Abstract
An assessment of abortion outcomes and costs to the health care system in Mexico City was conducted in 2005 at a mix of public and private facilities prior to the legalisation of abortion. Data were obtained from hospital staff, administrative records and patients. Direct cost estimates included personnel, drugs, disposable supplies, and medical equipment for inducing abortion or treating incomplete abortions and other complications. Indirect patient costs for travel, childcare and lost wages were also estimated. The average cost per abortion with dilatation and curettage was US $143. For manual vacuum aspiration it was US $111 in three public hospitals and US $53 at a private clinic. The average cost of medical abortion with misoprostol alone was US $79. The average cost of treating severe abortion complications at the public hospitals ranged from US $601 to over US $2,100. Increasing access to manual vacuum aspiration and early abortion with misoprostol could reduce government costs by 62%, with potential savings of up to US $1.6 million per year. Reducing complications by improving access to safe services in outpatient settings would further reduce the costs of abortion care, with significant benefits both to Mexico's health care system and women seeking abortion. Additional research is needed to explore whether cost savings have been realised post-legalisation.
Résumé
En 2005, avant la légalisation de l'avortement, on a évalué les résultats et le coût de l'avortement sur le système sanitaire à Mexico, dans des établissements publics et privés. Les données ont été obtenues auprès du personnel hospitalier et des patientes, et dans les dossiers administratifs. Les estimations directes des coûts incluaient le personnel, les médicaments, les consommables et l'équipement médical pour provoquer l'avortement ou traiter les avortements incomplets et d'autres complications. Les frais indirects de déplacement, de garde d'enfants et de perte de gain des patientes ont aussi été calculés. Le coût moyen par avortement avec dilatation et curetage était de $US143. Par aspiration manuelle, il était de $US 111 dans trois hôpitaux publics et $US 53 dans une clinique privée. Le coût moyen de l'avortement médicamenteux avec du misoprostol seul était de $US 79. En moyenne, le traitement des complications graves de l'avortement dans les hôpitaux publics allait de $US 601 à plus de $US 2100. Un accès élargi à l'aspiration manuelle et à l'avortement précoce au misoprostol permettrait de réduire de 62% les coûts gouvernementaux, avec des économies potentielles se chiffrant à $US 1,6 million par an. En réduisant les complications par l'amélioration de l'accès à des services ambulatoires sûrs, on diminuerait encore le coût des soins de l'avortement, avec de nets avantages pour le système de santé mexicain et les femmes souhaitant avorter. Il faut mener des recherches supplémentaires pour déterminer si des économies ont été réalisées après l'adoption de la légalisation.
Resumen
En 2005, antes de la legalización del aborto en el Distrito Federal de México, se realizó una evaluación del impacto y los costos del aborto en el sistema de salud del D.F., en diversos establecimientos públicos y privados. Se obtuvieron datos de personal hospitalario, registros administrativos y pacientes. Los cálculos de costos directos incluían personal, medicamentos, suministros desechables, y equipo médico para inducir el aborto o tratar abortos incompletos y otras complicaciones. También se calcularon los costos indirectos de las pacientes en viajes, cuido de niños y sueldos perdidos. El costo promedio por cada aborto con dilatación y curetaje fue de US $143. Para la aspiración manual endouterina (AMEU), fue de US $111 en tres hospitales públicos y US $53 en una clínica privada. El costo promedio del aborto inducido con misoprostol solo fue de US $79. El costo promedio de tratar las complicaciones graves del aborto en los hospitales públicos varió de US $601 a más de US $2,100. Al ampliar el acceso a la AMEU y al aborto precoz con misoprostol, se podrían disminuir los costos gubernamentales en un 62%, un posible ahorro de hasta US $1.6 millones al año. Al disminuir las complicaciones tras mejorar el acceso a los servicios seguros en ámbitos ambulatorios, disminuirían también los costos de la atención del aborto, lo cual sería un gran beneficio tanto para el sistema de salud de México como para las mujeres que buscan servicios de aborto. Aún se necesitan más investigaciones para explorar si se han logrado ahorros en costos post-legalización.
Until 2007, when first trimester abortion was legalised in Mexico City, abortion was legally restricted in Mexico. Even for legal indications, such as pregnancy resulting from rape or when the pregnancy threatened the woman's life, abortion services were rarely available because few states had established mechanisms by which women could seek care. In 2002 in Mexico City, the process to obtain a legal abortion following rape involved six steps at four different locations, and could take three months or longer.Citation1
Illegal abortion services were much more accessible than legal services, even if a woman might qualify for a legal abortion. Illegal abortion services by private providers are widely available in Mexico, especially in urban areas, and range from safe to unsafe. Poor women and women from rural areas suffer the consequences of unsafe abortion disproportionately.Citation2 Increasingly, women are using misoprostol obtained either from a provider or directly from a pharmacy or other drug seller in order to induce an abortion.Citation3–5 This is happening not only in Mexico but all over Latin America.
While efforts to improve access to safe abortion services in Mexico have been limited until recently, post-abortion care programmes using manual vacuum aspiration (MVA) to treat abortion complications have been extensively promoted.Citation6
Some data suggest that, at least for first trimester abortion, illegal services in Latin America may be safer than they were in the past. This has been documented in Brazil, where, as misoprostol use increased, a corresponding reduction in abortion-related complications was observed.Citation7 A recent review of death certificates in two districts in Mexico found no deaths that were suspected to be related to first trimester abortion procedures.Citation8 Another study on the incidence of abortion in Mexico found that the severity of abortion-related complications decreased between 1990 and 2006.Citation9
Although data exist on abortion-related morbidity and mortality, there has been relatively little research on the economic impact of unsafe abortion. In the area of post-abortion care, research in Brazil demonstrated the cost savings of introducing MVA in settings where dilatation and curettage (D&C) was the norm, especially when MVA is performed on an outpatient basis under local anaesthesia.Citation7 Similarly, a recent study from Nigeria found that out-of-pocket costs were higher for women who developed serious complications after an abortion outside of the hospital compared to those who had less severe or no complications.Citation10 Yet this study also reported that charges for D&C were only slightly higher than those for MVA,Citation8 even though outpatient MVA should be less costly than inpatient D&C.Citation6
The aim of this study was to estimate the costs incurred by the health care system associated with the treatment of incomplete abortion and other abortion complications due to unsafe abortion in Mexico City prior to reform of the abortion law. This includes the costs of surgical abortion (MVA and D&C) and medical abortion (MA) for incomplete abortion, as well as treatment of haemorrhage, sepsis, uterine perforation, cervical trauma and shock. More specifically, we compared the costs of treating incomplete abortion and other abortion complications in three hospitals in the public health system (as a proxy for costs associated with unsafe abortion) with the costs of performing safe abortions illegally in a private clinic.
Methodology
Study sites
The study was conducted between January and July 2005 in Mexico City. Cost and abortion outcome data were collected from a convenience sample of three public hospitals and one private clinic, representative of facilities providing abortion services to women. Hospital MX1, part of the Federal District Ministry of Health, was selected because it is one of two public hospitals in Mexico City that had implemented abortion services for the limited number of legal indications at the time of the study. Hospital MX2 is a large tertiary hospital within the Mexican Social Security System that serves non-governmental employees with low to moderate income levels. Hospital MX3 is a tertiary public hospital serving a low-income population without access to social security services and is part of the national Ministry of Health.
In all three public hospitals, women were generally seeking treatment for incomplete abortion; they reported to the emergency room and were then transferred to the gynaecology ward. Even though hospital MX1 was authorised to perform legal abortion for limited indications, very few legal abortions were performed. Both D&C and MVA were used in the gynaecology operating room. Most women attending the three hospitals did not require an overnight stay. They recuperated in a separate room on the gynaecology ward for 2–8 hours before leaving. The exception was in hospital MX3, where women having a D&C stayed for 24 hours. All three hospitals reported very few cases of severe post-abortion complications (other than incomplete abortion). However, women who did present with such complications were hospitalised.
Clinic MX4 is a private clinic that provided comprehensive reproductive health care for women, including safe but illegal induced abortions using MVA or MA. For women having MVA, in the first visit the doctor consulted with the patient and evaluated her for sexually transmitted infections. In the second visit, she received counselling, had the MVA and recuperated. A follow-up visit was scheduled two weeks later. Women who received misoprostol on the second visit took it at home and had a follow-up visit on the fifth day after taking the medication, to confirm completion of the abortion by ultrasound, with an additional follow-up visit two weeks later. Women over 14 weeks gestation were referred elsewhere.
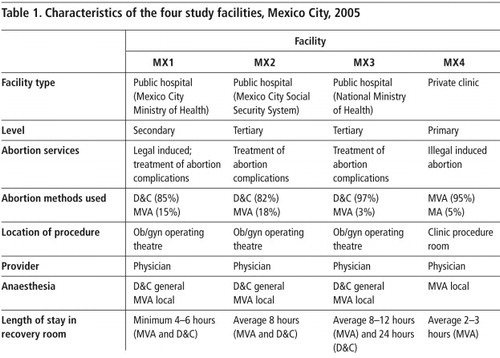
Table 1 summarises the characteristics of the study facilities. All three abortion methods were used across the four facilities, but to differing degrees. In the public hospitals, 82–97% of cases of treatment of incomplete abortion and the rare legal abortions were done using D&C; MVA was used less frequently. Medical management of incomplete abortion using misoprostol was not practised in these facilities. In the private facility, MVA was the only surgical technique, used in approximately 95% of cases, and in the remaining 5%, MA with misoprostol alone was used. In all study facilities, treatment was provided by at least one physician with a nurse present. Where D&C was performed, general anaesthesia was administered by an anaesthetist. In the three public hospitals, local anaesthesia was used with MVA, also administered by an anaesthetist. In the private clinic, only local anaesthesia was used and was administered by the physician performing the procedure.
Data collection and analysis
The cost estimates presented in this analysis represent the opportunity cost of all resources used in the treatment of incomplete abortion and other complications from the health system perspective. Cost data were collected using an ingredients-based costing methodology based on guidelines recommended by the World Health Organization.Citation11 The ingredients approach works from the specific abortion procedures (D&C, MVA and MA) and treatment protocols for septic shock, hypovolemic shock, infection and uterine laceration, and lists the various inputs required. Inputs here included type of personnel, drugs, consumable supplies, and medical instruments and equipment (hospital, surgical and imaging) used to induce abortion, or treat incomplete abortion or another abortion-related complication (Table 2 contains a list of typical inputs). The quantities and prices of inputs used were collected based on interviews with health care providers at each hospital and clinic. No observational data or individual patient records were used. However, whenever possible, a visual inspection of the surgical or procedure room was used to create an inventory of supplies and equipment for providing abortion and treatment of incomplete abortion and other complications. Supplementary budgetary data and expenditure records were used to gather information on salaries and indirect facility overhead costs. Lastly, the indirect costs of patient travel, childcare and reported lost wages were also collected in an effort to capture women's non-medical expenses. This study was not able to capture the costs associated with the initial interventions by women that led to incomplete abortion. All costs were in Mexican pesos and were converted to US dollars (USD) using the exchange rate of US $1=11 pesos valid in 2005.
A more detailed description of how each cost component was estimated is available from the authors. Here we briefly describe the estimation of personnel costs, drugs and disposable supply costs, medical instrumentation and equipment, and operational costs. Staff costs included the service time of doctors and nurses in the direct provision of care before, during and after inducing an abortion, treating an incomplete abortion and/or treating a complication. Indirect time spent by other staff serving patients was also included; the percentage of indirect support staff time spent was estimated by hospital personnel. The quantity and price of drugs for abortion services were collected from each hospital or clinic for analgesics, antibiotics and anaesthetics (local and general). Additional types of drugs, including uterotonics, oxygen and other emergency medications used for the treatment of abortion complications, such as septic shock, hypovolemic shock, infections and repair of uterine perforation, were estimated separately. Cost information was obtained from hospital pharmacies, clinic invoices, and central stores in Mexico City or the national Ministry of Health, depending on the facility.
Costs for laboratory tests for abortion complications were obtained from hospital user fee lists, showing what patients would pay. It was considered too difficult to use micro-costing methods to obtain costs for laboratory personnel, supplies and equipment in the large public hospitals in Mexico City. The annual costs of medical instruments and equipment were calculated using reported useful years of life for capital goods and a depreciation rate of 3% on instruments and equipment. The total annualised cost of medical instruments and equipment per woman treated was estimated separately for each type of abortion procedure (D&C, MVA and MA) and for each type of abortion complication.
Facility operating costs were estimated either from hospital administrative records, where easily available, or from published or available hospitalisation cost estimates obtained from the Mexico City or the national Ministry of Health central records. Hospitalisation costs were adjusted by subtracting the share of costs attributable to personnel, drugs and supplies used to provide abortion services to estimate a proxy for operating expenses. Hospitalisation costs were adjusted to cover operating expenses only and pro-rated for the patient's length of stay at each hospital, depending on the service.
Health workers administered a brief questionnaire to women seeking reproductive health services at each facility to estimate the average transport cost, childcare cost and lost wages associated with a general visit, family planning services and abortion care. The data presented primarily capture their transportation and child care costs. Most women did not report an amount for the wages lost but did indicate that they missed work for their hospital or clinic visit. An average of 33% of the women interviewed (n=75) in all the facilities said that they had missed all or part of a day of work to receive treatment. It was beyond the scope of this project to estimate the lost wages from women who did report missing a day of work but did not specify an amount. A proxy of the average daily wage across all women who reported missing work is used in this analysis, which is likely to underestimate the actual lost income. The estimate covers all visits to receive treatment, including follow-up visits.
The total costs are presented as a total (direct and indirect) cost per woman having an abortion, receiving post-abortion care using D&C, MVA or MA, and any additional costs for the treatment of complications and required hospitalisation. These costs are the sum of labour, drugs and disposable supplies, medical instruments, equipment, operating expenses and patient costs.
Data on the treatment of incomplete abortions and induced abortions were collected directly from hospital records or interviews with medical personnel, where available. It was more difficult to obtain information on the number of other more severe abortion-related complications. All three public hospitals reported very low rates of severe abortion-related complications. Because of the difficulty in obtaining complete information on complication rates for the sample hospitals, the analysis uses data on complication rates for the Mexico City and national Ministry of Health hospitals and both types of social security hospitals.Citation12–14 Sensitivity analysis varied the complication rate to estimate a range of plausible costs.
In order to estimate the potential impact of legalising safe abortion, the analysis estimated the total costs associated with scenarios that assume legal access, as well as increased access to MVA and MA services for early abortion.
Results
Health outcomes
Each of the public health facilities in this study performed approximately 600 to 1,400 abortions annually for the years 2004 and 2005, for a total of 3,945 cases. The great majority (over 95%) were for treatment of incomplete abortion. The private clinic providing safe but illegal abortions performed an average of 720 abortions per year, based on 2004 and 2005 patient visits, using MVA and to a limited extent MA. All four facilities reported very low rates of serious abortion-related complications or had incomplete data.
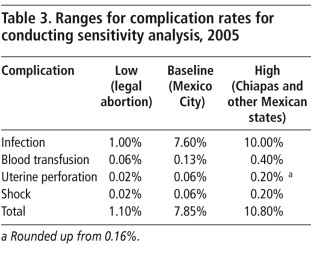
Table 3 shows the complication rates used in the sensitivity analysis that would be expected if abortion were legally available in all settings. According to the available data for Mexico City, of all the women who presented at hospitals for treatment after an abortion (14,163 total cases), 92.20% were treated for incomplete abortion, 7.69% required treatment for infection, and 0.06% required repair of a uterine perforation.Citation12 We were unable to obtain direct information about blood transfusion. Hospital discharge data indicated that 1.29% of women presenting for abortion-related care were diagnosed with haemorrhage,Citation12 and we estimated that 10% of them required a blood transfusion. We therefore estimated that 0.13% of women presenting for treatment after abortion required a blood transfusion. The complication rates listed for the “low” scenario in Table 3 are similar to those reported in settings where abortion is safe and legal.Citation14Citation15 Estimates for the “high” complication-rate scenario are based on hospital discharge data indicating a higher incidence of severe complications, taken from other states in Mexico as compared to Mexico City. For example, in Chiapas, one of the poorest states in Mexico, the reported incidence of uterine perforation is at least 0.16%, or more than double that of Mexico City.Citation12 This was rounded up to 0.20% in the table.
Cost of treating incomplete abortion and/or induced abortion
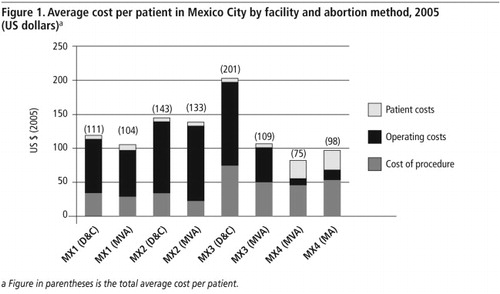
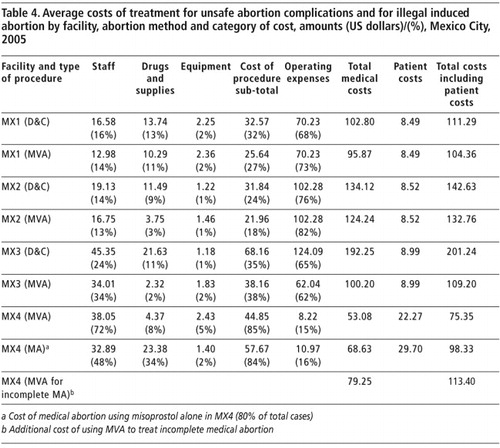
and Table 4 present data on the average cost of post-abortion care or inducing abortion for the three types of abortion procedure (D&C, MVA and MA) at the four study sites in Mexico City. Cost estimates are presented with and without patient costs. The total cost per patient was highest in the two largest public hospitals (MX3 and MX2), located in the more central parts of Mexico City and serving the largest number of patients. The cost of providing abortion was lowest in the private clinic providing safe but illegal induced abortion, using MVA and MA. In the private clinic, the total cost per patient of providing MVA, excluding patient costs, was US $53, almost 60% of the average cost of MVA (US $93) used to treat incomplete abortion in the three public hospitals. MVA cost less than D&C. The total cost of treating an incomplete abortion with D&C ranged from US $103 to US $192 in the three hospitals. MVA was slightly lower, ranging from US $96 to US $124. At the private clinic, the cost of providing MA was slightly more expensive than MVA, but both methods were significantly less costly compared to the treatment of incomplete abortion in the public hospitals.
Cost profiles
The variation in costs across facilities is shown in the breakdown of costs by category in Table 4. The general allocation of total costs to staff time, drugs and supplies, and equipment was similar across the three public hospitals. Operating expenses were the largest contributor to average cost per patient, followed by labour costs, drugs and supplies, and lastly, equipment. Among the direct service-related expenses, personnel time was the largest cost item across all four facilities. In each public hospital setting, average staff costs per patient were lower for MVA compared to D&C. In the private clinic, staff costs for MVA were higher than for MA, accounting for 85% to 94% of direct input costs, respectively. However, drugs accounted for 34% of total costs for the provision of medical abortion, due to the high cost of misoprostol tablets in Mexico. In the hospital settings, the share of costs for drugs and supplies used for D&C and MVA was between 2% and 13%, and was generally lower for MVA, which requires only local anaesthesia. The share of total costs for equipment was slightly higher for MVA, reflecting the need to purchase MVA cannulas and syringes.
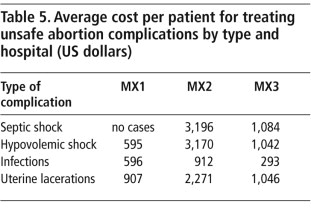
Cost of treating abortion complications
We estimated the average cost per woman treated by complication type for each public hospital, shown in Table 5. Costs of treating complications were in addition to initial costs of treating an incomplete abortion. On average, infection was the least costly to treat, although it was the most prevalent complication. Treatment costs on average were: septic shock (US $2,140), hypovolemic shock (including blood transfusion) (US $1,602), mild to moderate sepsis (US $601), and repair of uterine perforation (US $1,408). The Mexico City public hospital (MX1) had the lowest average treatment costs for shock (US $595), infections (US $596) and uterine perforation (US $907). Average costs were highest at the Mexico City Social Security System public hospital (MX2) for treating shock (US $3,170), infections (US $912) and uterine perforation (US $2,270). These costs included hospitalisation for inpatient care, some 4–7 days for shock, 2–3 days for infection, and 4–10 days for repair of uterine perforation.
Costs of unsafe vs. safe abortion
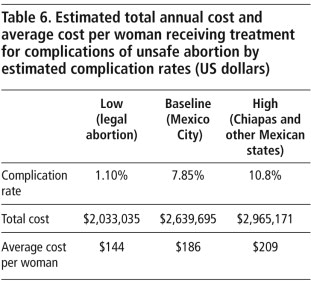
To estimate the total cost of treating incomplete abortion, including costs associated with treating more severe abortion complications, we used 7.9% as the estimate for the 2005 baseline rate of more severe abortion complications, associated with legally restricted access. This gave a total cost of US $2.6 million to treat all complications related to unsafe abortion for one year for Mexico City, or an average cost per woman treated of US $186. Assuming a high rate of complications from unsafe abortion, as pertains in the poorest parts of Mexico, with 11% of women experiencing more severe complications, the cost to the government of treating all abortion-related complications would reach US $2.9 million or $209 per woman treated. In contrast, if a low complication rate associated with legal abortion is assumed, the total complication rate would be an estimated 1.1%, and the total cost for treating abortion-related complications would be US $2 million, or an average cost per woman treated of US $144 (see Table 6).
These estimates show that modest cost savings would be achievable if efforts were made to reduce complications associated with unsafe abortion. For instance, reducing the rate of more severe complications from 7.9% to 1.1% by making safe and legal abortion more broadly available could save US $43 per woman treated, or over US $600,000 per year for the government of Mexico City. Similarly, a reduction of complication rates from 11% to 1.1% would lead to savings of US $65 per woman or a total of close to US $1 million annually.
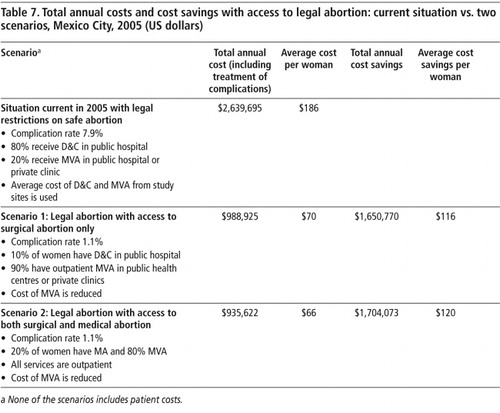
Even greater savings would be possible, however, if lower-cost methods for treating incomplete abortions were introduced, alongside increased access to safe and legal abortions. We explored the potential savings for the government of this change through two scenarios. Table 7 presents a summary of the differences in the cost of abortions for Mexico City for the situation current in 2005 (baseline) and for two different scenarios that increase access to safe, legal abortions.
In Scenario 1, we assumed that 10% of all abortion patients were still receiving treatment from public hospitals using D&C at the same average cost as in the current or baseline situation, at US $143. In Scenarios 1 and 2, an average cost of US $53 was used for providing MVA in non-hospital settings, based on the cost of providing services in the private clinic MX4. In Scenario 2, a cost of US $79 was used for MA, also based on estimates from MX4 (see Table 4).
Table 7 presents the total costs and cost savings associated with increasing access to safe and simpler methods of abortion for Mexico City. In Scenario 1, increasing access to legal and safe abortion using primarily MVA would reduce costs to the government by 62%, with a potential savings of up to US $1.6 million. In Scenario 2, even a modest increase in access to MA would provide additional cost savings of over US $50,000. Key to these scenarios is that the cost of providing abortion services declines as access increases at smaller public and private health facilities, which can provide abortion care efficiently and at less cost than large hospitals.
Discussion
This study demonstrates that unsafe abortion is costly to the Mexican health system for a number of reasons, both health-related and economic, and that significant cost savings per woman can be realised through increasing access to safe abortion services. Complications after unsafe abortion are more common in legally restricted settings,Citation15Citation16 and treatment for them is expensive, especially serious complications for which prolonged hospitalisation is required. However, at the time this study was done, prior to abortion law reform in Mexico City, health facilities were reporting many incomplete abortions but few other post-abortion complications. This may be because women and providers were increasingly using medications such as misoprostol to induce abortion or because clandestine providers might have begun using MVA more frequently instead of dangerous invasive techniques. Widespread antibiotic prophylaxis has also been cited as a reason for a reduction in morbidity and mortality associated with unsafe abortion in Latin American settings.Citation2
Despite the apparent reduction in morbidity in recent years, the incidence of complications reported in the hospital discharge data is still much higher than that reported in settings where abortion is safe and legal, and we have demonstrated significant cost savings to the health system in Mexico City if complications are reduced even further. Even small reductions in the incidence of serious complications has an important impact on cost, as well as women's health. Because the incidence of complications is higher in other parts of Mexico, savings would also likely be higher. In addition, the published data on the incidence of abortion complications reflect reported cases only and likely underestimate the total costs and health burden for women seeking abortions outside the national health system.
In Mexico City, at the time these data were collected, D&C was the preferred method of treating incomplete abortion. D&C is more costly than MVA because general anaesthesia in an inpatient setting is required. In addition to the expense, D&C is no longer recommended by the World Health Organization unless MVA is not available because D&C has a higher complication rate.Citation16Citation17 In two of the three public hospitals we studied, when MVA was provided, women were often made to stay in a recovery area as long as women who underwent D&C, even though MVA was provided with local anaesthesia. In hospital MX3, where the average recovery time was shorter after MVA, the costs were significantly less than for D&C. Our data suggest that treatment of incomplete abortion could be provided through a less costly model that relies on MVA under local anaesthesia in an outpatient setting, combined with a shorter recovery period.
Our findings regarding cost differences between D&C and MVA are consistent with findings from other studies conducted in Mexico and Latin America, where the cost of providing MVA through ambulatory services was 30–70% lower than the cost of providing D&C through inpatient services.Citation17 Also consistent with other studies in Latin America,Citation6 our findings suggest that improvements in service delivery and increased access to abortion services using MVA can translate into potential cost savings.
Differences in the costs across methods alone were less pronounced than differences in costs of the different methods related to where treatment was delivered. Excluding operating expenses across the three public hospitals and focusing only on the direct inputs of staff time, drugs, supplies and equipment used to provide abortion services, personnel time was the largest cost item across all four facilities. The variation in costs is explained by the choice of procedure, average length of stay and personnel costs associated with the provision of care. In general, average staff costs per patient were lower for MVA compared to D&C. In the two larger hospitals (MX2 and MX3), personnel costs were higher than in the smaller secondary hospital (MX1) due to both higher salaries and greater use of labour resources in the provision of abortion care.
When the recovery times were equal, there were only marginal differences between D&C and MVA in the public hospitals because of the higher inpatient overhead costs regardless of which method was used. However, the cost of providing MVA in the outpatient clinic setting was 40–50% less than the cost of providing either MVA or D&C in the hospital. The reduction in cost is explained by differences in costs associated with local anaesthesia, lower operating expenses and less personnel time required for post-operative care. Furthermore, the resources used to treat incomplete abortions in a large hospital would be better used to improve maternity care and other critical obstetric and gynaecological care,Citation18 while moving abortion services to smaller facilities and/or primary care settings.
In the private clinic providing safe abortion, the cost of MA was somewhat higher than MVA, especially when women's transportation costs were included. This cost differential was largely due to the additional follow-up visit that was required with MA. A previous study in a Latin American country where abortion was illegal documented a similar MA protocol involving two follow-up visits; providers seemed particularly eager to ensure that women had a complete abortion as soon as possible,Citation19 likely because of the fear that women might seek care at a different clinic if they had prolonged bleeding or other unexpected symptoms. Only one follow-up visit is the norm in settings where the method is approved. Under a more liberal abortion law, providers are likely to feel more comfortable following evidence-based protocols with only two visits to provide MA,Citation20 reducing the associated costs. In addition, the cost of misoprostol has risen rapidly throughout Latin America in recent years, possibly related to the high demand on the black market.Citation5 With legalisation and the appearance of generic products, this likely would fall.
This study has several limitations. First, since it focused on the costs of treating unsafe abortion from the perspective of the health system, we were unable to capture the cost of women's time waiting for treatment in the three hospital settings, the cost of the initial intervention that led to an incomplete abortion, the cost of any abortifacient medication purchased, payment to a provider who supplied pills or carried out a surgical or other procedure, transportation costs, childcare costs or cost of days lost from work due to complications but prior to treatment.
Second, we could not compare the costs of abortion provision by doctors vs. mid-level providers such as nurses or midwives, because in Mexico only doctors are currently permitted to provide abortion or treat incomplete abortion. A recent study in the United States examined different MA service delivery models using clinicians of varying levels and found cost differentials were at least partially related to provider level.Citation21 Third, our sensitivity analysis did not explore the possibility that some costs to the patient might increase with access to safe and legal abortion, such as increased user fees and out-of-pocket expenses related to recommended follow-up visits. Future studies should attempt to estimate these differences to capture a more complete picture of the true costs associated with both safe and unsafe abortions in Mexico for women and providers.
Doctors at the inauguration ceremony of the Reproductive Health area of the Centro de Salud Beatriz Velasco de Aleman, in Mexico City, where safe legal abortions are now being provided, 22 May 2008

Finally, it was beyond the scope of this study to conduct a full economic evaluation of the costs and health outcomes (morbidity and deaths) associated with unsafe abortion in Mexico. This cost analysis draws on primary data from four facilities representative of Mexico City, along with secondary data on abortion complications from Mexico City only. These are not representative of other parts of Mexico. A full economic analysis could model both the costs and effectiveness of alternative policy options and at the same time extend the geographic representation and the analytical horizon.
After this study was completed (2005), elective abortion up to 12 weeks gestation was legalised in Mexico City (2007) and access to safe abortions has increased.Citation22 It is too early to assess whether the increase in demand on the health system for legal abortions in this new environment will translate to savings to the public health system. This is because the reduction in per capita costs might be outweighed by a larger number of women seeking elective abortion than those seeking treatment for incomplete abortion in the past. It is clear, however, that many more women could have safe abortions with the same amount of funds. We hope to conduct a follow-up cost analysis within 3–5 years of the change in legislation, when services should be well established, in order to further document the cost impact of improving access to safe, legal abortion.
Our data provide overwhelming support for shifting abortion management from emergency, inpatient procedures to routine, outpatient procedures in Mexico City, as well as shifting away from D&C to MVA and MA. In 2008, the Mexico City Ministry of Health opened the first legal abortion service at the health centre level. They have also made important strides in reducing the use of D&C to induce abortion and moving toward more widespread use of MVA and MA. It is hoped that Mexico City will serve as a model for other parts of Mexico and that our findings will help to convince other countries where unsafe abortion is still prevalent that the provision of safe abortion care is not only cost-effective but better addresses the needs of women.
Acknowledgements
This study was funded by an anonymous donor. A version of this paper was presented at the annual meeting of the National Abortion Federation on 24 April 2006.
References
- D Lara, SG Garcia, J Strickler. El acceso al aborto legal de las mujeres embarazadas por violación en la ciudad de México. Gaceta Médica de México. 139(1): 2003; S77–S90.
- Alan Guttmacher Institute. Aborto clandestino: una realidad latinoamericana. Fact sheet. 1994; Allan Guttmacher Institute: New York.
- H Espinoza, K Abuabara, C Ellertson. Physicians' knowledge and opinions about medication abortion in four Latin American and Caribbean region countries. Contraception. 70(2): 2004; 127–133.
- J Sherris, A Bingham, MA Burns. Misoprostol use in developing countries: results from a multicountry study. International Journal of Gynecology and Obstetrics. 88(1): 2005; 76–81.
- D Lara, K Abuabara, D Grossman. Pharmacy provision of medical abortifacients in a Latin American city. Contraception. 74(5): 2006; 394–399.
- DL Billings, J Benson. Postabortion care in Latin America: policy and service recommendations from a decade of operations research. Health Policy and Planning. 20(3): 2005; 158–166.
- A Faúndes, LC Santos, M Carvalho. Post-abortion complications after interruption of pregnancy with misoprostol. Advances in Contraception. 12(1): 1996; 1–9.
- D Walker, L Campero, H Espinoza. Deaths from complications of unsafe abortion: misclassified second trimester deaths. Reproductive Health Matters. 12(24 Suppl): 2004; 27–38.
- F Juarez, S Singh, SG Garcia. Estimates of induced abortion in Mexico: what's changed between 1990 and 2006?. International Family Planning Perspectives. 34(4): 2008; 158–168.
- SK Henshaw, I Adewole, S Singh. Severity and cost of unsafe abortion complications treated in Nigerian hospitals. International Family Planning Perspectives. 34(1): 2008; 40–50.
- World Health Organization Department of Reproductive Health and Research. Mother-Baby Package Costing Spreadsheet Version 1.01. 1999; WHO: Geneva.
- Mexican Ministry of Health. Automated Hospital Discharge Records System 2004. 2005; Mexican MoH: Mexico City.
- Instituto Mexicano del Seguro Social. Hospital Release Records Database 2004. 2005; IMSS: Mexico City.
- Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado. Hospital Release Records, Mexico 2004. 2005; ISSSTE: Mexico City.
- M Berer. National laws and unsafe abortion: the parameters of change. Reproductive Health Matters. 12(24 Suppl): 2004; 1–8.
- World Health Organization. Safe abortion: technical and policy guidance for health systems. 2003; WHO: Geneva.
- C Brambila, A Langer, C Garcia-Barrios. Estimating costs of postabortion services at Dr. Aurelio Valdivieso General Hospital, Oaxaca, Mexico. D Huntington, NJ Piet-Pelon. Postabortion Care: Lessons from Operations Research. 1999; Population Council: New York, 108–124.
- BR Johnson, J Benson, J Bradley. Costs and resource utilization for the treatment of incomplete abortion in Kenya and Mexico. Social Science and Medicine. 36: 1993; 1443–1453.
- DL Billings. Misoprostol alone for early medical abortion in a Latin American clinic setting. Reproductive Health Matters. 12(24 Suppl): 2004; 57–64.
- WH Clark, M Gold, D Grossman. Can mifepristone medical abortion be simplified? A review of the evidence and questions for future research. Contraception. 75(4): 2007; 245–250.
- A Afable-Munsuz, H Gould, F Stewart. Provider practice models for and costs of delivering medication abortion – evidence from 11 US abortion care settings. Contraception. 75(1): 2007; 45–51.
- ML Sánchez Fuentes, J Paine, B Elliott-Buettner. The decriminalisation of abortion in Mexico City: how did abortion rights become a political priority?. Gender & Development. 16(2): 2008; 345–360.