Abstract
Sex workers and their clients are particularly vulnerable to HIV/STI transmission. Most research on condom use has focused on barriers preventing use; less is known about attitudes, motivations and strategies employed by those who feel positively about condoms and who use them successfully. For this qualitative study, we conducted focus group discussions with sex workers (14), both female and transvestite, in Ciudad Juarez, Mexico, and female sex workers (17) and male clients (11) in Santo Domingo, Dominican Republic, who identified themselves as successful condom users in a condom use questionnaire. Discussions explored definitions of successful condom use, motivations and strategies for condom use and messages for future condom promotion. Sex workers defined successful condom use as being in agreement with their clients and partners about using condoms, protecting themselves from disease and unwanted pregnancy, and feeling good about using condoms. Condoms were seen to be hygienic, offer protection and provide a sense of security and peace of mind. Specific strategies included always having condoms on hand, stressing the positive aspects of condoms and eroticising condom use. Future educational messages should emphasise condom use to protect loved ones, increase security and pleasure during sex, and demonstrate respect for both sex workers, clients and partners.
Résumé
Les professionnels du sexe et leurs clients sont particulièrement vulnérables à la transmission du VIH et des IST. Les recherches portent généralement sur les obstacles contrariant l’emploi de préservatifs ; on connaît moins les attitudes, les motivations et les stratégies employées par ceux qui acceptent les préservatifs et les utilisent avec succès. Pour cette étude qualitative, nous avons organisé des discussions avec des professionnels du sexe (14 femmes et travestis), à Ciudad Juarez (Mexique), et des professionnelles du sexe (17) et des clients masculins (11) à Santo Domingo (République dominicaine), qui avaient déclaré utiliser avec succès les préservatifs dans un questionnaire. Les discussions ont étudié les définitions de l’utilisation réussie de préservatifs, les motivations et les stratégies pour l’utilisation des préservatifs et les messages pour leur promotion future. Pour les professionnels du sexe, l’utilisation réussie de préservatifs suppose d’être d’accord avec leurs clients et partenaires pour les utiliser, se protéger des maladies et d’une grossesse non désirée, et bien les tolérer. Ils estimaient que les préservatifs étaient hygiéniques, protégeaient et donnaient un sentiment de sécurité et de tranquillité. Les stratégies étaient de toujours avoir des préservatifs à disposition, souligner leurs aspects positifs et en érotiser l’utilisation. Les futurs messages doivent souligner que les préservatifs protègent les êtres chers, augmentent la sécurité et le plaisir pendant les rapports, et sont une marque de respect à l’égard des professionnels du sexe, des clients et des partenaires.
Resumen
Los trabajadores sexuales y sus clientes son particularmente vulnerables a la transmisión del VIH/ITS. La mayoría de las investigaciones sobre el uso del condón se han centrado en los obstáculos que impiden su uso; se conoce menos acerca de las actitudes, motivaciones y estrategias empleadas por aquellos que favorecen los condones y los usan exitosamente. Para este estudio cualitativo, realizamos discusiones en grupos focales con trabajadores sexuales (14), tanto mujeres como travestís, en Ciudad Juárez, México, y con trabajadoras sexuales (17) y sus clientes del sexo masculino (11) en Santo Domingo, República Dominicana, que se identificaron como usuarios exitosos del condón en un cuestionario sobre este uso. Durante las conversaciones se analizaron las definiciones del uso exitoso del condón, las motivaciones y estrategias para el uso del condón y los mensajes para una futura promoción del condón. Los trabajadores sexuales definieron el uso exitoso del condón como ponerse de acuerdo con sus clientes y parejas en cuanto a usar condones, protegerse contra enfermedades y embarazos no deseados y sentirse bien respecto al uso del condón. Los condones fueron percibidos como higiénicos, protección y algo que brinda seguridad y tranquilidad. Las estrategias específicas mencionadas fueron tener siempre un condón a la mano, recalcar los aspectos positivos del condón y erotizar su uso. Los futuros mensajes educativos deben hacer hincapié en el uso del condón para proteger a los seres queridos, aumentar la seguridad y el placer durante el sexo y demostrar respeto hacia los trabajadores sexuales, sus clientes y sus parejas.
Key Words:
The World Health Organization (WHO) estimates that there are 38 million new cases of curable sexually transmitted infections (STIs) each year in the Latin America and Caribbean region.Citation1 In 2005, the number of people living with HIV in the region was estimated at 2.1 million.Citation2 In Mexico and the Dominican Republic, where the study reported here took place, unprotected sex between sex workers and their clients often translates into high HIV and STI rates.Citation3Citation4Citation5Citation6
The Dominican Republic has a high number of people in the sex trade per capita, with some 50,000 female sex workers in Santo Domingo alone. A 2005 Ministry of Health study reported that HIV prevalence among Santo Domingo sex workers was 3%, compared to 1.7% in the general adult population.Citation4Citation7
In Mexico, national HIV prevalence is 0.3% in the general adult population, 0.5% among female sex workers, and 6.1% among male sex workers.Citation2Citation3 In Ciudad Juarez, at the US–Mexico border, sex workers regularly engage in high-risk sex with clients, including thousands of truck drivers carrying freight across the border. Violence and lawlessness are rife; the city has seen the abduction, rape, murder and disappearance of up to 600 Ciudad Juarez women in the past decade, likely including sex workers.Citation8
Research on condom use among sex workers and clients typically looks at barriers to condom use and risk factors that predispose to non-use. A recent qualitative study of female sex workers in the Mexican border city of Tijuana identified three major barriers to condom use: personal dislike of condoms, negative client reactions to condoms and financial incentives offered by clients for sex without a condom.Citation5 Street-based female sex workers in Mexico City reported high levels of condom use with clients (94%), but 73% never used condoms with their romantic partners, a finding that underscores the challenge of promoting safer sex in both the professional and private lives of sex workers.Citation9
Yet, there remains a scarcity of information on what differentiates successful condom users from inconsistent and non-users.Citation10 The concept of positive deviance is particularly relevant to addressing these knowledge gaps, in this case learning what the enabling factors are that motivate the relatively few individuals who do use condoms in order to develop successful condom promotion campaigns.Citation11Citation12
Sexual health researchers have long struggled to define and measure the concept of “successful condom use”, for which there is no universally accepted definition. For example, in some cases, successful condom use has been defined by researchers as using condoms with all partners in the past six months, but condom users themselves may define success as using condoms 100% of the time with secondary partners but less frequently with primary partners.
NGO partners working with sex workers in Santo Domingo and Ciudad Juarez
We decided to conduct this study in the Dominican Republic and Mexico based partly on the interests of donors and partly due to the encouragement of local NGOs with whom the Population Council has worked on previous projects. In Santo Domingo, we worked with the Centro de Orientación e Investigación Integral (COIN), which since the 1980s has worked with local sex workers to establish a network of peer health educators, develop and distribute educational materials and implement HIV prevention activities. Their educational materials featuring a Dominican sex worker called Maritza have been particularly successful as a peer education tool in addressing strategies such as negotiating and eroticising condom use with clients, refusing drunk, high or violent clients and keeping the client interaction as safe as possible for the sex worker.Citation6, Citation13 COIN was also influential in the formation of the Movimiento de Mujeres Unidas (MODEMU), a Dominican sex worker union run entirely by sex workers for sex workers, with whom we also worked to develop the current study protocol and instruments.
In Ciudad Juarez, we worked with the Federación Mexicana de Asociaciones Privadas de Salud y Desarrollo Comunitario (FEMAP), a health and community development NGO that has been operating for nearly 40 years. FEMAP has long experience working with female and male sex workers, particularly street-based sex workers, to educate them about HIV prevention, offer health referrals, provide condoms, address substance abuse and encourage transition out of sex work using grounded, respectful approaches. FEMAP put us in touch with a small group of sex workers who reviewed study plans and instruments during the design stage.
Methodology and participants
The research involved two components: first, the development and administration of a condom user scale that attempted to bring us closer methodologically to the meanings of successful condom use, and second, a qualitative exploration of the definitions of and conditions for successful condom use with a subset of respondents to the condom use scale.
Potential participants were screened to identify those meeting eligibility requirements (sexually active and had ever used condoms). Eligible participants then responded to a questionnaire with statements on condom use, attitudes towards condoms, positive and negative experiences with condoms, and beliefs about condoms. The questionnaire contained a 93-point scale for sex workers and a 75-point scale for male clients. A few questions were included from both the Sexual Relationship Power ScaleCitation14 and Sunmola’s scale for measuring barriers to condom use.Citation15 And questions were added on frequency of condom slippage and breakage, how much participants agreed or disagreed with statements about the benefits of condoms, and whether condoms interfered with the enjoyment of sex. Early drafts were piloted with sex workers in both sites and revised prior to field work.
A team of interviewers administered the condom user scale to 101 Mexican sex workers and to 71 sex workers and 30 male clients in the Dominican Republic. The participants were offered condoms and informational material on local NGOs as thanks for their time. Those who scored over half the possible points on the condom use scale and met other basic criteria were then invited to participate in focus group discussions. 42 accepted: 17 Santo Domingo sex workers, 11 Santo Domingo male sex clients, and 14 Ciudad Juarez sex workers, both female and transvestite. The transvestite sex workers were men who described themselves as trasvestis or vestidas, who dressed as women and had male sexual organs.
This paper presents the qualitative findings from the focus group discussions. The findings from the condom use scale are still being analysed. There were four focus groups in Ciudad Juarez (two with female sex workers and two with transvestite sex workers) and four in Santo Domingo (two with female sex workers and two with male clients). In Santo Domingo, male clients who participated in the study were recruited independently of sex workers; they were not necessarily clients of the participating sex workers. The discussions were audio-taped and held on-site at the offices of the local collaborators. We reimbursed all participants for their travel costs and gave them condoms and informational materials on local health NGOs. Informed consent was obtained from all participants and privacy and confidentiality were assured. The Population Council’s Institutional Review Board approved the study protocol.
The transcripts were analysed for relevant ideas and themes. The research methodology was the same in both sites. The aim was not to compare findings between sites; nevertheless, where clear distinctions emerged, they are noted.
Mexican participants in the study were street-based sex workers, while Dominican participants were locale-based sex workers and male clients of sex workers. Locale-based sex workers either work in what Dominicans describe as “indirect” sex work locales (i.e., employed by bars and discos as waitresses or dancers but also engaged in selling sex to clients), or direct sex work locales such as brothels, where their only source of income is selling sex. In Santo Domingo, most sex work is indirect.Citation16
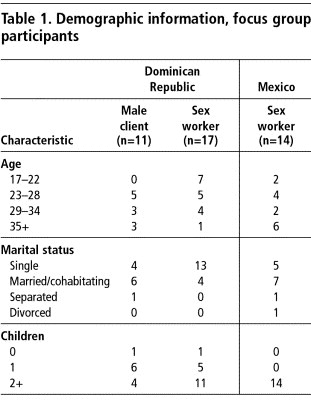
Table 1 gives basic demographic information about the participants, obtained using a brief questionnaire filled out immediately prior to the focus group discussions, but unlinked to specific individuals. At least half the Dominican male clients and Mexican sex workers were married or cohabitating, while the majority of Dominican sex workers were single. A large majority of participants across all three groups had at least one child, and all of the Mexican sex workers had two children or more. A small majority of Mexican sex workers were aged 29 or older, whereas the majority of Dominican sex workers were under age 29. Male clients were aged 23 and older.
Several of the transvestite sex workers were from other northern Mexico cities and several had at least some primary or secondary education. At least half of the Dominican sex workers had migrated to Santo Domingo from other cities; most had completed primary but not secondary school. All the transvestites used women’s names during sex work, and several reported using their male names when not dressed as women. Most transvestites reported having a current stable partner. Several of the Mexican women mentioned using drugs, which they said helped them to deal with sex work. One of the Dominican participants was pregnant at the time of the focus group. Many of the Dominican male clients reported having experienced an STI in the recent past.
First exposure to condom information
Most of the Dominican sex workers said they learned about condoms through COIN and MODEMU health promoters and peer educators, and some also from family planning providers. Most of the sex workers in Ciudad Juarez said they had taught themselves how to use condoms; nearly all of them routinely obtained condoms through FEMAP peer educators. A local hotel was also said to provide condoms. Most of the male clients described having had conversations in their youth with friends or male relatives who first taught them about condoms. In contrast, the majority of transvestites said that they had first heard of condoms in primary or secondary school.
Definitions of successful condom use
Female sex workers in the Dominican Republic defined successful condom use as being protected from disease and avoiding pregnancy, and being in agreement with their client about using a condom. One woman explained that successful condom use also meant that she and her partner felt good about condom use. Another participant felt that using condoms successfully meant going to the doctor, being tested for STIs and feeling healthy. According to female sex workers in the Dominican Republic, like themselves, “successful condom users are people who enjoy using condoms and who try to convince others to use them”. Other characteristics of successful condom users included being sure of yourself, not getting sick or pregnant, being careful about who you go out with and trying to go out with the same clients.
Female sex workers in Mexico also described successful condom use with stable partners as being in agreement with or on the same page as their partner; however, these women also defined success as “always using condoms”, “having an orgasm” and using condoms without breakage. As one Mexican woman stated: “When I have had sex and the man has had an orgasm, then it has been successful. It is not successful when the condom breaks and gets stuck inside of you.” The women also described successful condom users as individuals who are conscious of the need to protect and take care of themselves, who know how to use a condom well and who enjoy using condoms. According to female sex workers in Ciudad Juarez, successful condom users feel secure about using condoms, are able to talk about STIs openly with partners, peers and healthcare providers, and feel that their life is important. Similarly, a Dominican male client described a successful condom user as “a person who takes care of himself or herself and the family” and another client elaborated that successful condom use is “when you forget about the issue of whether you feel it [the condom] or not and you just always use it”.
Motivations for condom use
At both sites, sex workers noted that a motivating factor in the decision to use condoms was a desire to remain healthy and not succumb to STIs or HIV. Several sex workers spoke openly about personal experiences of friends or acquaintances (and less frequently, family members) living with or dying from AIDS; all sex workers also shared related concerns about simply staying healthy for the sakes of their families. Similarly, several Dominican male clients had witnessed the death of a loved one from AIDS. Such personal experiences were also more common among the Dominican sex workers and seemed to influence their motivation to use condoms more so than the Mexican sex workers.
“[I’m motivated to use condoms] to protect myself from infections because I wouldn’t want people to be saying to my kids when they grow up: ‘Your mom died of AIDS.’” (Female sex worker, DR)
“I’ve seen several people in my neighborhood who have died of AIDS, even a 17 year-old girl. That made me really sad.” (Female sex worker, DR)
“What motivated me [to first use condoms] was when a friend died of AIDS and I saw how he died and I started to use condoms. He was my best friend.” (Male client, DR)
“In my case, my brother died of AIDS and all of us at home were scared by how it affected him. Nobody used to believe in AIDS, but after that, we all believed in it and I started to use condoms.” (Male client, DR)
Many male clients spoke about their desire to protect their wives and girlfriends from pregnancy and disease.
“I started using condoms because my girlfriend can’t use other [contraceptive] methods. So I use condoms with her. I’m a womaniser; I also have to use condoms with her because I go with prostitutes.” (Male client, DR)
“I learned about condoms when a girl gave me genital warts; I started using condoms because I have a family.” (Male client, DR)
While the Mexican transvestites were concerned about protecting their own health as a motivation to use condoms, several were even more concerned about protecting the health of their clients and other people. Unlike the participants in any of the other groups, the transvestite participants cited client health as one of their top motivations.
Sex worker strategies to ensure condom use with clients
Sex workers in both sites used similar strategies to ensure condom use with their clients. The most basic strategy was simply having condoms on hand and carrying a supply in their bags. The women also felt it was crucial to communicate their desire to use condoms prior to engaging in sexual activity so that they could refuse sex, leave or threaten to leave the client if he refused to use a condom.
“I have condoms at home and at times I bring two with me in my purse and when I am working a lot and there aren’t any left, I ask one of the other girls to lend me one.” (Female sex worker, Mexico)
“I tell him, ‘No party hat, no party.’” (Female sex worker, DR)
“If I don’t know a client, I tell him beforehand that I use condoms and I ask him: ‘Do you use condoms?’ One time I left a man lying in a hotel room and at the reception… they asked me why and I said that he didn’t want to use a condom and they said to me ‘Congratulations’.” (Female sex worker, DR)
“You have to make sure you are both in agreement at the beginning of the encounter. It’s really important to say, this is what I’m going to do and we are going to make sure that we agree on the condom, on using the condom.” (Female sex worker, Mexico)
“I don’t convince them. If they don’t want it with a condom, then they don’t come in.” (Female sex worker, Mexico)
Many sex workers also described how they frequently convinced their clients to use condoms by explaining the risks of unprotected sex. An additional strategy that sex workers used was to remind clients of their families and the importance of protecting them from disease.
“Take care of your family, your children and father and everyone, by taking care of me.” (Transvestite sex worker, Mexico)
Once condom use has been agreed, the majority of sex workers preferred putting condoms on clients themselves. There was consensus in all groups that this ensured it was done correctly and safely, with the added advantage of allowing foreplay and games to eroticise condoms.
“I hold it [the condom] like this with two fingers. I unroll it so that no air gets inside because many times it breaks. This way he can keep his erection.” (Female sex worker, Mexico)
“I put it on because clients don’t know how and this man, he’ll come and puncture the condom. I feel safer putting it on him myself.” (Female sex worker, DR)
Many sex workers also described remaining firm in their refusal to have sex with a client without a condom, even in the face of violence:
“If you put it on, I’ll give you a blow job. Or I’ll put it on with my mouth.” (Female sex worker, DR)
“I fire him [if he doesn’t want to use a condom] (laughing).” (Transvestite sex worker, Mexico)
“A while ago a guy hit me because he did not want to use a condom. I told him, ‘You know what? Between you hitting me and me getting an STI, I’d rather have you hit me.” (Female sex worker, Mexico)
While some Dominican male clients described putting condoms on themselves, using foreplay and discussing the importance of condom use prior to engaging in intercourse, for most men these responsibilities belonged to the sex worker. A few male clients did describe refusing sex when a sex worker did not want to use a condom, but in the majority of cases, men said it was the sex worker who returned their money and declined sex. Several clients also made the distinction between women who worked for establishments and women working on the street, as they perceived the latter to be less conscientious about condoms. One client stated: “It’s safer to be with a woman from an establishment than a woman you meet on the street, because women from the establishments won’t sleep with any man without a condom.”
Successful condom use by partner type
The ease with which the female sex workers used condoms successfully seemed very much related to the type of relationship they had with the partner. Many Dominican sex workers felt it was easier to use condoms with short-term clients and men they did not know than with their spouses, regular partners or long-term, trustworthy clients. For many of the women, it was the expectation of trust at all costs in more established relationships that made condom use so difficult. Mexican female sex workers expressed similar sentiments, explaining that regular partners would get angry and at times violent when “treated like a client”. Male clients in the Dominican Republic and transvestite sex workers in Mexico made similar distinctions. With one-time or short-term clients, many transvestite sex workers felt it was easier to use condoms because both parties had an interest in not putting themselves at risk of HIV.
“When you’ve been seeing a client for two or three months, they say: ‘Why use a condom if we have known each other for so long?’” (Female sex worker, DR)
“They say to you, ‘OK I will put it on today, but next week if you bother asking again forget about it.’” (Female sex worker, DR)
“He says I don’t love him because I use a condom with him, that I treat him like a client. He says, ‘I’m not a client like the ones you have had.’” (Female sex worker, Mexico)
“It is most difficult with the wife because almost no one uses condoms with a regular partner.” (Male client, DR)
“It is more difficult with my wife because of the trust I have in her, despite the fact that with trust comes danger.” (Male client, DR)
“With partners it is difficult to use a condom because you’ve had time to get to know the person.” (Transvestite sex worker, Mexico)
Positive aspects of condom use
The majority of female sex workers at both sites reported that condoms did not reduce sexual satisfaction and that sex did not feel any less pleasurable with a condom. They explained that sexual pleasure is largely psychological and therefore can be achieved easily when using a condom if a person adopts the correct frame of mind. Responding to the belief among many men that sex with a condom does not feel the same, one Dominican woman responded: “That is their own psychosis, because for me I feel the same satisfaction.” One Dominican woman said sex can last longer when she uses a condom, while another stated that using condoms has in fact increased her “attractiveness” to clients. A few female sex workers, however, did make a distinction between using condoms with clients and regular partners, claiming that sex was better without condoms with regular partners, and acknowledging that this difference was probably also due to the emotional connection to the partner.
“It’s the same for me. Well, no, it’s not exactly the same. With my partner it’s better without a condom, but with a client it doesn’t matter if he feels the same or if he doesn’t.” (Female sex worker, Mexico)
Other advantages of condoms recognised by female sex workers in both countries were their dual protection from STIs and pregnancy and the sense of cleanliness and hygiene that condoms offered. They saw condoms as an easy and affordable form of contraception. Benefits of hygiene and ease of use were closely linked to feelings of security, protection and peace of mind when using condoms. One Dominican woman said condoms can improve self-esteem and allow women to feel more in control of the sexual encounter. Similarly, transvestite sex workers in Ciudad Juarez explained that condoms made them feel good and gave them peace of mind.
Although the majority of transvestite sex workers acknowledged that sex with a condom was less satisfactory, they shared the women’s view that condom use was essential to prevent STIs/HIV.
“Yes, a lot of times [condoms interfere with sexual satisfaction], and most people know that and say, ‘But it is so much better like this [without condoms]’, but the fact is you have to use them.” (Transvestite sex worker, Mexico)
One transvestite said it was sometimes a challenge to use condoms with clients who were very attractive. Another described a situation in which he did not want to use a condom, but his client put it on him. A minority said they did not notice any difference in sexual satisfaction with condoms. Others echoed the women’s sentiments that condoms affect sex more with a stable partner than with clients.
Similar, positive opinions emerged among male clients in the Dominican Republic. Condoms were considered advantageous because they made men feel protected and reassured them that they were taking precautions to protect their own lives. Even among those who acknowledged that sexual satisfaction was diminished using condoms, the protective effects of condoms outweighed the decreased satisfaction:
“Yes, I can say it does not feel the same; you are better off masturbating [compared to having less pleasurable sex with a condom]. [But] having sex with a condom is an obligation.” (Male client, DR)
Ideas for condom promotion campaigns
Participants suggested using positive messages for health communication campaigns promoting condom use. Apart from condom effectiveness in preventing STI/HIV transmission or pregnancy, most mentioned the feelings of security and protection of self and family as effective messages for condom promotion campaigns to emphasise:
“Protect yourself and your family from an unwanted pregnancy.” (Female sex worker, DR)
“If you are going to have sex with another person, always think of your partner and use a condom.” (Female sex worker, DR)
“Use a condom, because to use a condom is to love yourself and love others.” (Female sex worker, DR)
“You should use condoms to take care of yourself, to feel secure.” (Transvestite sex worker, Mexico)
Both female sex workers and clients were conscious of the benefits of condom use both for their own well-being and the benefit of their loved ones. One client thought educational campaigns should focus less on the negative effects of not using condoms, and more on their positive aspects.
“Campaigns about condoms are really bad because they say condoms are to prevent pregnancy or diseases but that doesn’t motivate you to use condoms. What motivates you is information about what a condom is and why you use it, how you can feel when using it.” (Male client, DR)
The transvestite sex workers voiced similar opinions about promoting the feeling of security that condoms can provide, with one calling condom use “a message of life”. Several added that it was important to focus on male adolescents who have sex with men. Elaborated one participant, “I would target youth as well, because nowadays youth aged 14 to 16 are the ones who have more sex with gay men compared to older men.”
Other ideas suggested by sex workers in both sites included the use of personal testimonials, encouraging businesses to convince their customers to use condoms and finally, convincing the public that sex can be enjoyable and more carefree with condoms.
Discussion
It was clear from the richness of the qualitative study that the condom use scale was effective in leading us to a subset of positive-minded, successful condom users. Working closely with local NGOs helped to ensure that our instruments, methods and recruitment strategies were culturally sensitive. Whether or not this same scale, instruments and so on would be appropriate in other settings would require testing and validation elsewhere.
The qualitative methodology and working with small, non-representative samples of sex workers and clients limits the generalisability of our findings, even though we are confident that saturation was achieved with female sex workers in both countries. Moreover, the experience of sex workers with no access to NGO and peer support structures might be entirely different. Nevertheless, the findings have important implications both for public health programmes promoting condom use and future research on condom use behaviour.
Sex workers in both cities defined successful condom use as being in agreement with their sexual partners about using condoms, protecting themselves from disease and unwanted pregnancy and feeling good about using condoms. Condoms were seen to offer protection, were hygienic and provided a sense of security and peace of mind. Similar findings in sex worker and client populations have been reported in an earlier study among Santo Domingo sex workers, who cited the maintenance of personal health, protection of one’s family and a sense of peace as advantages of condom use.Citation17 While positive experiences with condoms and feelings of security are not new for this population, linking such concepts to the effective use of condoms distinguishes our current study.
Although successful condom use is often measured only in terms of frequency and consistency of use, very few participants mentioned these concepts. Rather they characterised successful condom use in terms of meeting personal goals. These included the public health goals of avoiding unwanted pregnancy and preventing STI/HIV transmission but also the importance of gaining a sense of personal security during the sex act.
Thus, a disparity between definitions of successful condom use as used by the research community as opposed to sex workers and clients can be discerned, where the context of the sexual encounter and positive feelings about condoms can be just as, if not more, important than whether condoms are used consistently. This disparity deserves attention. In 1999, Dominican NGOs collaborated on interventions to encourage condom use among female sex workers in Santo Domingo and Puerto Plata. While the programme significantly increased condom use with new clients in both cities, post-intervention STI prevalence remained high, with 16% of Santo Domingo sex workers testing positive for at least one of gonorrhea, trichomonas or chlamydia (compared to 26% pre-intervention).Citation13 The importance of consistency of use as a necessary part of achieving personal goals should become part of condom promotion work with sex workers and clients.
The study participants’ definitions of successful condom use also have an important implication for condom promotion. Anecdotally, field collaborators in Santo Domingo reported that condom promotion in the Dominican Republic consists mostly of negative, fear-based messages. Sex workers and male clients agreed, however, that instead of focusing on preventing negative health consequences, the positive benefits of condoms should be emphasised.
Finally, both sex workers and clients in both sites appeared to agree that sex workers must assume the bulk of the responsibility for ensuring condom use. Sex workers both articulated and employed the following strategies for successful condom use:
| • | always have condoms on hand, no excuses; | ||||
| • | clearly communicate the rules and establish that condom use is non-negotiable before committing to the sexual transaction; | ||||
| • | reason with clients, discussing the health risks of sex without a condom and highlighting the health benefits for the client’s family or other sexual partners; | ||||
| • | eroticise condom use and assure the client that his pleasure is the number one goal of the encounter; | ||||
| • | place the condom yourself, so that it is done correctly, reducing the chances of slippage or breakage; and | ||||
| • | walk away from a client who appears unwilling to use a condom. | ||||
Future educational messages should emphasise condom use to protect loved ones, increase security and pleasure during sex, and demonstrate love and respect for partners. These steps, grounded in sex workers’ real-life experiences, may help public health practitioners and peer educators to condom promotion messages and interventions more effectively.
Acknowledgements
We are grateful for the generous support of the Moriah Fund and the USAID-funded Interagency Gender Working Group, and to the study participants and our collaborators FEMAP, COIN and MODEMU, particularly Dr Enrique Suárez and Graciela de la Rosa of FEMAP and Francisca Ferreira and Luis Moreno of COIN. We are especially thankful to Ms Davida Becker and Ms Lisa Goldman, with the Population Council during the study, who supported field work. Preliminary findings were presented at the 2003 International Society for Sexually Transmitted Disease Research Biennial Meeting and the 2003 American Public Health Association Annual Meeting. In 2004, Michelle Firestone presented study findings in her Master of Health Science thesis, Department of International Health, Johns Hopkins Bloomberg School of Public Health, USA.
References
- World Health Organization. Global Prevalence and Incidence of Selected Curable Sexually Transmitted Infections: Overview and Estimates. 2001; WHO: Geneva.
- UNAIDS, WHO. AIDS Epidemic Update: December 2005. 2005; UNAIDS: Geneva. At: <http://www.unaids.org/epi/2005/doc/report_pdf.asp>. Accessed 26 July 2006.
- Consejo Nacional para la Prevencion y el Control del VIH/SIDA. Panorama epidemiológico del VIH/SIDA e ITS en México, 31 de diciembre del 2005. México City, 2005. At: <http://www.salud.gob.mx/conasida/estadis/2005/dic05/panoramadic05.pdf. >. Accessed 26 July 2006.
- SB Baldwin, B Djambazov, M Papenfuss. Chlamydial infection in women along the US-Mexico border. International Journal of STD & AIDS. 15: 2004; 815–821.
- J Bucardo, SJ Semple, M Fraga-Vallejo. A qualitative exploration of female sex work in Tijuana, Mexico. Archives of Sexual Behavior. 33: 2004; 343–351.
- D Kerrigan, L Moreno, S Rosario. Combining community approaches and government policy to prevent HIV infection in the Dominican Republic. 2004; Population Council: New York.
- Secretaria de Estado de Salud Pública y Asistencia Social de República Dominica. De segunda generación encuestas de seroprevalencia de la infección VIH basadas en puestos centinelas 2004. Santo Domingo, 2005.
- M Ensalaco. Murder in Ciudad Juarez: a parable of women’s struggle for human rights. Violence Against Women. 12(5): 2006; 417–440.
- B Allen, A Cruz-Valdez, L Rivera-Rivera. Afecto, besos, y condones: el ABC de las prácticas sexuales de las trabajadoras sexuales de la Ciudad de México. Salud Pública de México. 45(S5): 2003; S594–S607.
- Interagency Gender Working Group. Research Gaps Related to Gender Issues and Population, Health, and Nutrition Programs: An Analysis. Washington DC, 2000. At: <http://www.prb.org/pdf/researchgaps.pdf. >. Accessed 28 July 2006.
- DR Marsh, DG Schroeder, KA Dearden. The power of positive deviance. British Medical Journal. 329: 2004; 1177–1179.
- S Babalola, D Awasum, B Quenum-Renaud. The correlates of safe sex practices among Rwandan youth: a positive deviance approach. African Journal of AIDS Research. 1: 2002; 11–21.
- D Kerrigan, L Moreno, S Rosario. Environmental–structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. American Journal of Public Health. 96(1): 2006; 120–123.
- J Pulerwitz, H Amaro, W De Jong. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 14: 2002; 789–800.
- AM Sunmola. Developing a scale for measuring the barriers to condom use in Nigeria. Bulletin of World Health Organization. 79: 2001; 926–932.
- D Kerrigan, L Moreno, S Rosario. Adapting the Thai 100% condom programme: developing a culturally appropriate model for the Dominican Republic. Culture, Health and Sexuality. 3: 2001; 221–240.
- D Kerrigan, L Moreno, S Rosario. Investigación Operacional sobre un Programa de Uso de Condones 100% Santo Domingo, República Dominicana. 1997; AIDSCAP/Family Health International: Santo Domingo.