Abstract
Antenatal Results and Choices (ARC) celebrates its 20th anniversary as a UK registered charity in 2008. ARC's remit is to provide information and non-directive support to parents before, during and after antenatal screening. Much of its core work is supporting parents who are considering or who have already undergone a termination after a diagnosis of fetal abnormality. This paper describes ARC's history and how its work has changed over the 20 years, and looks at terminations, mostly in the second trimester, in the UK from ARC's experience as a parent support organisation. It summarises the law on when terminations for fetal abnormality can be offered and explores some of the issues that have affected the parental experience of termination after an antenatal diagnosis. It describes how standards of care have changed for the better, partly due to the training and information they provide widely, and parents' experience and perspectives on the importance of having contact with others with the same experience.
Résumé
Enregistré comme organisme de bienfaisance de droit britannique, Antenatal Results and Choices (ARC) fête son vingtième anniversaire en 2008. Le mandat de l'ARC est d'informer les parents et de leur apporter un appui non directif avant, pendant et après le dépistage prénatal. Une bonne part de son travail est de soutenir les parents qui envisagent une interruption de grossesse ou l'ont déjà pratiquée après un diagnostic d'anomalie fłtale. Cet article décrit l'histoire de l'ARC et l'évolution de son travail depuis sa création. Il examine les avortements, en majorité du deuxième trimestre, au Royaume-Uni à partir de l'expérience de l'ARC comme organisation d'appui aux parents. Il résume la législation sur la période pendant laquelle les avortements pour anomalie fłtale peuvent être proposés et aborde des questions qui ont influencé l'expérience parentale de l'avortement après un diagnostic prénatal. Il montre comment les normes de soins ont changé en mieux, partiellement grâce à la formation et aux renseignements qu'ils fournissent largement, et il décrit l'expérience des parents et leurs points de vue sur l'importance des contacts avec d'autres personnes ayant vécu la même épreuve.
Resumen
Antenatal Results and Choices (ARC), celebra en 2008 su 20° aniversario como organización benéfica registrada en el Reino Unido. El cometido de ARC es proporcionar información y apoyo no directivo a los padres antes, durante y después de las pruebas prenatales. Gran parte de su trabajo principal es apoyar a los padres que están considerando o que ya han pasado por una interrupción después de un diagnóstico de anormalidad fetal. En este artículo se describe la historia de ARC y cómo su trabajo ha cambiado en los últimos 20 años, y se estudian casos de interrupción del embarazo, la mayoría en el segundo trimestre, en el Reino Unido, a partir de la experiencia de ARC como una organización de apoyo a los padres. Se resume la ley que dispone cuándo se puede efectuar la interrupción del embarazo en casos de anormalidad fetal, y se exploran algunos de los aspectos que han afectado la experiencia de los padres con la interrupción después de un diagnóstico prenatal. Se describe cómo los niveles de atención han mejorado, en parte debido a la capacitación e información que proporcionan ampliamente, así como la experiencia y los puntos de vista de los padres respecto a la importancia de tener contacto con otros con la misma experiencia.
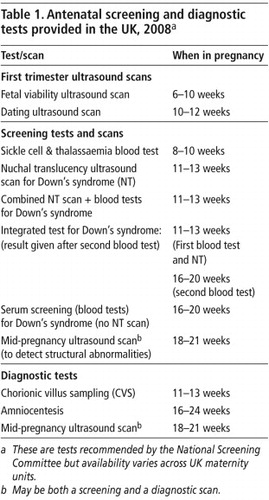
In the UK, the majority of women gain their maternity care through the National Health Service (NHS), and national antenatal screening policy is overseen by the UK National Screening Committee. All pregnant women are offered some kind of antenatal screening.Citation1 Table 1 shows the range of antenatal screening currently offered within the NHS.
Clause E in the abortion law in Britain (as amended in 1990)Citation2 Footnote* allows for termination of pregnancy on the grounds of fetal abnormality. Terminations are permitted at any time in pregnancy providing the following condition is met: “When there is substantial risk that if the child was born it would suffer from physical or mental abnormalities as to be seriously handicapped.”
In view of the way antenatal screening and testing is organised, most diagnoses are made in the second trimester. Fifty per cent of terminations performed under Clause E, according to the latest available data (2006), take place between 13 and 19 weeks,Citation3 and 35% at 20 weeks and beyond. National guidelines,Citation4Citation5 last updated in January 2008, encourage first trimester screening for haemoglobinopathies and Down's syndrome,Footnote† so the number of terminations at 12–14 weeks of gestation may increase. However, the major ultrasound scan to check for structural fetal anomalies is still carried out between 18 and 21 gestational weeks,Citation6 Footnote* so abnormalities will continue to be diagnosed well into the second trimester.
The Office of National Statistics for England and Wales quotes the number of terminations performed under Clause E in 2006 as 2,036,Citation3 or approximately 1% of the total number of terminations carried out in the two countries. This figure has been consistent over the years.
ARC's work
Antenatal Results and Choices (ARC) celebrates its 20th anniversary as a UK registered charity in 2008. ARC's remit is to provide information and non-directive support to parents before, during and after antenatal testing. Much of its core work is supporting parentsFootnote† who are considering or have undergone a termination after a diagnosis of fetal abnormality.
ARC began life within a different context of antenatal care and under a different name. The national charity was registered in 1988 as SATFA (Support after Termination for Abnormality). Antenatal screening for neural tube defects was available for many women at that time but most antenatal testing was comprised of the offer of diagnostic tests to women who were perceived to be “high risk”, either because of maternal age or family or obstetric history. The founders of SATFA were a group of bereaved parents and health professionals who recognised that the needs of those who had undergone a termination after an antenatal diagnosis were not being met. The conventional wisdom of the time was that women who had a termination in these circumstances had made a positive choice, would move on quickly and should focus on the next and hopefully successful pregnancy. This view determined how care was offered in hospitals. The rights and rituals afforded to other kinds of pregnancy loss, such as stillbirth, were not offered.
“You are the very person responsible for the loss; abortion implies the baby was unwanted. Rather than commiserating with your loss, people tend to say how lucky you were the abnormality was detected. With a stillbirth somehow it is acknowledged more – that a birth, labour and delivery has taken place… There are more likely to be painkillers available, photographs if wanted, registration of the stillbirth, provision of funeral if wanted… None of these exist for terminations; the baby has no identity as such, so it is difficult to mourn and grieve and come to terms with.” (Diagnosis of anencephaly at 22 weeks, SATFA newsletter, December 1985)
SATFA provided a helpline, established peer support groups for bereaved women and their partners, and worked closely with health professionals to improve care. ARC was fortunate in that one of its original founders was an “enlightened” health professional who saw the need for such an organisation. From the beginning, ARC has maintained an extremely close and supportive relationship with those working in the field. This has been instrumental in gaining widespread respect for the work that we do and in motivating health professionals to attend our training days and to refer parents to ARC.
The SATFA Handbook was first published in 1990 as a sensitively written guide to what the termination process may entail both physically and emotionally and to highlight the choices parents may have within the process. It was designed to be given as soon as possible after diagnosis to enable parents to prepare for what was ahead. Copies were sent to all UK maternity units. Partly because of this, SATFA became more widely known and more parents began to make contact before they had a procedure. They were often struggling to come to terms with the diagnosis and the onerous decision facing them.
“A choice sounded better than not having a choice. Yet, the idea of choosing was overwhelming and confusing. We were devastated at the thought of either course of action. It wasn't until much later that I realised the real tragedy was the loss of the healthy child and that I had not had a choice about it. The loss had to be accepted and mourned; and before that could take place we had to make an irreversible decision.” (Diagnosis of a chromosomal abnormality, SATFA News May 1991)
The organisation needed to reflect the shift in type of contact from people, so in 1992 the name became Support Around Termination for Abnormality. Then, as now, SATFA took a non-directive stance with the aim of helping parents to gather all the information they might need and to support them in working out the best way forward with the pregnancy in their individual circumstances. As the 1990s progressed and more women were offered antenatal screening tests, more of them began to contact SATFA while deciding whether to have screening or invasive diagnostic testing.
In 1998 there was a more substantial “rebranding” as the charity became Antenatal Results and Choices (ARC). The impetus for this major change was the increased volume of calls to the helpline regarding antenatal screening and diagnostic tests and the recognition that the needs of women who chose to continue pregnancies after an antenatal diagnosis were often neglected. There was some disquiet amongst our client group that by removing the reference to termination, ARC was tacitly colluding with the view that it was something to be ashamed of and so hidden away, not to be spoken about. They were reassured by the trustees that ARC would still actively raise awareness of the issues around termination, and that the name more accurately reflected its work. The truth is that although ARC provides support to parents whatever decision they make, most people who contact the organisation after a diagnosis are considering or have undergone a termination, while those continuing the pregnancy tend to veer towards condition-specific support groups.Footnote* It is likely that ARC will always provide most of its ongoing support to those who choose to end their pregnancies after an antenatal diagnosis as there is no other support organisation available to them.
ARC has continued to work closely with health care professionals and has developed a comprehensive training programme to help them promote the best standards of care to parents through antenatal testing and its aftermath. ARC also works at policy making level, sitting on a variety of antenatal screening subgroups of the UK National Screening Committee. This enables us to ensure that parents' perspectives influence the implementation and monitoring of screening programmes.
Factors affecting the offer of termination to parents after a diagnosis of fetal anomaly
The law allowing termination up to term should mean that parents can take the time they need to come to a decision about the future of what is most often a wanted pregnancy. Clause E does not list those conditions which would fit the criterion of “serious handicap”. It is left to clinicians (two are needed to sign the form) to take decisions on an individual case basis whether it is appropriate for the woman to have a termination. This has usually worked to the benefit of parents and their doctors, as each case can be considered with regard to the particular circumstances.
In reality, however, there can be time pressures associated with the legal limit for most abortions of 24 weeks. Research has suggested, and ARC has noted anecdotally, that there is variation in practice around the offer of post-24 week terminations for fetal abnormality, and that there has been an increase in professional caution in recent years. For example, some units will offer a termination after 24 weeks following a diagnosis of Down's syndrome, while others do not consider this lawful. Some fetal medicine units have now set up expert ethics panels to decide on the legality of post 24-week terminations.Citation7 A doctor interviewed as part of a study on attitudes to late terminations in fetal medicine units, by Statham et al,Citation8 noted the change in attitude.
“Whereas people used to say, yes, Down's is a permanent condition, you can have a termination after twenty-four weeks, [there are] lots of people now who say, well, maybe not… I think there's a climate change in society generally against them.” Citation8
Perhaps another explanation for shifts in practice in this area was the publicity generated in 2003 when the Reverend Joanna Jepson sought a judicial reviewCitation9 of the decision of the police not to prosecute doctors who terminated a pregnancy at more than 24 weeks' gestation where the fetus had been diagnosed with bilateral cleft lip and palate. The police authorities had undertaken an investigation of the case and were satisfied that the abortion was “legally justified and procedurally correctly carried out”. However, Rev Jepson challenged this decision on the basis that bi-lateral cleft lip and palate was not a “serious handicap” and therefore the abortion had been unlawful. After a detailed re-investigation it was re-affirmed in March 2005 that the doctors involved would not face prosecution. Although Jepson was unsuccessful, the media interest in the story was high and one of the doctors involved was named and pictured in a popular national daily newspaper.Citation10
Since Jepson, there have been other anti-abortion attempts to limit or ban these abortions. To generate interest, they suggest that parents are seeking perfection and aborting pregnancies in the second trimester and beyond when minor and rectifiable conditions are diagnosed. Conditions that have been highlighted in a number of stories in the British press include cleft lip and palate and talipes (club foot), on the basis that they can be successfully treated postnatally.Citation11 ARC's experience does not support the assertion that parents are seeking anything more sinister than a “healthy baby”. It is worth noting that the birth prevalence of talipes and cleft lip and palate in the UK is approximately 1 in 700 and 1 in 1000, respectively.Citation12Citation13 In other words, with an annual live birth rate of approximately 700,000, around 1,000 babies are born with clefts and about 700 with talipes each year. The vast majority of parents continue their pregnancy after a diagnosis of either condition.
What is often overlooked is that both conditions can sometimes be indicators of an underlying chromosomal or genetic syndrome, and there may be other what are called “soft markers” visible from scanning the fetus that are not listed as the reason for the termination, because they would not be considered structural abnormalities in themselves. Many syndromes cannot be diagnosed through amniocentesis, so some women may opt to end the pregnancy because of the significant risk of a serious problem.
Factors affecting parental decision-making
While technology may have moved on and shifts in professional attitudes taken place, what has not changed at all in 20 years is the emotional impact of the whole experience. We cannot underestimate the distress that is caused by an antenatal diagnosis and the subsequent decision-making process. However comprehensive the pre-test counselling and information may be, the news that there is something wrong with their unborn baby has a huge impact on women and their partners.Citation14
“My husband and I felt everything crumble around us in the face of that news. Convictions previously held and decisions previously made seemed superficial and hastily arrived at now that the reality of the situation was upon us.” (ARC News, April 2003)Footnote*
ARC has always maintained that if the process is handled well, extra distress can be avoided. It is essential that parents are given all the support and information they need in order to make the decision that is right for them. This will mean parents can look back and feel they were enabled to do the best they could in difficult circumstances. Crucial to achieving this is that the process is not routinised or assumptions made, as this may lead to parents feeling unsupported.
“It was the most difficult decision I have ever had to make and I feel the gravity and enormity of the responsibility was glossed over by one or two professionals… for us it wasn't an inevitable consequence. It was something we gave a lot of thought to, and a decision we both found very difficult. Whilst we don't regret the decision, we still regret aspects of the process of the decision.” (Mother of baby diagnosed with Down's syndrome, DIPEx interview no.AN02)
Those caring for parents given a diagnosis of fetal anomaly need first to acknowledge the shock and grief that sets in almost immediately and recognise that, in a state of emotional distress, parents are being asked to make a decision which they know will have long-term consequences for themselves and their family's well-being. A further compounding factor is that there is often very little definite information about the prognosis for the baby apart from when a lethal malformation is discovered (and even then, there can be uncertainty over when the baby's demise will actually take place). For example, there are excellent sources of information about what living with Down's syndrome might mean, but no one can tell parents the level of learning disability their child will experience. Other diagnoses may require parents to weigh up potential outcomes that feel equally painful to contemplate. It becomes an attempt to find the least worst outcome between equally nightmarish scenarios.
“But how, as… a human being you make those sorts of decisions, you know: ‘Do I stick a needle in my baby's heart and kill him now? Do I give birth to him and then sort of hope that he doesn't die, have a heart attack and drop dead at the age of five, you know? Or, if he survives it all, which is the best you can hope for, how will he live with the burden of this knowledge of this terrible incurable thing.’ …And I remember sort of going round in circles in my head between these things… And thinking, what am I going to choose, you know? Which of these three just awful, very different scenarios is the one that I feel I could live with, or that I could choose him to have to live with?” (Mother of baby diagnosed with congenital heart disease, DIPEx interview no. AN04)
There is little evidence on how parents actually make their decisions,Citation15 and the sensitivity of the situation means that research in this area will always be very limited. When talking through potential outcomes after a diagnosis of fetal abnormality on the ARC helpline or during face-to-face sessions, the factors parents bring to the decision have remained consistent over the years. They will most often include the perceived severity of the condition diagnosed, the predicted quality of life for the child and the impact of bringing up a child with special needs on the family, including existing and potential siblings. They may also be weighing up other factors such as their chosen lifestyle, work and financial situation. They may sometimes have particular religious, moral or cultural values that will play a part in their decision-making. They are always acutely aware that the decision they make will be something they have to be able to live with.
Within a UK setting, i.e. a National Health Service with many committed staff but all too often overstretched and under-resourced, it can be hard for parents facing these dilemmas to have all the time they need to discuss their options with caregivers. ARC encourages clinics to refer to us when appropriate, so that parents have a safe space and the time to explore their options with someone independent. Our contact details appear in the NHS antenatal screening information leaflet given to all pregnant women.
Evidence does not suggest that the type of procedure women have makes a difference to their long-term emotional recovery.Citation14 However, some women who have had an earlier diagnosis will put pressure on themselves to make a decision in time to have a surgical termination, as the idea of a medical induction comes as a shock to most. It can be understandably hard to contemplate labouring to deliver a dead baby. The ARC Parents Handbook provides information on all aspects of the termination process and gives women the chance to consider the advantages and disadvantages of the two types of procedure.Citation16
Standards of care for women having a termination for fetal abnormality
Although there is some variation in practice between NHS hospitals, most women will be offered a surgical termination before 13 weeks and a medical induction beyond this gestation. The Royal College of Obstetricians and Gynaecologists recommends that feticide is offered as part of the process for pregnancies from 21 weeks 6 days gestation onwards.Citation17Citation18 Feticide (most often an injection of potassium chloride into the fetal heart) is usually performed in a specialist tertiary unit. The termination itself will either take place on a maternity or gynaecology ward. In general, parents report better standards of care in the maternity setting. Some parents choose to use an independent abortion provider to obtain a surgical procedure post-13 weeks. All post-24-week terminations for abnormality are done by the NHS.
Twenty years ago, there was little or no specific care provision for women undergoing a termination after an antenatal diagnosis. Over SATFA/ARC's lifetime, thanks in no small part to its training for and work with health professionals, care for women and their partners undergoing termination has improved markedly. In the second trimester, most women are given a private room with facilities for the partner to stay and options regarding pain relief and ways to remember the baby if appropriate. There are usually discussions as to whether they want to see and hold the baby. Units will offer to take pictures of the baby and help with funeral arrangements if required. Today, we receive fewer accounts as desperate as the following:
“Here I was going through a termination when I could feel my babies moving, as if trying to tell me ‘Mammy I'm here, I'm alive, don't do this.’ This I found very difficult to cope with. My sons were delivered at lunchtime the following day within ten minutes of each other. I was told I wasn't to see them as it was thought that I would find it too distressing. Following a visit to theatre the next day for an evacuation, I was discharged home feeling guilty, depressed and totally useless – unfit to call myself a mother.” (Diagnosis of neural tube defects in both twins, SATFA News, February 1993)
Most parents who come to ARC report satisfaction with the way the process was handled:
“Throughout, we never felt pressurised into doing anything; we always felt that we had choices and that we were totally in control. There was no pressure or emotional blackmail at any stage from the initial phone call, to have the amniocentesis, or the termination, it was our decision. I cannot express how impressed with the sincerity, support, compassion and professionalism of all the staff involved in our baby's journey.” (Diagnosis of Down's syndrome, ARC News, March 2000)
High parental satisfaction with their care in hospital is supported by a major study into the psycho-social sequelae of antenatal diagnosis undertaken by Statham et al.Citation19
After the termination: the parental perspective
Over its 20 years, ARC has had contact with thousands of parents who have undergone a termination for abnormality. Most will need a period of grieving and adjustment to their loss, but from our experience we can say that the vast majority move on positively with their family lives. They come to recognise that they made the best decision they could in an extremely difficult situation.
“…as I read during the service about my experience of his birth and my uncertainty about whether I had done the right thing, my feelings felt clear. They were of sadness and loss; the taint of guilt seemed to have gone. It felt as if I had done my best, even if that was not very good.” (Father after termination due to severe heart defect)Citation20
Women are often anxious to recover physically so that they can start to think about trying to conceive again. It is not uncommon for post-delivery bleeding to continue for some weeks and this can be worrying, particularly if follow-up care is not in place. In ARC's experience, this is still patchy.
So what kind of support do parents seek from ARC after a termination? From an audit performed in 1998 and feedback gathered since, there seems to have been little change in what parents want from ARC although there has been a change over time in how this is delivered. When SATFA was founded in 1988, the support work was done by one part-time worker and a number of volunteers offering peer support and organising local support group meetings across the country. These well-attended informal meetings gave parents the opportunity to acknowledge their loss and share their experience with others who had undergone something similar. This was at a time when termination for abnormality was not considered as a significant bereavement, so some parents had been to groups for those who had experienced other kinds of pregnancy loss. While they appreciated the generic bereavement support, they were left with the feeling that having made the decision to bring about their baby's death made their experience different. Attendees at SATFA group meetings often mentioned the value to them of meeting others who had faced similar dilemmas and made similar decisions. They found it comforting to note that others in the group were people much like themselves who could empathise with and therefore normalise many of the intense emotions associated with their loss.
“I've come away feeling that I'm right to feel how I do, because so does everyone else. I'm not weak or dramatic or over-sensitive - I'm normal. This has been a tremendous boost for me.” (Evaluation form, ARC parents' meeting, Liverpool 2003)
Gradually, local support groups dwindled; parents still sought peer support but of a different type. SATFA trained volunteers to give individual support by telephone and arranged monthly regional parent meetings at different locations in the UK. In recent years the number of these meetings has reduced as more parents have opted for the anonymity of internet support. The ARC-moderated e-mail group, a listserve hosted by Yahoo, is heavily used, with nearly 500 members.
“By the fact that it is e-mail format, it allows me to express those feelings I have fought all day to suppress, at a time when I choose. It enables me to have time each day to think about my experiences, share them and think about what I have lost. I would say it has played an invaluable part in the grief process.” (E-mail to ARC, August 2005)
As well as the parent handbook, the other publication parents regularly point to as being especially helpful in their emotional recovery is our newsletter, ARC News. We send out three per year, and most of the content is taken up by parents' accounts of their personal experiences of termination. It also includes announcements of successful subsequent pregnancies. For those who find it difficult to speak to others about what has happened to them, reading stories that mirror their own is a way to break the feeling of isolation.
“We had a ceremony at the grave about four months after we lost our baby and our friends and family were very supportive of us… It was during this time that ARC came more into our lives. We read the newsletters when they arrived and discovered that there were many, many people like us. My wife used the support of the e-mail group and we knew there would be someone at the end of the phone if we needed them – I can't explain how important this was for us to know.” (ARC News, March 2007)
The majority of parents who contact ARC after a termination have always done so two to three months after the procedure. This often coincides with the original estimated date of delivery and pressure from friends/family or work colleagues to be “back to normal”.
“I felt like I should be getting back to normal by now and couldn't bear this sadness. I wished I could fast forward to a year's time and be through this pain. Thankfully, I phoned ARC. It was a relief to hear that they received many calls from mothers a couple of months after their termination and I was not being completely useless. It was good to talk to someone who had been through the same and fully understood my feelings… You have to act upon the information you have and the circumstances you are in and what is right for you and your family. I know we will get through this and I know we made the right decision.” (ARC News, October 2006)
Around 500 parents a year currently contact ARC after a termination for abnormality; they represent approximately a quarter of all those who go through the procedure. It remains a challenge for a small charity to ensure that parents are referred when necessary, but we would hope that thanks to ARC's work, the majority of those who do not make contact are receiving better care now than when we were starting out, and are enabled to come to terms with their experience.
Conclusion
As ARC enters its third decade, antenatal testing technology marches inexorably on. State of the art ultrasound machines provide ever-clearer images of a developing fetus and research is well underway into using fetal DNA in maternal blood to diagnose genetic conditions in the first trimester non-invasively. No matter how advanced and “safe” the testing technology, and no matter how good the care given to parents, the impact of a diagnosis of fetal abnormality at any time in a wanted pregnancy is devastating for those involved. The decision-making process is never entered into lightly, and whatever decision parents make they will live with the consequences. There will always be grief for the loss of the healthy baby they had been expecting, whatever decision they make. Inevitably, more abnormalities will be diagnosed antenatally, but the ability of clinicians to provide definitive prognoses or successful treatments cannot keep pace. So ARC will continue to be called upon to provide its specialised, independent information and individualised support to parents for whom results of an antenatal test lead to some of the most challenging decisions they will ever face. And ARC will go on collaborating with those involved in antenatal care to help them best meet parents' needs at this sensitive time.
Note
For further information on the work of ARC, see: <www.arc-org.uk>.
Notes
* The 1967 Abortion Act covers England, Scotland and Wales. Abortion is legal up to 24 weeks gestation only where continuing the pregnancy involves a greater risk to the physical and mental health of the woman or her existing children than if the pregnancy were terminated. Abortion is legal at any time if there is a risk to the life of the woman, risk of severe fetal abnormality or risk of grave physical or mental injury to the woman.Citation2
† “Review of the evidence presented and discussions from expert members of the Down's Syndrome Advisory Implementation Group have clearly shown that the way forward is introduction of first trimester screening.”Citation5
* The National Screening Committee Policy Position since July 2006 has been that aa providers must ensure they provide a dating scan and an 18–21 week anomaly ultrasound scan.Citation6
† Throughout the paper the terms “parents”, “baby” and “child” are used, as in ARC's experience this is how the majority of women and couples conceptualise themselves and the fetus within the context of a wanted pregnancy.
* In its early days, ARC worked closely with the Association for Spina Bifida and Hydrocephalus, for example, as they had contact with many women who had terminations after a diagnosis of neural tube defects. ARC also made contact with various bereavement support organisations.
* ARC News is a newsletter sent to 1,500 ARC members in the UK three times a year.
References
- Department of Health Chief Executive Bulletin. Issue 84 NHS Interest (4)14–20 September 2001.
- Abortion Act (1967) and Section 37, Human Fertilisation and Embryology Act (1990).
- Department of Health. Abortion Statistics, England and Wales: 2006. Bulletin No. 1, 2007.
- NHS Sickle Cell and Thalassaemia Programme. At: http://sct.screening.nhs.uk/antenatal.htm. Accessed 3 March 2008.
- Fetal Anomaly Screening Programme Director. Letter to Regional Antenatal Screening Co-ordinators. 10 May 2007.
- National Screening Committee Policy Position. July 2006. At: www.library.nhs.uk/screening/viewResource.aspx?mr=10&offset=10&catID=1328&resID=35693. Accessed 3 March 2008.
- UK Clinical Ethics Network. Clinical ethics committees. At: www.ethics-network.org.uk/committees. Accessed 3 May 2008.
- H Statham, W Solomou, J Green. Late termination of pregnancy: law, policy and decision making in four English fetal medicine units. BJOG: An International Journal of Obstetrics and Gynaecology. 113(12): 2006; 1402–1411.
- Jepson v. The Chief Constable of West Mercia [2003] EWHC 3318. From: Scott R. The uncertain scope of reproductive autonomy in preimplantation genetic diagnosis and selective abortion. Medical Law Review. 13: 2005; 291–327.
- J Mills. Doctor may be charged over late abortion. Daily Mail (London). 23 September. 2004
- L Rogers. Rules may have been twisted in abortion of cleft palate babies. Sunday Times (London). 11 July. 2004
- Cleft lip and palate. NHS Direct Health Encyclopedia. At: <www.nhsdirect.nhs.uk/articles/article.aspx?articleId=103. >. Accessed 3 March 2008.
- Talipes. NHS Direct Health Encyclopedia. At: <www.nhsdirect.nhs.uk/articles/article.aspx?articleId=104. >. Accessed 3 March 2008.
- H Statham. Prenatal diagnosis of fetal abnormality: the decision to terminate the pregnancy and the psychological consequences. Fetal and Maternal Medicine Review. 13: 2002; 213–247.
- TM Marteau, E Dormandy. Facilitating informed choice in prenatal testing: how well are we doing?. American Journal of Medical Genetics. 106: 2001; 185–190.
- ARC (Antenatal Results and Choices). A handbook to be given to parents when an abnormality is diagnosed in their unborn baby. 4th ed., 2007; ARC: London.
- Royal College of Obstetricians and Gynaecologists. Working Party Report:Termination of Pregnancy for Fetal Abnormality in England, Wales and Scotland. 1996; RCOG: London.
- Royal College of Obstetricians and Gynaecologists. Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths. 2001; RCOG: London. At: <www.rcog.org.uk/index.asp?PageID=549. >. Accessed 5 March 2008.
- H Statham, W Solomou, JM Green. When a baby has an abnormality: a study of parents' experiences. 2001; Centre for Family Research, University of Cambridge: Cambridge.
- A Don. Fathers Feel Too. 2005; Bosun Publishing on behalf of Sands (Stillbirth and Neonatal Death Charity): London.