Abstract
Cervical cancer is the most common reproductive cancer in women in Bangladesh, and most women come for diagnosis and treatment when it is too late. To support early detection of pre-cancerous conditions and prevent cervical cancer, Bangladesh undertook a screening programme using visual inspection of the cervix with acetic acid (VIA) and cryotherapy through a public sector programme. The programme was launched in 2004—05 in a phased manner, starting with a pilot programme in 16 of the 64 districts in the country and scaled up to 44 districts as of the end of 2007. Evaluation of the pilot programme’s performance showed that VIA can be carried out by trained doctors, nurses, and paramedical workers in Bangladesh, even though the level of resources is poor, and women, their partners and families are often not aware of the disease and its consequences. The programme now needs to move from opportunistic screening to population-based, systematic screening of women over age 30. More providers need to be trained, and clinics better equipped. The links between screening, diagnosis and treatment need to be improved and the false-positive rate of VIA tests greatly reduced. It is only when we have achieved high coverage that reduced rates of cancer can be ensured.
Résumé
Le cancer du col de l’utérus est la forme la plus fréquente de cancer de l’appareil génital féminin au Bangladesh, et la plupart des patientes se présentent pour un diagnostic et un traitement quand il est trop tard. Pour soutenir le dépistage précoce des lésions précancéreuses et prévenir la maladie, le Bangladesh a appliqué un plan de dépistage avec inspection visuelle après application d’acide acétique (VIA) et cryothérapie au moyen d’un programme du secteur public. Cette activité a été lancée progressivement en 2004–05, en commençant par un projet pilote dans 16 des 64 districts du pays, élargi fin 2007à 44 districts. L’évaluation des résultats du projet pilote a montré que la méthode VIA pouvait être utilisée par des médecins, des infirmières et des agents paramédicaux formés, même si le niveau de ressources est faible et que les femmes, leurs partenaires et leurs familles ignorent souvent tout de la maladie et de ses conséquences. Le programme doit maintenant passer d’un dépistage opportuniste à un dépistage systématique des femmes âgées de plus de 30 ans. Il faut former davantage de prestataires et mieux équiper les dispensaires. Les liens entre le dépistage, le diagnostic et le traitement doivent être resserrés et les taux de faux positifs des tests VIA nettement réduits. Seule une couverture élevée garantira une réduction des taux de cancer.
Resumen
El cáncer cervical es el cáncer reproductivo más común entre las mujeres de Bangladesh; la mayoría de las mujeres buscan un diagnóstico y tratamiento cuando ya es demasiado tarde. A fin de apoyar la detección temprana de condiciones pre-cancerosas y evitar el cáncer cervical, se inició en Bangladesh un programa de tamizaje en el sector público, que utiliza la inspección visual del cérvix con ácido acético (IVAA) y crioterapia. El programa se lanzó en 2004—05, en fases, empezando con un programa piloto en 16 de los 64 distritos del país, y se amplió a un total de 44 distritos para fines de 2007. La evaluación del desempeño del programa piloto mostró que la IVAA puede ser efectuada por médicos, enfermeras y trabajadores paramédicos capacitados en Bangladesh, aunque el nivel de recursos es deficiente, y las mujeres, sus parejas y familias generalmente no son conscientes de la enfermedad y sus consecuencias. El programa ahora debe hacer la transición de un tamizaje oportunista a un tamizaje sistemático de las mujeres mayores de 30 años. Es esencial capacitar a más prestadores de servicios y equipar mejor a las clínicas. Deben mejorarse los vínculos entre el tamizaje, el diagnóstico y el tratamiento y disminuirse considerablemente las tasas de resultados positivos falsos de las pruebas de IVAA. Sólo cuando se haya logrado una amplia cobertura podrán garantizarse tasas disminuidas del cáncer.
Visual inspection of the cervix with acetic acid (VIA), followed by treatment where necessary, aims to help women conquer cervical cancer through early detection and prevention. A number of studies have shown the advantages of VIA, including its low cost, simplicity of use, high sensitivity and instant results.Citation1–4 A study in Nigeria showed higher sensitivity of VIA (100%) than that of Pap smears (85.7%). The negative predictive value of VIA was 100%, while the positive predictive value was 20%. The sensitivity of VIA equalled the rates reported for Pap smears.Citation5 Bangladesh has an annual incidence of cervical cancer of 11,956;Citation6 and cervical cancer constitutes about 22–29% of all female cancers, according to hospital records.Citation7Citation8
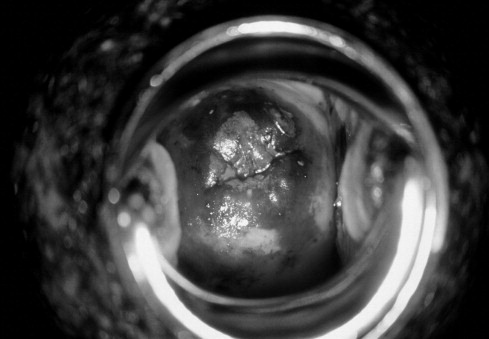
Cervical cancer is preventable if detected at an early stage. Studies in IndiaCitation9 and South AfricaCitation10 have shown that VIA is a very simple test. It needs minimum laboratory equipment and reagents, and paramedics can be trained to apply it. A VIA test uses a freshly prepared solution with 5% acetic acid (vinegar), which is applied to the cervix. When exposed to this solution for a few minutes, abnormal cells temporarily turn white and reveal aceto-white epithelium of the abnormal transformation zone. This test has been shown to be 90% effective in diagnosing pre-cancerous conditions of the cervix.Citation11
Cervical cancer is the most common cancer of the reproductive system in women in Bangladesh, and most women come for diagnosis and treatment when it is too late.Citation12 There was previously no programme for cervical screening. Cervical cancer was addressed in the same manner as other cancers, meaning there was only detection after onset and treatment through routine procedures. Cervical cancer was treated in public sector hospitals and in a limited number of private clinics.
The issue of doing something to prevent cervical cancer in Bangladesh was discussed in several meetings in 2003 between gynaecologists at the Bangabandhu Sheikh Mujib Medical University (BSMMU) and the United Nations Population Fund (UNFPA) Bangladesh. Since prevention using VIA is possible with minimum resources, BSMMU and UNFPA Bangladesh agreed to explore the possibilities of introducing it within the government health system. Subsequently, a meeting on cervical cancer screening was organised in 2003 with representatives from the government, non-governmental organisations and health professionals. VIA performed by field level health and family planning workers and paramedics was proposed as the method for cervical screening in the current socio-economic context of Bangladesh.
Pilot programme for VIA tests
A pilot programme was undertaken from August 2004 to December 2005 to assess the feasibility of training health workers and using this method within existing governmental infrastructure, with the support of UNFPA and BSMMU. The objectives of the pilot programme were:
| • | to train Government of Bangladesh service providers to perform VIA for cervical screening for early detection of cervical cancer and pre-cancerous conditions. | ||||
| • | to develop referral linkages to ensure follow-up and management of women with cervical intraepithelial neoplasia (CIN). | ||||
| • | to motivate other health personnel and communities to support the setting up of a cervical cancer screening programme. | ||||
Bangladesh has a well-established health infrastructure, with health and family planning facilities providing services from grassroots to tertiary level. The service centres are placed at different administrative tiers: national, district, upazilla (sub-district) and union. The Union Health and Family Welfare Centres in rural Bangladesh are at the lowest level of the health infrastructure, where basic health services are provided by paramedics called Family Welfare Visitors (female) and a Medical Assistant (male). Upazilla Health and Family Welfare Complexes (UHFWCs) are 31-bedded hospitals at the sub-district level, staffed with doctors and nurses. The Maternal and Child Welfare Centres (MCWCs) at district level provide maternal health care and reproductive health services. Two doctors and four Family Welfare Visitors who are trained in comprehensive emergency obstetrics care are responsible for providing reproductive health care to women. District hospitals have both outpatient and inpatient facilities, including obstetric and gynaecological patients. District hospitals have a consultant obstetrician–gynaecologist and several Medical Officers, supported by nurses, who provide services round the clock. BSMMU and 14 medical college hospitals function as tertiary-level referral centres.
The pilot programme was carried out in 16 of the 64 districts in the six divisions of the country, randomly selected from among districts with Maternal and Child Welfare Centres. As women needed to be referred to colposcopy clinics, more districts were selected from Dhaka and Chittagong division, which have more of these facilities. The pilot aimed to train manpower based in district hospitals and Maternal and Child Welfare Centres in VIA and to establish a system for cervical cancer screening as well as to create referral linkages to treatment facilities with a colposcopy clinic. The Department of Obstetrics and Gynaecology of BSMMU, with the help of other institutes and medical college hospitals, conducted a training course for master trainers in visual inspection. Twenty-five gynaecologists from BSMMU and other medical college hospitals were trained as Master Trainers.
The master trainers then trained senior staff nurses, paramedics and doctors based in the local and district health service centres. During the pilot phase, 113 service providers from the 16 selected districts were trained at BSMMU. These included one Medical Officer and two Family Welfare Visitors from each of the Maternal and Child Welfare Centres, one consultant or Medical Officer and two nurses from departments of obstetrics and gynaecology in the district hospitals, and one Family Welfare Visitor from each Upazilla Health & Family Welfare Centre in each of the 16 selected districts. These personnel were trained to use VIA to detect pre-cancerous conditions or evidence of cervical cancer among women patients, along with counselling, referral, follow-up and management of women.
The target group for cervical cancer screening were all ever-married women aged 30 years and above. Unmarried women were not included, because in the socio-cultural context of Bangladesh, unmarried women are not considered to have had sexual exposure and it would be socially unacceptable to examine them. Women were encouraged to attend their local Union Health and Family Welfare Centre, Maternal and Child Welfare Centre or the district hospital for a VIA test. Screening test positive women were referred to a tertiary hospital for colposcopy evaluation, and treatment was arranged as necessary.
BSMMU, Dhaka Medical College Hospital and Chittagong Medical College Hospital were recognised referral centres to receive screen-positive women from field level. In these centres, facilities for colposcopy, histopathology and management of CIN were available. The Department of Obstetrics and Gynaecology of BSMMU worked as the main co-ordinating centre in this programme.
Scaling up and implementation of the VIA programme
After completion of the pilot initiative, the programme was presented to the Ministry of Health and Family Welfare in 2005. Based on recommendations made at the presentation meeting, a study was conducted at the field level in six of the 16 pilot districts to assess the attitudes of women patients and of field level staff to the screening services. The findings were positive. The majority of the women interviewed at the service points (84%) showed an interest in availing the screening service. The service providers demonstrated a positive attitude (94%) and were willing to provide the service within the government health infrastructure. However, 30% of service providers called for improvements in infrastructure and clinic facilities and an increase in the number of trained staff, to share the increased workload. About 100–150 women attend the outpatient departments of district hospitals and Maternal and Child Welfare Centres every day. Even though it was difficult for only three trained service providers to do VIA as well as their other tasks, they did it willingly.
After dissemination of the findings on VIA performance, prepared by the screening centres, and the findings of the study on attitudes, the Government agreed to the expansion of the programme to the remaining ten pilot districts, and UNFPA Bangladesh included this programme in their annual country workplan for 2006–2010. At the same time, breast cancer screening by clinical breast examination was incorporated in the programme. Up to June 2008, facilities for cervical screening (and also for clinical breast examination) have been set up in 44 districts, and by the year 2010, all 64 districts in Bangladesh will have VIA centres.
Training and staffing
Trainee service providers spend 15 days at BSMMU learning VIA and colposcopy in small groups. This training is coordinated centrally by the Training Co-ordination Committee. A national curriculum, entitled Cervical and Breast Cancer Screening Programme: Standards and Guidelines, was developed and approved and is being used in the training programme. Following observation of 10–20 cases, at least 30 cases of VIA screening are done by each trainee during the training period. They also assist the master trainers by recording information in the registry book and counselling the women as well as doing visual inspections and coloposcopy examinations. Trainees are continuously monitored and evaluated during the practical sessions and advised how they can improve.
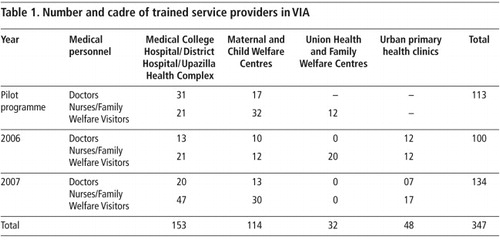
In 2006 and 2007, as part of the extension of the programme, 234 service providers were trained at BSMMU, in addition to the 113 who had been trained in the pilot phase (Table 1). The urban primary health clinics were also incorporated into the programme.
Renovation and equipment
Equipment required for VIA, and colposcopy and cryotherapy machines were procured to set up the screening centres and strengthen the referral hospitals. Acetic acid and other consumables were also supplied by the programme. Screening rooms were renovated and aseptic conditions were ensured.
Colposcopy training and development of colposcopy centres
To develop well-equipped referral centres (colposcopy clinics) in medical colleges, colposcopy training was provided to 37 gynaecologists in 2006–2007 at the colposcopy clinic of BSMMU. The participants came from several medical college hospitals and BSMMU. Resource persons for the training programme were from BSMMU, other medical colleges and from abroad (United Kingdom and India). The existing colposcopy clinics at BSMMU, the Sir Salimullah Medical College & Hospital in Dhaka, and the medical college hospitals in Chittagong, Rajshahi, Khulna and Mymensingh were all strengthened, with a view to providing a better service for the patients and develop referral centres nearer to home for VIA-positive patients.
Several master trainers also participated in a course on early detection and prevention of cervical cancer and screening programme implementation, jointly organised by the International Agency for Research on Cancer (IARC), Tata Memorial Centre Rural Cancer Project and Nargis Dutta Memorial Cancer Hospital at Barshi, Maharashtra, India.
Sensitisation workshop for stakeholders
After completion of training of intended staff in each district, an orientation meeting is held in the district to provide information to the community, the administration, social workers and other health care providers in the district about cervical cancer screening based on the VIA method.
Numbers of service points, and women screened and treated
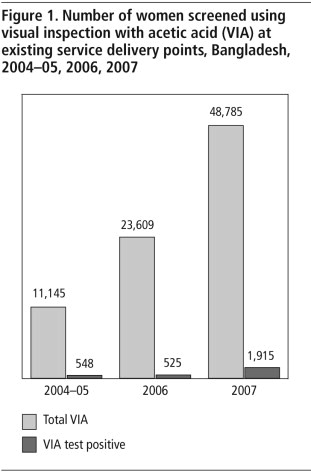
During the pilot phase, 32 service points in the 16 districts performed 11,145 VIA tests. Among them 548 (4.92%) women were VIA-positive. From January–December 2006, 21,609 VIA tests were done at service points in 22 districts. Among them 925 (4.28%) were VIA-positive. From January–December 2007, 107 service points in 34 districts performed 40,785 VIA tests. Among them, 1,918 women (4.70%) were VIA-positive ().Citation13 All the positive cases were referred to the colposcopy clinic of BSMMU or other government hospitals.
From 2005 to 2007, the colposcopy clinic of BSMMU received 1,547 women who were VIA-positive who had been referred there from 34 districts. The clinic evaluated these by colposcopy and cervical biopsy whenever indicated. Among the 1,547 referred cases, 763 (50%) had a diagnosis of normal, 422 (27%) had CIN stage I, 110 (7%) had CIN stage II or III, and 85 (5%) had cervical cancer. 167 (11%) women had unsatisfactory colposcopy findings ().
Management of CIN and cervical cancer
Women with CIN I were managed conservatively, as 70–80% of CIN cases revert to normal spontaneously. They were advised to come back after six months to a year for a repeat colposcopy examination. If the woman was more than 35 years old, a Loop Electro-surgical Excision Procedure (LEEP) was preferred. The women with CIN II and III were treated and followed up. In 2007, LEEP was done in 70 cases and cryotherapy in 15 cases of CIN I and CIN II. The women with early cervical cancer were managed in the gynaecological oncology unit of the same institute. There were 16 women with late stage cervical cancer who were managed in the gynaecological oncology unit of BSMMU, Dhaka Medical College Hospital, and National Institute of Cancer Research and Hospital.
Record-keeping
A general registry book for registration of all women having a VIA test has been developed. A red card is used to refer women with VIA-positive results from service points to referral centres. A blue card is given to women with VIA-negative results, who are advised to have a repeat VIA test after three years. A separate VIA-positive registry book has also been developed. These cards and registry books are already in use at VIA service points. In addition, a colposcopy registry book has been developed for recording colposcopy findings and type and outcome of management for women with VIA-positive results at referral centres (BSMMU and other medical college hospitals). Service providers have been supplied with reporting forms, and are asked to report monthly on all VIA tests performed in each centre.
Constraints faced during implementation
In the government medical college hospitals and the Maternal and Child Welfare centres, trained service providers were often transferred, thus depriving these centres of VIA-trained staff. To overcome this problem, more gynaecologists were trained in colposcopy.
Full facilities for LEEP and cryotherapy are available only at BSMMU. Equipment for carrying out LEEP is necessary in at least seven medical college colposcopy clinics, however. Equipment for cryotherapy was provided to BSMMU and two medical college colposcopy clinics. But more cryotherapy machines are also necessary and all referral centres should have facilities for both LEEP and cryotherapy.
Although the numbers of women screened has risen, utilisation of services by women who should be screened has been low at the screening centres, mainly because the centres are still using an opportunistic approach. That is, it is only women who have already come to a hospital or clinic outpatient department for other care who are advised to go for a VIA test. In any of the intervention districts in the country, there would be an average population of married women aged 30 and above of 360,000,Citation14 and all of them should be screened under this programme.
Monitoring and evaluation
Though the programme is being continuously monitored by BSMMU and government officials, still no monitoring system has been developed as yet. An evaluation of the programme was carried out in 2008 by a team of external reviewers. The reviewers assessed the cervical cancer screening programme up to 2007. The team selected four districts of three divisions of Bangladesh (Dhaka, Rajshahi and Khulna). They also evaluated the performance of BSMMU as the referral and treatment centre, as well as the national training and coordination centre.
Their report noted that at present the programme is largely based on opportunistic screening, though with good central coordination and some elements of organised screening. They recommended a broad-based public awareness campaign to increase uptake of services and improve the spontaneous participation rate, and a sensitisation campaign among other clinicians and paramedical staff to encourage them to disseminate knowledge and awareness of the programme in the community.
Colposcope image of a cervix stained with iodine showing possible dysplasia. The speculum is at the periphery.
The evaluation team found the structure and content of the training curriculum, course materials and handouts, and the competency-based evaluation system satisfactory for both training on VIA and colposcopy. However, they recommended shortening the course duration and decentralisation of the training programme. They also recommended screening only women who are 30 years old and above. They commented on the low VIA-positivity (below 3%) in some of the screening centres, and raised the concern that some cases were being missed. They advised creating better linkages between screening and treatment, and noted that many women are being lost after referral. They suggested that women patients and/or their relatives should be instructed to report back to the screening centre after colposcopy and/or treatment. Non-compliant patients could be contacted by telephone or with the help of field workers in the community. The referral centres should also generate a centre-wide list of patients seen by them and send the list to the respective screening centres on a quarterly basis, for cross-checking. The VIA-positive patients’ register maintained at the screening centre must then be updated using this list.
To improve compliance with treatment, the team advised following a “see-and-treat” policy, by carrying out treatment immediately after colposcopic confirmation of disease. They also recommended more use of cryotherapy, as it is a safe, low-cost and effective method of treatment for all grades of CIN. Each district should have a referral colposcopy centre with cryotherapy facilities. The team also suggested a unique registration number to be given to each woman at the screening centre using a district code/centre code/year/serial number, and to maintain a database in all the referral centres.
Discussion
The recommendations of the evaluation team now need to be carried out. As the scaling-up of the cervical screening programme proceeds, one of the most important next steps is to convert the programme from one based on opportunistic screening to one with population-based, organised, systematic screening that proactively ensures women attend. A public awareness campaign and sensitisation of clinicians and paramedical staff who are in a position to educate, encourage and refer women who should be screened, would be valuable.
As regards clinical care, we need to improve the links between screening, diagnosis and treatment and to fully equip our colposcopy clinics with approachable treatment facilities. VIA was developed in order to allow women to be screened and treated with cryotherapy, when appropriate, in one visit. The Bangladesh programme has not yet incorporated cryotherapy training and provision in this way, and needs to consider how and where this might be done.There are plans to promote cryotherapy in the future. The doctors have found this treatment to require less training and easy to use. The equipment is more affordable and could be maintained easily, and patients have less bleeding. In addition, the reasons for the high rate of false positive VIA tests (50%) and unsatisfactory colposcopy findings (11%) will need to be examined, and improvements made in the skills of providers. These improvements and integration of care will help to ensure better outcomes of the programme. Continuous proactive monitoring and appropriate corrective measures will ensure satisfactory performance and better utilisation of limited resources.
The greatest challenge will be increasing and maintaining the quality of the services. This means that ongoing training, supervision and monitoring are essential. However, with the reality of frequent transfers of staff, it may be impossible to retain staff in dedicated clinics for more than three years. The only solution is to continue training providers and setting up enough centres at the different levels of the health system, so that no matter where a woman is, the services will always be available to her.
Another challenge is in following up of referred cases. A system for community workers to be able to track patients from screening through diagnosis and treatment to ensure that they have the best possible outcome may need to be designed. Community sensitisation and provision of information to women about the importance of cervical screening is a commitment we need to fulfill; although VIA itself is a simple test and easy to explain, any follow-up diagnosis and treatment is not, especially for more advanced disease, and women need to understand this so that they will not be frightened off. It is only when the population recognises the importance of screening for all women over the age of 30 that high coverage and reduced rates of cancer can be ensured.
References
- A Goel, G Gandhi, S Batra. Visual inspection of the cervix with acetic acid for cervical intraepithelial lesions. International Journal of Gynecology and Obstetrics. 88: 2005; 25–30.
- OI Akinola, AO Fabamwo, YA Oshodi. Efficacy of visual inspection of the cervix using acetic acid in cervical cancer screening: a comparison with cervical cytology. Journal of Obstetrics and Gynaecology. 27(7): 2007; 703–705.
- V Singh, A Sehgal, A Parashari. Early detection of cervical cancer through acetic acid application – an aided visual inspection. Singapore Medical Journal. 42(8): 2001; 351–354.
- F Ghaemmaghami, N Behtash, MM Gilani. Visual inspection with acetic acid as a feasible screening test for cervical neoplasia in Iran. International Journal of Gynaecological Cancer. 14: 2003; 465–469.
- OI Akinola, AO Fabamwo, YA Oshodi. Efficacy of visual inspection of the cervix using acetic acid in cervical cancer screening: a comparison with cervical cytology. Journal of Obstetrics & Gynaecology. 27(7): 2007; 703–705.
- J Ferlay, F Bray, P Pisani. Cancer incidence, mortality and prevalence worldwide. J Ferlay. GLOBOCAN 2000. 2001; IARC Press: Lyon.
- PS Akhter, MM Uddin, SK Sharma. Patterns of malignant neoplasm: a three year study. Bangladesh Medical Journal. 27(2): 1998; 29–32.
- PS Akhter, MM Uddin, N Akhter. Gynaecological cancers – analysis of 1020 cases in three years. Journal of Teachers’ Association, Sher-e-Bangla Medical College Hospital, Bangladesh. 7(16): 1996; 439–445.
- N Bhatla, A Mukhopadhyay, S Joshi. Visual inspection for cervical cancer screening; evaluation by doctor versus paramedical worker. Indian Journal of Cancer. 41: 2004; 32–36.
- E Megevand, L Denny, K Dehaeck. Acetic acid visualization of the cervix: an alternative to cytologic screening. Obstetrics and Gynecology. 88(3): 1996; 383–386.
- R Sankaranarayanan, R Wesley, T Somanathan. Visual inspection of the uterine cervix after the application of acetic acid in the detection of cervical carcinoma and its precursors. Cancer. 83(10): 1998; 2150–2156.
- PS Akhter, MM Uddin, SK Sharma. Patterns of malignant neoplasm: a three year study. Bangladesh Medical Journal. 27(2): 1998; 29–32.
- Findings of Pilot (2004–05) and Extended Programme (2006–07) of Cervical and Breast Cancer Screening Programme, BSMMU.Reports 2006 and 2008.
- Bangladesh Bureau of Statistics. Bangladesh Population Census 2001 (Provisional). 2003; Dhaka: Government of Bangladesh.