health surveys: caesarean section rates in sub-Saharan Africa. BMJ 2003;326:136. | ||||
Public versus private antenatal care in Tanzania
Tanzania has encouraged the promotion of a private health sector to work alongside public providers. Now the relative quality of health care provision in the two sectors needs to be assessed. One method of doing so is to allocate a value to each of a range of features and compare these values in the two sectors. Results of such an investigation of antenatal care show that both public and private providers were reasonably good with respect to infrastructural aspects, such as toilets with water, private examination rooms, named diagnostic equipment, general cleanliness and availability of named drugs and vaccines, with a median score of 51/71 for the public and 64/71 for the private sector. Inter-personal aspects such as offering the pregnant woman a seat, interest being shown in her concerns and an appropriate explanation of procedures were also reasonably good in both sectors, with the private sector being slightly better. However both sectors were poor when it came to technical aspects of quality, for example not taking appropriate histories, disregarding guidelines on dispensing drugs and failing to perform tests for anaemia or urinary tract infections, with a median score of 18/39 for the public and 21/39 for the private sector. No assessments were made of the outcome of care in the two sectors, however, a surprising omission. Although the quality of care is somewhat better in the private sector by these measures, the cost of services is also higher. Approaches to improving antenatal care in both sectors should include strategies for gradual small changes, supported by regular quality assessment
| 1. | Boller C, Wyss K, Mtasaiwa D, et al. Quality and comparison of antenatal care in public and private providers in the United Republic of Tanzania. Bulletin of World Health Organization 2003;81(2):116–22. | ||||
Test tube babies come of age
It is now 25 years since the first successful birth of a child conceived by in vitro fertilisation (IVF). Over a million babies have now been born worldwide using IVF, pioneered in the UK in the 1970s. The stigma associated with such treatments and births is now fading. Recent advances in the technique now include sperm injection for male infertility. The overall success rate of IVF has also been improving, though slowly, with about one in four cycles being successful for couples under 40 years of age.1
| 1. | Holdsworth Associates. 25 years of IVF: media invite. 25 June 2003. At: 〈[email protected]〉. | ||||
Indian health care services are corrupt
A survey in India of public perception of the extent of corruption in public services put health care second only to the police. A quarter of all respondents said they had paid bribes for health services.1
| 1. | Kumar S. Health care is among the most corrupt services in India (News Roundup). BMJ 2003;326:10. | ||||