Abstract
As part of a multi-country study, maternal health services were reviewed in one health district in Gauteng Province, South Africa. Poor record-keeping, inadequate supervision, poor levels of clinical knowledge and under-utilisation of midwife obstetric units were found. Interventions identified by local health service personnel to improve maternity care were developed, implemented and evaluated, included programme-specific (training in prevention of mother-to-child transmission of HIV and neonatal resuscitation) and system interventions (improving interpersonal relations and system functioning, use of routine data for monitoring purposes, improving supervision skills). This resulted in some positive outputs. Health worker knowledge and patient records improved, and there was some indication that supervision improved. However, system-wide interventions that could improve programmes were less successful. To build a learning organisation, a new culture of monitoring and evaluation, including routine self-evaluation, is required as core skills for all health workers. These data should be used at the point of collection. Changing reporting lines between programme and district managers may improve co-ordination between different authorities, and there is a need to enhance the manner in which staff are assessed, appraised, promoted and rewarded. Professional bodies who oversee training curricula, institutions that offer training, and institutions that provide funding for training and development need to take on the challenge of health systems development and avoid promoting programme-specific interventions only.
Résumé
Une étude plurinationale a examiné les services de santé maternelle dans un district sanitaire de la province de Gauteng, Afrique du Sud. Elle a révélé une mauvaise tenue des dossiers, une supervision médiocre, de faibles niveaux de connaissances cliniques et un sous-emploi des services obstétricaux. Des interventions identifiées par le personnel des services de santé locaux ont été appliquées et évaluées. Ces mesures étaient spécifiques au programme (formation à la prévention de la transmission mère-enfant du VIH et réanimation néonatale) ou systémiques (amélioration des relations interpersonnelles et fonctionnement du système, utilisation systématique de données aux fins du suivi, amélioration des compétences de supervision). Leurs résultats ont été positifs sur les connaissances des agents de santé et la tenue des dossiers, et il semble que la supervision se soit améliorée. Néanmoins, les interventions systémiques susceptibles de corriger les programmes ont eu moins de succès. Pour construire une organisation apprenante, une nouvelle culture du suivi et de l’évaluation, et notamment une auto-évaluation systématique est requise comme compétences fondamentales pour tous les agents de santé, et des données doivent être utilisées au point de collecte. Modifier les modalités des rapports entre les directeurs des programmes et des districts peut resserrer la coordination entre différentes autorités et il est nécessaire de perfectionner les méthodes d’évaluation, de promotion et de récompense du personnel. Les organes professionnels qui encadrent les programmes de formation, les institutions qui proposent une formation et celles qui financent la formation et le développement doivent éviter de promouvoir uniquement les interventions circonscrites aux programmes.
Resumen
Como parte de un estudio realizado en varios países, se analizaron los servicios de salud materna en un distrito de salud de la Provincia de Gauteng, en Sudáfrica. Se encontraron registros deficientes, supervisión inadecuada, bajos niveles de conocimientos clínicos y subutilización de las unidades obstétricas de parteras. Las intervenciones identificadas por el personal de salud local para mejorar la atención de maternidad fueron formuladas, aplicadas y evaluadas, incluidas las intervenciones específicas a programas (capacitación en la prevención de la transmisión materno-infantil del VIH y la reanimación neonatal) e intervenciones de sistema (mejoras en las relaciones interpersonales y el funcionamiento de sistemas, uso de datos rutinarios para fines de monitoreo, mejoría de habilidades de supervisión). Esto tuvo algunos resultados positivos. Mejoraron los conocimientos de los trabajadores de salud y los registros clínicas, y hubo indicios de que mejoró la supervisión. Sin embargo, las intervenciones realizadas en todo el sistema que podrían haber mejorado los programas, fueron menos exitosas. Para crear una organización de aprendizaje, se necesita una nueva cultura de monitoreo y evaluación, que incluya la autoevaluación rutinaria, como habilidades fundamentales de todos los trabajadores de salud, y se deben utilizar los datos en el momento de la recolección. Al cambiar las líneas de informe entre los administradores de programas y distritos, posiblemente mejore la coordinación entre diferentes autoridades, y se debe mejorar la forma en que el personal es evaluado, valorado, ascendido y recompensado. Las entidades profesionales encargadas de los currículos de capacitación, las instituciones que ofrecen capacitación y las que proporcionan financiamiento para la capacitación y el desarrollo deben asumir el reto de desarrollar los sistemas de salud y evitar promover exclusivamente intervenciones específicas a los programas.
This research intervention, part of a multi-country study in South Africa, Tanzania and Cape Verde, aimed to improve maternal health services using a health systems approach rather than only a programme perspective. In phase one, a common data collection tool was applied to describe maternal health services. In phase two, country specific interventions addressing the issues identified by the phase one data, feasible within the time frame and resources available, were developed and implemented. In the final phase, again using a similar tool in each country, data collection aimed to assess if the interventions had made a measurable impact on maternal health services comparing pre-with post-intervention data. This is contrary to many traditional maternal health programmes, where internationally pre-defined common interventions are often applied in each country.
In sub-Saharan Africa, the excess burden of poor health is well documentedCitation1Citation2 and the magnitude of this excess is often described as most extreme in relation to indicators of maternal health and in particular maternal mortality.Citation3 The HIV epidemic has increased maternal and many other mortality rates; gains that were evident in health overall have now been lost.3 This has been especially so for infant mortality, life expectancy, and in general and maternal cause-specific death rates in hospitalised patients. However, the disparities in maternal health indicators predated the HIV epidemic. International interventions, such as the Safe Motherhood Initiative, did not have the intended impact.Citation4
Criticism of the Safe Motherhood Initiative, as became clear only later, included that interventions were not always evidence-basedCitation5 and these advances in knowledge have now been taken into account in later efforts to address maternal health.Citation6 Nevertheless, other criticisms remain of this and other internationally driven health interventions (e.g. antiretroviral treatment programmes). These include that such programmes take a “one-size-fits-all” approach and may not be locally appropriate. They often create vertical programmes that duplicate and work around existing health care systems. These vertical interventions may draw health workers towards the “flavour-of-the-month”, better-funded health interventions, rather than building the overall health system serving the multiple health needs in a particular country.Citation7 It has been increasingly identified that poorly functioning health care systems are a fundamental reason why greater gains in health have not been achieved in sub-Saharan Africa. The HIV epidemic has laid bare just how poorly these systems function. Improving health care systems is the current mantra.Citation8 What needs to be done is stated repeatedly; however, there is little said about how this may be achieved.
In this paper, the South African study is presented and discussed. The focus is on the programme-specific and more generic health systems interventions that were identified and their relative success.
South Africa is a country of almost 47 million people with a crude birth rate of 23 per 1,000 population, a total fertility rate of 2.7 children per woman and an estimated literacy rate of 84% and 81% for men and women, respectively.Citation9 19% of the adult population (older than 15 years) are estimated to be living with HIV, and the life expectancy of men and women is 50 and 52 years respectively.Citation9,10 Data from South Africa indicate that, in comparison to countries with similar levels of income, maternal (175–200 per 100,000) and perinatal (40 per 1,000) mortality rates are higher than one would expect, especially in a country where 92% of women attend antenatal care and 92% deliver in a medical facility.Citation11–13 Some of the explanation lies in the increasing HIV-related deaths. The top five causes of maternal mortality account for 87% of maternal deaths; non-pregnancy-related sepsis (mainly HIV) accounts for nearly 38% of the deaths.Citation11 The apartheid legacy of inequality, not only with regard to access to health care but also many other inequalities, explains some of this excess. For the 1998 South African Demographic and Health Survey, an asset survey was used to divide households into wealth quintiles and indicated that, while 14% of all births in the five years preceding the survey were delivered without the help of a medically trained attendant, 1.6% of these were in the wealthiest quintile compared to 30% in the poorest quintile.Citation14
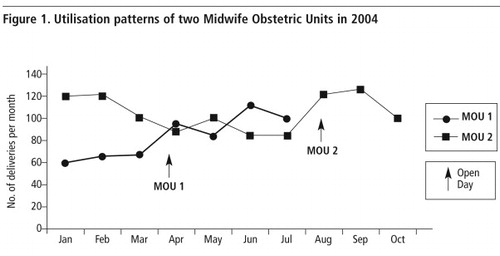
South Africa’s maternal health services are provided at various levels in the health care system. Antenatal clinics are widely distributed; some stand alone and some are within hospitals. Women can deliver at Midwife Obstetric Units (MOU), which provide a 24-hour service managed by midwives. In Gauteng, Midwife Obstetric Units are expected to perform 150 deliveries per month (Mr S Masilela, Director, Maternal & Child Health Unit, Gauteng Health Department. Personal communication, 2 July 2007). Level-1 (district) hospitals offer generalist care, level-2 (specialist care) and level-3 hospitals (sub-specialist care) provide referral cover and delivery services. Provincial departments of health measure their success through the achievement of national objectives, such as referring multiparous women with previously uncomplicated deliveries to lower levels of care for delivery.Citation15
Objectives
The overall objective of the study was to strengthen the health system in one sub-district in South Africa by working with local health care managers and providers. The specific objectives were to:
| • | assess and evaluate the quality of maternity care in a sub-district in South Africa, | ||||
| • | identify locally appropriate interventions to improve maternity care in this sub-district, | ||||
| • | prioritise and implement interventions through action plans developed jointly with local health managers, and | ||||
| • | evaluate the interventions. | ||||
Study site
A peri-urban district in Gauteng was identified by the provincial health managers. This sub-district, being poorer than other sub-districts, was anecdotally reported to have less well-functioning health services and included a number of informal and squatter settlements. At the time of this research project (2002-2004) there were few donor-funded research projects or programmes operating in this district. The district included 61 antenatal clinics, four Midwife Obstetric Units, one level-1 hospital and five level-2 hospitals. For this study we defined a single referral pathway and aimed to include all service points within that pathway. For the pre-intervention data collection, six antenatal clinics, one Midwife Obstetric Unit, one level-1 hospital and three level-2 hospitals were included. As there were so few deliveries in the one Midwife Obstetric Unit, all four Midwife Obstetric Units in the district were included, not only to get a larger sample but also to assess if the other Midwife Obstetric Units were under-utilised or not. During the study period, the district redefined its boundaries, which resulted in referral pathways that crossed boundaries. In addition, (numerator) data from certain clinics and hospitals were assigned to different service delivery areas and changes in the population served (denominator data) changed. The post-intervention data were gathered from the same referral pathway, which included the same six antenatal clinics, the same level-1 hospital but only two of the level-2 hospitals. At the end of the project our referral pathway was no longer consistent with the sub-district boundaries, nor was collated, pre-intervention, summary data totally comparable with the post-intervention period.
Methods
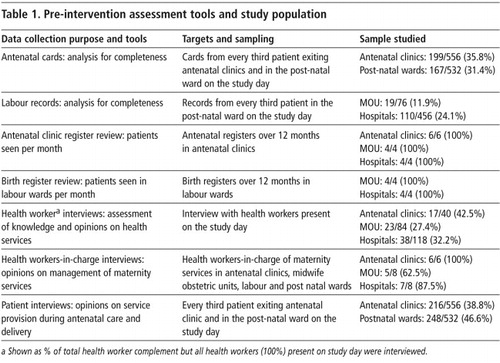
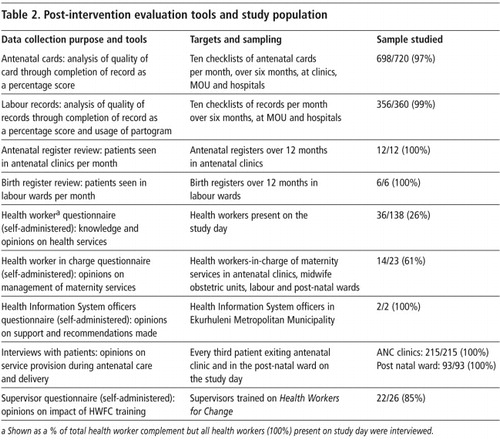
Data in phase one were collected using multiple methods and included interviews with health workers and patients, observation visits and patient record reviews. The impact of interventions was assessed using similar tools ( and ). In each facility, we attempted to interview all staff and reviewed all facility registers. A 30% systematic sample was used to review every third antenatal and delivery record and interview every third patient.
The quantitative and interview data were combined to describe how well the system functioned and were also used to assess the degree to which the district managed to achieve national objectives.
Various indicators were constructed to describe how well the services worked. Preventive care was considered to be done if syphilis screening results and tetanus toxoid were recorded on the antenatal records. Both of these also gave some indication of health system functioning, as it indicated that supplies (needles, syringes, drugs) were available and communications systems between antenatal clinics and laboratories were operational. Noting on the antenatal record that “a plan for delivery” was discussed with the patient indicated whether health workers understood that skilled care during delivery is important and that assisting patients in preparing for this is part of a quality service. The completion of partograms was used as a measure of the quality of intrapartum care. Other measures that were used included health workers’ knowledge on clinical care, and information from health workers and managers on supervision. The health information system data were reviewed to assess quality and utilisation. The proportions of each indicator were calculated and chi-squared tests were used to assess whether differences between the pre-and post-intervention data were statistically significant.
Results
In this section we describe the pre-intervention findings, the resultant interventions identified and the post-intervention findings. The pre-and post-intervention findings are, however, combined in the tables for ease of comparison.
Service quality
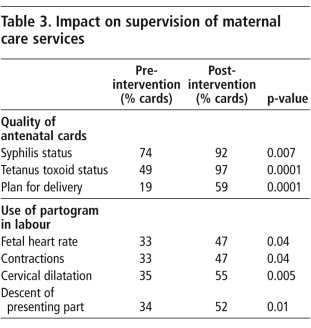
The pre-intervention findings indicated that most patients did have their syphilis status recorded, less than half had received a tetanus toxoid vaccination, and a plan for delivery was noted as having been discussed in fewer than 20% of patients. Partograms were routinely completed for less than one third of patients (Table 3).
Half of the facilities had had a supervisory visit related to maternity care in the last year. It was unclear who undertook the supervision, and only 17% of health workers in charge had documentation regarding these visits or could describe what happened during a supervisory visit. 33% of health workers interviewed had had a general supervisory visit in the last year, of which 59% were related to maternity care. Of those who had supervisory visits, 68% described them as useful. 63% of the health workers said that they had been praised for good work, compared to 74% who had been criticised for a mistake.
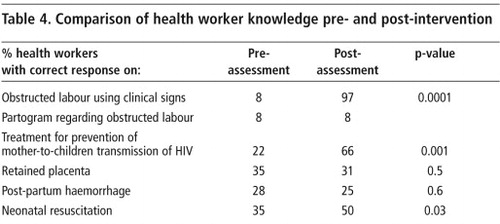
A series of questions were constructed to assess health workers’ knowledge: how well health workers could recognise obstructed labour (signs and symptoms) and how to read this off a partogram; their knowledge of how to provide treatment for prevention of mother-to-child transmission of HIV; how to treat retained placenta and post-partum haemorrhage; and how to resuscitate a neonate. Very few were able to demonstrate adequate levels of knowledge (Table 4).
A significant amount of routine data was being collected in the district, but the quality of the data was poor. Reviews of antenatal and birth registers identified many missing variables. These missing variables made comparisons between and within facilities practically impossible. The facility-level data were compared to the minimum data sets provided by the regional office of the Department of Health, and similar flaws were found. In addition, most data were not available to the people who needed it. At monthly maternal mortality meetings, while some data were presented, no trends were shown nor were data used to identify problems or improve performance.
Service use
The record reviews indicated that the Midwife Obstetric Units on average had 99 deliveries per month and hospitals 453. In the district as a whole, most of the Midwife Obstetric Units were falling short of the expected 150 deliveries per month. During the antenatal exit interviews, 65% of patients reported that they preferred to deliver in hospitals compared to 28% who preferred to deliver at a Midwife Obstetric Unit. The reasons cited were proximity to the hospital and a perception of better quality of care. Interviews with patients during the antenatal period indicated that health workers referred more patients for delivery to hospitals (49%) than Midwife Obstetric Units (18%). 24% of the patients referred did not know the reason why they were referred to a specific level of service, whether a Midwife Obstetric Unit or hospital.
Developing interventions
The findings were discussed with targeted district health workers in maternity services. Underlying causes for the issues identified were debated and ultimately five main interventions were prioritised:
| • | To improve the health system functioning and quality of interpersonal relations (between health workers and between health workers and patients) by using a WHO-tested interventionCitation16 developed in South Africa called Health Workers for Change. Citation17 | ||||
| • | To provide skills training, some of which was part of a national training agenda at the time, e.g. prevention of mother-to-child transmission of HIV and neonatal resuscitation. | ||||
| • | To improve the utilisation of Midwife Obstetric Units by holding “open days” to which the community would be invited and to reinforce health workers’ knowledge about Midwife Obstetric Unit referral criteria. | ||||
| • | To strengthen supervision at all facilities with an emphasis on the use of antenatal checklists and monitoring of labour using labour card checklists and partograms.Citation12 | ||||
| • | To strengthen the collection, analysis and utilisation of data for improving performance and decision-making, by identifying a key health information systems officer to work with maternal health care managers. | ||||
Most of the interventions were introduced at a workshop that included all Maternal and Child Health supervisors and managers based at facilities, district and regional offices, comprising provincial and local authority staff. Some of the interventions are described in detail elsewhere. Health Workers for Change is a workshop process described in other publications.Citation17 In this study, research staff trained facility and provincial health managers on how to run these workshops. Existing nationally-led prevention of mother-to-child transmission and neonatal resuscitation training was presented to workshop participants. The supervisory checklist for antenatal and intrapartum care is a tool developed elsewhere in South Africa but was not in use in this province at the time.Citation12 In this study, the researchers assisted managers in using the checklist, attended and participated in maternal and neonatal morbidity and mortality meetings, participated in supervisory meetings, assisted in collating data for these visits, and worked with the Health Information Systems Officer to collect and collate data. The local authority Health Information Systems Officer suggested various interventions. These were that a uniform minimum data set is used in all facilities, that health workers are trained on the usage of data and the consequences of poor data, and that trends in data be monitored over time so that progress could be measured. The Midwife Obstetric Unit open days were planned and run by the Midwife Obstetric Unit health workers with district management support. The members of the research team who were located in the district during this period played a mentoring role to district managers.
Impact
As illustrated in Table 4, there was a significant improvement in health workers’ knowledge post-intervention in identifying obstructed labour from clinical signs (p=0.001), prevention of mother-to-child transmission of HIV and neonatal resuscitation. Knowledge on use of partograms to identify obstructed labour was low in both the pre-and post-intervention data.
The Health Workers for Change intervention also had an impact. Some of the statements from the evaluation included “It improved communication between staff and patients”; “Staff have also changed towards their patients in that they are more sympathetic, especially to female patients”; “After the workshops there have been fewer patient complaints”; “Regarding staff attitudes towards their peers, some have changed for the better and some are more confident in challenging their colleagues who are performing poorly”. However, not all supervisors who were trained to and agreed to run workshops did it. Of the 28 supervisors who were trained, two left the district and only two ran workshops.
The post-intervention data showed improvements in record-keeping. Over 90% of antenatal cards recorded syphilis results; tetanus toxoid was given to almost every patient (97%) and three times more (59%) cards showed plans for delivery compared to pre-intervention levels (Table 3). While the increase in partogram use was statistically significant, more than 50% of the patient files still showed inadequate use of the partogram, and this is clinically not acceptable. It appears that the supervisory checklist, which aims to improve record-keeping as a proxy for improved care, did have some success. In addition, more health workers in the post-intervention phase had supervisory visits (33% pre vs. 67% post) and more health workers found these visits useful (68% vs. 97%, p=0.0001). This was important, as it probably indicated that supervisors were using these visits to be more proactive and constructive. At the end of the study period, the supervisory checklist was incorporated into the provincial Clinic Supervision Manual, which is a national managerial assessment tool.
shows the utilisation patterns of two Midwife Obstetric Units in the sub-district. Midwife Obstetric Unit 1 held an Open Day in April 2004 which resulted in an increase of approximately 90 deliveries per month. In Midwife Obstetric Unit 2, there was an initial increase in utilisation after the August 2004 Open Day, but it is not known if this was sustained. These open days may have changed community perceptions as advice on where to deliver had not changed. Women were still predominantly referred to hospitals (49% nurses referring to hospital vs. 16% to Midwife Obstetric Units) as was found in the pre-intervention phase.
The recommendations of the local health authority Health Information Systems Officer (that a uniform minimum data set is used in all facilities, that health workers are trained on the usage of data and the consequences of poor data, and that trends in data be monitored over time so that progress could be measured) were not adopted and no changes after the intervention were noted; data quality is still poor and data use inadequate.
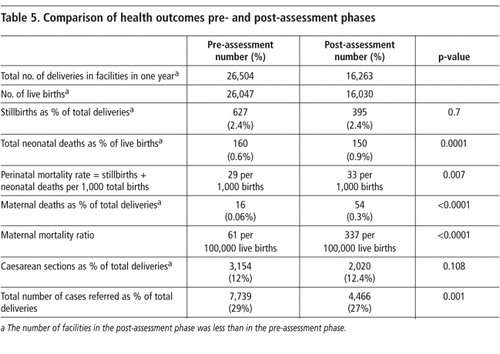
Given the short duration of this project, it was unlikely that outcome measures would have changed, and many factors that have an impact on maternal health outcomes were beyond the scope of this project. They are nonetheless presented in Table 5. These data were also drawn from provincial data. Because district boundaries were changed during the study period, it is not clear if numerator and denominator data were correctly allocated as the change was still new. Although these data should be treated with caution, they are not encouraging. Perhaps the most disturbing element is the sudden increase in maternal mortality in the post-intervention data. The problem was quickly identified and resources within this project were deployed to investigate. Poor patient management in one facility was identified and corrective measures were instituted. The other data indicate worse health outcomes or little change comparing the pre-and post-intervention data.
Discussion
This article describes operations research, a design that by definition may have to adapt to realities on the ground, e.g. in this study where district boundaries changed and the pre-and post-intervention data were not exactly comparable. The length of the study meant that being able to demonstrate an impact on health outcomes was very unlikely. Operations research is often vexed by such constraints, unlike traditional scientific research designs. However, the latter approach suffers from poor reproducibility of results once interventions are introduced in non-research settings. The motivation behind this design was to work with and in the usual health service without the related increased resources that often go with research interventions. This project sought to try and understand what is do-able in the real world of day-to-day health services and lessons learnt in that context. Further, the study was motivated by a desire to understand what is required to make health systems function better. There are many approaches to doing this and operations research can lead to some important insights.
The findings are equivocal. For example, programme-specific training (as in neonatal skills training or prevention of mother-to-child transmission of HIV) was easy to conduct, health workers attended and the knowledge base changed. Record-keeping improved as improved supervision contributed to this. However, there is no evidence to assert that improved records meant that services improved; they are only a proxy. While there was a definite improvement in partogram use, it was still at too low a level. It was also unclear if new knowledge was translated into action. This is consistent with other research on training for maternal care services.Citation18 In general, the interventions did not leave a significantly altered health system and we attempt to understand this.
The interventions can be divided into two types: programmatic interventions with a specific but narrow focus, such as the prevention of mother-to-child transmission of HIV and neonatal training, and systems level interventions, such as the Health Information Systems intervention, the Health Workers for Change workshops and the new supervisory methods introduced.
The programmatic interventions represent business as usual in this and many health systems. Training is a common intervention. It is routinely organised, people know the system and attend and they do learn.
The systems interventions were different in many respects. They were also less enthusiastically embraced and it is important to understand why. While all participants in the Health Workers for Change training agreed to run workshops, only a small minority did. In interrogating this, we look at the intervention itself and the people charged with implementing it. Health Workers for Change is a workshop process that demands that health care workers in managerial posts engage in problem-solving with other health workers. Consequent to the workshop processes, they need to set up systems that are more responsive to service needs (e.g. supply systems for drugs or equipment, supportive rather than punitive supervision, etc). At first glance these are not related directly to maternal health outcomes. It may be that potential benefits of addressing systems issues rather than programme issues are not considered beneficial to programmes and so are not prioritised. Maternal health managers may not see it as their job to get involved in systems issues. They may also have been uncomfortable with the workshop process itself as it is anti-hierarchical. This intervention is in every way not business as usual. Why then step out of the mould and take on new and what may be seen as additional work?
Managers who did not do it said they were too busy and did not get support from superiors. It is unlikely that those who did were less busy and there is no evidence that they got more support. They did appear to be more efficient and organised. It is worth reiterating that those who did run it found it beneficial for the maternal health services they supervise and that it did achieve some of their core programme-specific goals. So if it is worth doing, it is useful to postulate how else these managers differ from the majority, as this may inform further research. Some features of good management are that managers can organise and prioritise their time, and there is evidence of this as one factor differentiating these managers. Another feature may be people who are able to embrace and attempt new ideas, and that too differentiated the managers who did implement the workshops. Such managers do exist in the current health service. The question then becomes how to recognise, promote and reward them. A larger systems issue is how a large state bureaucracy can include a measure of initiative in performance appraisals. Can existing managers who do not display an appetite for innovation be coached or trained into new behaviours? What implications does this have for people running public sector management training courses? Is it possible to influence current training of new entrants into the public sector so that they have a new approach? In South Africa, this is currently predominantly nurses and thus a challenge to the South African Nursing Council, who oversee curricula.
Managers in this study who found the Health Workers for Change intervention useful may act as motivators of others who avoided it. For this to occur, existing senior staff members in the health service need to recognise this and create opportunities for such people with initiative to have influence.
The Health Information Systems intervention was also not easy to implement. One reason is that the role of a supervisor is not defined nor are the concomitant required skills. The baseline data indicated that supervision was unfocused, as evidenced by no one having documentation or being able to describe what was done at a supervisory visit. Supervisors and supervisees were unclear of the purpose of supervision. The supervisory checklist introduced is very clear and includes some guidance on how to collate data, but supervisors needed mentoring in order to use this checklist, and to get people to use it required constant reinforcing. However, this study showed that the knowledge required to collate and analyse data and, in particular, use data as a monitoring tool was largely absent. Using data for decision-making and management purposes is neither a generic skill nor an approach that people are comfortable with or competent in. This may explain why the intended contribution of the Health Information Systems officer never materialised. People who do not routinely use data may not appreciate the contribution that these officers can make. A new culture of monitoring and evaluation is required as these are core functional skills for health workers at every level. This should include routine self-evaluation as a standard at every level in the health service. Data should be used at the point of collection. This is an opportunity to build a learning organisation.
A second reason for the challenges the Health Information Systems intervention faced can be described as structural. This is a systems level issue, but health care workers are trained and work in a health care system where programme silos are the de facto building block of the health system. Programme managers are focussed on programme outcomes and measures. In most instances, district and programme managers do not have a routine way of working together and do not have common goals. This can be addressed in the way current services are organised, and some process for co-ordinating this at a senior level needs to be introduced.
There are other, more complicated structural problems that this study highlighted. In South Africa at the time of the study, and still today, services are overseen by different authorities. While the country nominally uses a district-based primary care model to organise services, in fact, the district health system, the basic building block of the health system, is still not functionally set up.Citation19 This may explain why the idea of a uniform set of maternal health indicators and training on their use suggested by the local authority Health Information Systems officer was never implemented in spite of a joint (province and local authority) working group agreeing to it. This is a very good example of how, if the health system itself is disorganised, it is very difficult to implement system-level initiatives.
This article began with the observation that in spite of high levels of antenatal clinic attendance and women having skilled attendants at delivery, we still have not brought down maternal mortality. It is perhaps easier to make a measurable impact on maternal health services when one starts from a very low base (low service use, very high maternal and neonatal mortality). This was certainly the case when the South African experience was compared to interventions possible in Cape Verde and Tanzania, where programme-specific interventions can make a huge difference. It is at the margins, when one is trying to have an impact in a relatively better-resourced environment, that different challenges exist and where we believe attention to systems issues are essential. A district-based system requires that a district manager oversees all aspects of the services and that programme-specific managers need to report to that district manager rather than to a higher level of programme manager. Further research could test if this would succeed. Opportunities for synergistic interventions between programmes may offer opportunities to improve programme-specific services.
In conclusion, we have focused our discussion on how to build the health system. We have identified the need to put in place systems that will develop a learning organisational culture. There is a need to move away from training that is technical in nature and only programme-specific. Interventions that are synergistic and affect more than one programme are required. Training should promote the ability to work as a problem-solving team. Data use and meetings where data are collated and reviewed at each service delivery point, at all levels of the health service, should be instituted. Senior managers need to champion people with drive and initiative who have been able to develop local solutions, so that they can act as role models. This needs to be done in a way that does not alienate others. This concurs with other work highlighting the need to transfer lessons and diffuse innovation in complex systems.Citation20Citation21
Other interventions suggested by this research talk to what can be called health systems structural changes. These include changing reporting lines between programme and district managers, co-ordination between different authorities within one district or province boundary, and changing the routine way people are assessed, appraised, promoted and rewarded.
The research has also identified a number of role players who can contribute to developing health systems, who are outside the health system. These include professional bodies who oversee training curricula, institutions which offer training, and institutions which provide funding for training and development nationally and internationally. This includes foundations, bilateral and multilateral agencies. International health bodies, whether they are focused on reproductive health, child health, HIV/AIDS, TB or chronic diseases, need to take on the challenge of health systems development and avoid promoting programme-specific interventions exclusively.
Lastly, this research has suggested some potential interventions that could be incorporated into a research agenda. If there is serious commitment to improving health systems, these kinds of interventions may be the ones that should be funded.
Acknowledgement
This research project was funded by the European Union as part of a joint multi-country study “Enhancing health system quality of care in pregnancy & childbirth based on locally generated evidence & adapted interventions” (Grant ICA4-CT-2001-10009).
References
- World Health Organization. World Health Report 2003: Shaping the Future. 2003; WHO: Geneva.
- World Health Organization. World Health Report 2004: Changing History. 2004; WHO: Geneva.
- World Health Organization. World Health Report 2005: Make Every Mother and Child Count. 2005; WHO: Geneva.
- D Maine, A Rosenfield. The Safe Motherhood Initiative: why has it stalled?. American Journal of Public Health. 89(4): 1999; 480.
- I Chalmers, M Enkin, M Keirse. Effective Care in Pregnancy and Childbirth. 1989; Oxford University Press: New York, 3–38.
- Effective Health Care Alliance Programme. Better Births Initiative. Liverpool School of Tropical Medicine. 29 September 2003. At: <www.liv.ac.uk/evidence/BBI/home.htm>. Accessed 2 July 2007
- Bill and Melinda Gates Foundation, McKinsey and Company. Global Health Partnerships: Assessing Country Consequences. 2005; McKinsey & Company: Florham ParkAt: <www.who.int/entity/healthsystems/gf16.pdf>. Accessed 11 May 2007
- World Health Organization. World Health Report 2006: Working Together for Health. 2006; WHO: Geneva.
- United Nations Children’s Fund. South Africa: Statistics. At: <www.unicef.org/infobycountry/southafrica_statistics.html>. Accessed 2 July 2007
- World Health Organization. World Health Statistics 2007. 2007; WHO: Geneva.
- RC Pattinson. Saving Mothers 2002-2004: Third Report on Confidential Enquiries into Maternal Deaths in South Africa. 2006; Government Printer: Pretoria.
- RC Pattinson. Saving Babies: A Perinatal Care Survey of South Africa 2000. 2000; Medical Research Council: Pretoria.
- South African Demographic and Health Survey 2003. Department of Health. <www.doh.gov.za/facts/sadhs2003/part1.pdf>. Accessed 2 July 2007
- South African Demographic Health Survey 1998. Department of Health. 1999; Government Printer: Pretoria.
- South African Department of Health. Guidelines for Maternity Care in South Africa: A Manual for Clinics, Community Health Centres and District Hospitals. 2nd edition, March. 2002
- C Vlassoff, S Fonn. Health Workers for Change as a health systems management and development tool. Health Policy and Planning. 16(Suppl.1): 2001; 47–52.
- S Fonn, M Xaba. Health Workers for Change. 1996; World Health Organization, Women’s Health Project: Geneva.
- E LeRoux, RC Pattinson, W Tsaku. Does successful completion of the Perinatal Education Programme result in improved obstetric practice?. South African Medical Journal. 88(2 Suppl.): 1998; 180–182.
- H Schneider, P Barron, S Fonn. The promise and the practice of transformation in South Africa’s health system. S Buhlungu, J Daniel, R Southall. State of the Nation South Africa 2007. 2006; Human Sciences Research Council: Cape Town, 289–311.
- H Schneider, D Blaauw, L Gilson. Health systems and access to antiretroviral drugs for HIV in southern Africa: service delivery and human resources challenges. Reproductive Health Matters. 14(27): 2006; 12–23.
- H Schneider, D Coetzee. Strengthening the health system and ensuring equity in the widescale implementation of an antiretroviral therapy programme in South Africa. South African Medical Journal. 93(10): 2003; 772–773.