Abstract
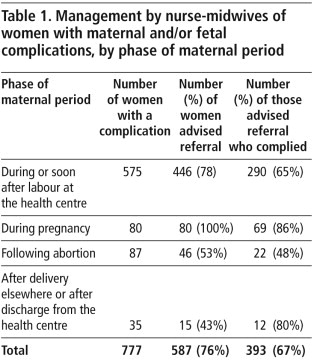
This paper documents the experience of two health centres in a primary health service located in interior rural areas of southern Rajasthan, northern India, where trained nurse-midwives are providing skilled maternal and newborn care round the clock daily. The nurse-midwives independently detect and manage complications and decide when to refer women to the nearest hospital for emergency care, in telephonic consultation with a doctor if required. From 2000-2008, 2,771 women in labour and 202 women with maternal emergencies who were not in labour were attended by nurse-midwives. Of women in labour, 21% had a life-threatening complication or its antecedent condition and 16% were advised referral, of which two-thirds complied. Compliance with referral was higher for maternal conditions than fetal conditions. Among the 202 women who came with complications antenatally, post-abortion or post-partum, referral was advised for 70%, of whom 72% complied. The referral system included counselling, arranging transport, accompanying women, facilitating admission and supporting inpatient care, and led to higher referral compliance rates. There was only one maternal death in nine years. We conclude that trained nurse-midwives can significantly improve access to skilled maternal and neonatal care in rural areas, and manage maternal complications with and without the need for referral. Protocols must acknowledge that some families might not comply with referral advice, and also that initial care by nurse-midwives can reverse progression of certain complications and thereby avert the need for referral.
Résumé
Dans deux centres de santé d’un service de soins de santé primaires situé dans des zones rurales de l’intérieur du Rajasthan méridional, en Inde septentrionale, des infirmières sages-femmes formées assurent des soins de la mère et du nouveau-né tous les jours, 24 heures sur 24. Les infirmières sages-femmes décèlent et prennent en charge indépendamment les complications et décident quand transférer les femmes à l’hôpital le plus proche pour des soins d’urgence, si nécessaire en consultation téléphonique avec un médecin. De 2000 à 2008, les infirmières sages-femmes se sont occupées de 2771 femmes en couches et de 202 femmes avec d’autres urgences maternelles. Sur les femmes en couches, 21% présentaient une complication pouvant entraîner la mort ou son stade précédent ; et 16% se sont vu conseiller un transfert et les trois quarts l’ont accepté. L’acceptation du transfert était plus élevée pour les problèmes maternels que fłtaux. Un transfert a été conseillé à 70% des 202 femmes présentant des complications prénatales, post-avortement ou post-partum, et 72% d’entre elles l’ont accepté. Le système de transfert comprenait des conseils, l’organisation du transport, l’accompagnement des patientes, l’aide à l’admission et aux soins hospitaliers ; il a accru les taux d’acceptation du transfert. Un seul décès maternel a été enregistré en neuf ans. Nous en concluons que, dans les zones rurales, les infirmières sages-femmes formées peuvent notablement élargir l’accès à des soins maternels et néonatals compétents, et prendre en charge les complications maternelles nécessitant ou non un transfert. Les protocoles doivent reconnaître qu’il arrive que des familles ne suivent pas les recommandations de transfert et aussi que les soins donnés initialement par des infirmières sages-femmes peuvent régler certaines complications et éviter la nécessité d’un transfert de la patiente.
Resumen
Este artículo documenta la experiencia de dos centros de salud de primer nivel situados en zonas rurales del interior de Rajasthan meridional, en la India septentrional, donde enfermeras-parteras profesionales capacitadas brindan atención calificada a madres y recién nacidos las 24 horas del día. Independientemente, ellas detectan y manejan complicaciones y deciden cuándo remitir a las mujeres al hospital más cercano para que reciban atención de urgencia, en consulta telefónica con un médico si es necesario. Desde 2000 a 2008, 2,771 mujeres en trabajo de parto y 202 con urgencias maternas, que no estaban de parto, fueron atendidas por enfermeras-parteras profesionales. De las que estaban de parto, el 21% presentó una complicación que puso en riesgo su vida, o su afección antecedente, y el 16% fueron aconsejadas referencia y, de éstas, dos terceras partes accedieron. El cumplimiento de la referencia fue más alto para las afecciones maternas que para las fetales. Entre las 202 mujeres que llegaron con complicaciones antenatales, se aconsejó referencia postaborto o posparto al 70%, de las cuales el 72% accedieron. El sistema de referencia incluyó consejería, planes de transporte, acompañar a las mujeres, facilitar admisión y atención con apoyo a las pacientes internadas, por lo cual aumentaron las tasas de cumplimiento de referencias. En nueve años hubo una sola muerte materna. Concluimos que las enfermeras-parteras profesionales capacitadas pueden mejorar considerablemente el acceso a la atención materna y neonatal calificada en zonas rurales, y manejar las complicaciones maternas con o sin la necesidad de referencias. Los protocolos deben reconocer la posibilidad de que algunas familias no sigan el consejo de referencia, y que la atención inicial brindada por enfermeras-parteras profesionales puede detener la evolución de algunas complicaciones y evitar la necesidad de referencia.
Enhancing access to skilled care during and after childbirth is a key strategy for reducing maternal mortality.Citation1Citation2 The 2005 World Health Report recommended provision of professional but de-medicalised care through midwife-led birthing centres located close to people's homes.Citation3 Thus, professionally trained midwives are an important human resource for rendering maternal health care, especially in underserved primary care settings. A functioning referral system and back-up hospital care are vital components of successful maternity care programmes.Citation4 However, referral to an urban hospital may not be possible or might be subject to delays because of distance, costs and the family's apprehensions about the woman being referred.Citation5
Within India, promoting institutional delivery through demand-side financing has become a key strategy to reduce maternal mortality – women receive a substantial cash payment if they deliver in a government health facility.Citation6 Concerns have been raised about under-equipped facilities consequently become overstretched and quality of care declining, but in fact the majority of institutional deliveries have taken place in doctor-led facilities with nurse-midwives working largely as assistants.
Service guidelines have been developed for use by skilled attendants working in primary care settings,Citation7Citation8 and their knowledge and skills have been studied and assessed.Citation9,10 Most guidelines mandate skilled, non-physician attendants to stabilise and then refer women with obstetric complications to the nearest emergency facility. In 2005 the Government of India issued guidelines allowing nurse-midwives to initiate emergency care independently before referral. However, there is little documented experience of the implementation of such guidance by first-level maternal care services, especially as to how midwives recognise, manage and refer for treatment of complications, and how families respond to the need for referral.
Rajasthan's maternal mortality ratio is estimated at 445 per 100,000 live births.Citation11 Deliveries in health facilities have increased from 15% in 1998-99 to 23% in 2005–06 for rural women,Citation12Citation13 but marginalised groups continue to lag behind in access to essential maternal health services. This paper documents the experience of two health centres in a primary health service located in interior rural areas of southern Rajasthan, in northern India, where trained nurse-midwives are providing skilled maternal and newborn care round the clock every day. The nurse-midwives independently detect and manage complications and decide whether to refer women to the nearest hospital for emergency obstetric care, in telephonic consultation with a doctor, when required. It analyses the factors influencing decisions on when to manage women locally and when to refer women with maternal complications, and describes an active referral system which allowed for rapid access to emergency obstetric care for women, especially those from the poorer, socially disadvantaged communities of the area.
Intervention and data sources
Action Research and Training for Health (ARTH), a non-profit public health organisation based in southern Rajasthan since 1997, has implemented a field service programme for a rural population inhabiting 49 villages (2008 population estimated at 57,000). Recognising the paucity of doctors in the rural interiors, ARTH initiated a service to demonstrate the feasibility of providing maternal health services through nurse-midwives, by training, empowering and supporting them in this role. The first health centre started providing 24-hour maternal—neonatal health services in 1999, and a second one commenced at the end of 2002. Southern Rajasthan's villages comprise several small hamlets scattered across low hills. While motorable roads reach most village centres, most hamlets, which are inhabited by marginalised scheduled tribes, are accessible only on foot. Data reported in this paper cover the nine years from January 2000 to December 2008.
Midwives recruited to health centres had either undergone an 18-month auxiliary nurse-midwife (ANM) certificate course or a three-year general nursing and midwifery (GNM) diploma, both recognised by the state nursing council. A quick assessment of knowledge and skills at the time of recruitment suggested that most lacked the skills and confidence to conduct a delivery or manage emerging complications independently. Doctors and senior nurse-midwives provided them with practical on-the-job training over 48 days in maternal—neonatal health care. ARTH developed and field-tested a local language training moduleCitation14 by adapting generic service guidelines from the World Health Organization (WHO), Saving Newborn Lives and Government of India.Citation7,8,15–21
Antenatal care provided at the health centre was based on the WHO antenatal care model, (20) adapted for use by midwives in a primary care setting. Nurse-midwives were trained to follow evidence-based labour and delivery care practices.Citation17Citation21 They were specifically instructed not to augment labour even in the face of pressure from family members to hasten delivery. Women were discharged a minimum of 24 hours after delivery; those with maternal or neonatal problems stayed for a few days longer, as required. Decision-making protocols for managing complications during pregnancy, labour and the post-partum period were in accordance with WHO guidance;Citation7 cut-off criteria for referral were conveyed during training and reinforced at the time of the doctors' routine visits and during emergency telephonic consultations. Although a lot depended on when women presented at the health centre, the practice was to detect and manage complications in the early stages and/or to advise referral before they developed into full-blown emergencies. For example, referral was considered when the partograph crossed the alert line, when transverse lie was detected or when a woman presented in labour with a twin pregnancy. Thus, referral was advised both for complications and for “antecedent conditions” that were likely to lead to complications. After 2007, midwives had a 24-hour facility for consultation with doctors over mobile phones linked through a closed users' group. They were trained in emergency measures like using intravenous fluids, magnesium sulphate, antibiotics, oxytocics after delivery and ovum forceps for evacuating products of conception.
In rotation, one of three women gynaecologists visited each health centre on fixed days, either once or twice a week. She provided outpatient services (including first trimester abortions), reviewed treatment of women with complications, and reinforced training messages. The visiting doctor made a conscious effort to guide and support the nurse-midwives on the day of her visit, when there were more patients. Women in labour were managed by nurse-midwives even on days when the doctor was visiting — she was called in only in the event of a problem or complication. Families paid a nominal charge for delivery at the health centre — Rs 100-150 (US$2-3) for socially disadvantaged groups and Rs 250-350 (US$5-7) for other communities. These charges were inclusive of admission, delivery, medications, inpatient stay and (after 2005) a set of clothes for the newborn and one to two post-natal home visits. For referral to the city hospital, poorer families received free or subsidised transport and initial medication, at the discretion of the nurse-midwife on duty.
When necessary, nurse-midwives advised referral to the comprehensive emergency obstetric and neonatal care facility at the medical college hospital in Udaipur city, located 58 and 30 km away, respectively, from the two health centres. Services at this hospital are intended to be free or very nominally priced. On determining that referral was required, the nurse-midwife counselled the family about the woman's condition and likely risks to the woman or fetus, assured them that she would accompany them to hospital and/or arrange for a social worker to meet them on admission, and offered to arrange for transport (free or subsidised for poorer sections). Once the family agreed, she prepared a referral note and hired a local fixed-price jeep-taxi. Carrying a small medical kit, she accompanied the woman to the hospital, where she facilitated timely admission, while also telephoning a social worker based in Udaipur. The social worker met the family during or soon after admission and made daily rounds of the hospital until discharge. His role was to reassure the patient and family, help with difficult decisions such as agreeing to surgery or blood donation, help family members avail of subsidies (including free medication, meals for relatives and fair-priced drugs), and confront any demands for irregular payment. Nurse-midwives recorded antenatal care on a patient-retained card and register; kept notes on labour (including partograph), post-partum and neonatal care till discharge on a user-friendly case sheet; and recorded the management of complications in registers. Families that refused referral advice despite counselling were asked to sign an undertaking to that effect. For women who reached hospital, the social worker recorded admission and treatment specifics (including surgery and blood transfusion) and outcomes, while an outreach worker made home visits after a month and a half to record outcomes among women with complications. This visit to record outcomes was made for all women from ARTH's field area, even if the women did not comply with referral advice. A programme coordinator (an obstetrician) reviewed complications and referrals during monthly meetings. Data were analysed using Epi Info.
Findings
The two health centres commenced operations respectively in October 1999 and December 2002. Maternal and fetal complications were detected and managed by nurse-midwives in two instances — among women in labour coming for delivery and among those presenting with a problem during pregnancy, after abortion or during the post-partum period.
Women presenting in labour
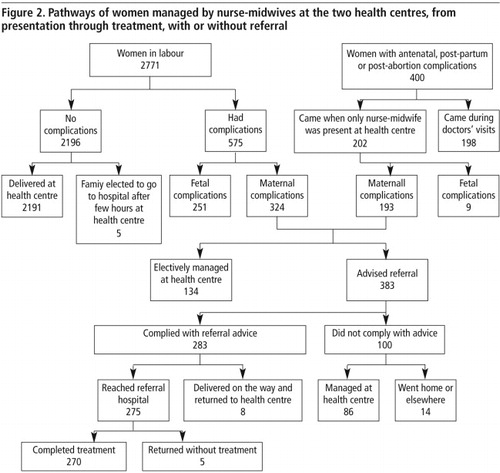
The number of women coming to both health centres for delivery increased steadily till 2006, after which there was a drop following the introduction of the cash benefit scheme to women who delivered at government hospitals. It took over a year and a half before our two midwife-led centres could be accredited under the scheme. Of 2,771 women who presented in labour from January 2000 to December 2008 (), nurse-midwives detected complications in 575 (20.7%) (Table 1). These included 324 women primarily with a maternal complication and 251 with a fetal complication. Of those with maternal complications, first-level emergency management succeeded in stabilising 73 to the extent of obviating the need for referral. The rest were advised to accept referral, but the families of 62 women refused. Eight of those who undertook the journey to the referral hospital delivered on the way (assisted by the accompanying nurse-midwife) and returned to the health centre.
Women presenting with complications during pregnancy, after abortion or delivery
During the same period, 400 women presented with complications during pregnancy, after abortion or after delivery. Of these, 198 women came on days when a doctor was visiting and were managed as per her direct instructions. The remaining 202 women (193 with maternal and 9 with fetal complications) presented on other days and were attended by nurse-midwives ().
Of the total of 517 women with maternal complications managed by nurse-midwives (324 that presented in labour and 193 that presented in other phases of maternity), 74% were advised referral and 74% of those actually complied. Among the 260 women with fetal complications, 77% were advised referral, but only 53% of those actually complied. Thus, family compliance with referral advice was significantly lower for fetal conditions than maternal ones (p<0.001). The rest of this paper focuses on emergency management in the health centre and referral of the 517 women with maternal complications.
Support for women during referral and admission to hospital in Udaipur
Of the women who complied with referral advice, 77% were either accompanied en route by the nurse-midwife, or were met at the hospital by a staff social worker. Families of women in labour better recognised the urgency of the situation and more promptly agreed to travel to the hospital. Hence, ARTH staff were able to support as many as 89% of them. By contrast, more families of women who were not in labour preferred to first make alternative arrangements at home and then go (often a day or two later) at their own convenience; hence fewer (52%) could be supported by ARTH staff. The difference was highly significant (p <0.001).
Maternal outcomes of women managed by nurse-midwives
shows the pathways of the women managed by nurse-midwives at the two health centres, from presentation through treatment, with or without referral. Of the 2,771 women who were attended by nurse-midwives during labour, there were no maternal deaths, whether or not they were referred. Of the 202 women with maternal emergencies but who were not in labour, there was one maternal death after referral. This woman had come with jaundice during pregnancy, and was successfully referred before labour commenced. She delivered in the referral hospital three days after admission but died from post-partum haemorrhage.
Management by nurse-midwives of maternal complications by type of complication
Nurse-midwives attended to a total of 517 women with maternal complications. If a woman had more than one complication, we included the most serious complication in the analysis. While after 2004 nurse-midwives could consult the doctor over the telephone, they themselves had to decide whether to refer individual women with complications, depending on the woman's condition. Table 2 reveals that nurse-midwives referred most or all women with antepartum haemorrhage, severe anaemia, pregnancy-induced hypertension and obstructed labour (and their antecedent conditions). The 134 (26%) women with complications who were not advised referral largely included women with post-partum haemorrhage (and its antecedent conditions) and post-abortion complications.
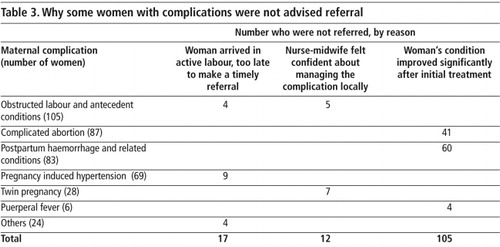
Why some women with maternal complications were not advised referral
We reviewed case notes and retrospectively assessed nurse-midwives' reasons for not referring 134 women with maternal complications. For 41 women with post-partum haemorrhage, nurse-midwives used oxytocics and IV fluids while referral was being considered and transport arranged. In the interim, bleeding reduced substantially among most of the women, and only nine required to be referred. Similarly, the use of oxytocics and controlled cord traction resolved retained placenta in 24 of 37 women who presented with the condition, while the bleeding in four women with a vaginal tear stopped after compression and clamping. For six women with puerperal fever, the use of oral or injectable antibiotics meant that only two had to be referred.
Thirty of the 51 women with incomplete abortion responded after nurse-midwives administered oxytocin and, digitally or with an ovum forceps, removed any visible products of conception; the rest were referred. Five of 20 women with threatened abortion had normal vital signs; after telephonic consultation with the gynaecologist, they were advised rest at home, and their pregnancy continued. Two of eight women with septic abortion had mild sepsis with no evidence of perforation or peritonitis; nurse-midwives consulted the gynaecologist by telephone, admitted them to the health centre and administered fluids and antibiotics until the gynaecologist saw them 1-2 days later on a routine visit. Four of eight women with inevitable miscarriage had normal vital signs and the miscarriage was complete within hours at the health centre.
While nurse-midwives advised referral for all women presenting with transverse lie (11) and obstructed labour (14), they judged the maternal and fetal condition to be good in the cases of five of 70 women in whom the partograph crossed the alert line, and elected to wait a bit longer – labour progressed and the women in question delivered at the health centre within a few hours. Four out of nine women with face presentation arrived during advanced labour; the nurse-midwife judged that the delivery might occur too quickly for referral to be carried out and hence chose to manage them locally. Similarly, all ten with eclampsia were advised referral. However, out of 59 women with pre-eclampsia, eight presented during advanced labour; the nurse-midwives administered magnesium sulphate and delivered them at the health centre. Blood pressure declined rapidly after delivery, thereby obviating the need for referral.
Nurse-midwives would initially refer all women with twin pregnancy in labour. However, when a few families refused referral, they had no option but to manage them at the health centre. This gave them the experience and confidence to manage uncomplicated (without anaemia or pre-eclampsia) twin delivery, and they elected not to refer seven out of 28 such women who presented subsequently. Thus, there were three main reasons for not advising referral for some women with complications, which appeared to vary according to the type of complication, as shown in Table 3.
Why some families refused to comply with referral advice
Families of 100 women with maternal complications did not comply with nurse-midwives' advice regarding referral, despite having been counselled and offered transport and accompaniment to the hospital. They included 62 women in labour and 38 who presented with complications during pregnancy, after abortion or after delivery.
We attempted to discern patterns in families' willingness to comply with referral advice. Family compliance was significantly higher (p=0.00019) for maternal complications that occurred before the baby was born (78.7%), as compared to those that occurred after delivery or abortion (57.1%). However, there were a few exceptions to this general pattern – families appeared reluctant to travel to hospital for a twin delivery (compliance 8 out of 21, 38%), while they appeared to be more willing to do so for retained placenta (11 out of 13, 85%) and puerperal fever (2 of 2, 100%). The latter two conditions are well recognised in local tradition as being serious. Compliance among families belonging to marginalized tribal and better-off groups was similar (p>0.05).
Nurse-midwives advised immediate referral for all women with transverse lie, obstructed labour, eclampsia, antepartum haemorrhage and severe anaemia. Compliance was 100% for the first three conditions, but only 52 out of 62 (83%) in cases of antepartum haemorrhage and 39 out of 53 (69%) with severe anaemia. This was probably because family members were informed about the likely need for blood transfusion at the hospital for the latter two conditions. They tended to be apprehensive about being asked by hospital staff to donate blood by way of replacement, this being hospital policy. Families also tended to refuse referral if they knew from the past experience of others that the condition could be managed locally by nurse-midwives. This occurred in cases of prolonged labour, abortion complications, twin pregnancy and even post-partum haemorrhage. In such cases, family members would negotiate with nurse-midwives, citing precedents, and would plead for treating women at the health centre itself. It proved especially difficult to convince the families of women with severe anaemia that the condition was serious and urgent. This was possibly because, during the months of pregnancy, relatives had become used to seeing symptoms like breathlessness and effort intolerance in the woman.
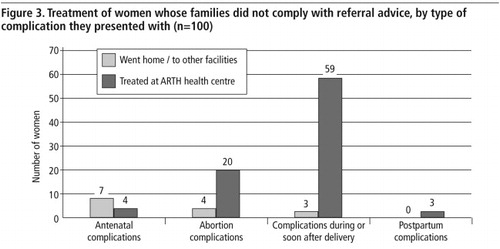
Treatment of women whose families did not comply with referral advice
Among the women with complications whose families did not comply with referral advice (), most (86 out of 100) remained at the health centre, where nurse-midwives continued treatment to the best extent possible, without discrimination. Of the 14 women who preferred treatment elsewhere, seven had developed complications during pregnancy (four with severe anaemia, two with twins and one with mild antepartum haemorrhage). These women had come for a routine antenatal visit and were not prepared to be rushed abruptly to hospital. Seven others included four women with abortion complications who returned home and three women in labour, of whom one was severely anaemic and was taken to an unequipped community health centre and two who went to even smaller local facilities. There were no maternal deaths among the women whose families did not comply with referral advice.
Discussion
A referral system that couples primary health care institutions with emergency obstetric care is considered to be essential to prevent maternal deaths.Citation22 There is evidence that reducing delays in linking a woman with emergency obstetric care can make a difference in maternal mortality. However there is little documentation of the effectiveness of maternity referral systems.Citation4 One study in India found that only 10% of women advised referral by a primary-level institution eventually reached the referral facility.Citation23 Asha George, on the other hand, found in Karnataka that families lost valuable time and resources accessing many providers but failed to get effective care, while blame was laid on lower-level health workers and women for not accessing institutional delivery.Citation24
Maternal health interventions for low resource settings have emphasised a “step-up” sequence of early detection of complications, initial emergency care (”first-aid”) to stabilise and support the woman, transportation to effect quick referral to an emergency obstetric care facility, followed by prompt, definitive care at that facility. This approach does not acknowledge that early recognition and prompt emergency care might alter the natural course of certain complications to the extent that onward referral becomes unnecessary. Further, it has been shown that referral decisions are not just technical or organisational matters; they involve stress, fear and anxiety on the part of the provider, as well as on the part of patients and their families.Citation25
In our series, while the consistent practice of active management of third stage of labour prevented post-partum haemorrhage (PPH) in most women, oxytocics and intravenous fluids controlled bleeding in most of those that did develop PPH, thereby sharply reducing the need for referral. Similarly, supported by doctors' telephonic advice, most women with puerperal fever and about half of those with abortion complications could be managed locally. These three conditions contributed to a third of maternal complications in our series. For the few women (with face presentation and pre-eclampsia) that arrived in advanced labour, the nurse-midwife on duty decided that it was too late to refer. While we did not have the means to judge the merits of individual decisions of this nature, they represent critical situations that midwives working in remote rural areas are likely to face, and must make decisions on, based on the local context of distance and time to the nearest hospital. Lastly, confidence from past experience of managing women whose families had refused referral encouraged midwives to similarly manage a few women with twin pregnancies and prolonged labour.
A study of nurses working in rural Niger has highlighted that nurses might be unwilling to refer patients to hospital because they perceive it as leading to excessive referral, and as evidence of professional failure and loss of face in the eyes of patients' families.Citation26 Nurse-midwives in our series relied on local treatment (often under telephonic guidance) only for certain clinical conditions, while making immediate referrals for others. Ongoing supervision and feedback on the outcome of referred cases gave them a better understanding of when to refer, and there was no financial benefit in avoiding referral. We therefore conclude that effective training, supervision and feedback can enable nurse-midwives to successfully manage a significant proportion of maternal complications without referral.
After providing first-level emergency care, our intervention attempted to reduce all three delays in accessing referral services. This was achieved by counselling the family early about the need for referral. Several unwilling families were reassured when told that a staff member would accompany them and facilitate hospital admission. Given that high costs are a known barrier to referral,Citation27 securing a panel of fixed-price private jeeps and a transport subsidy for the poor helped to reduce that cause of delay. At the hospital, the nurse-midwife's referral note helped doctors to make a quicker diagnosis, while also assuring them that treatment provided thus far was in accordance with standard guidelines. Having a social worker maintain regular contact during inpatient stay ensured that treatment costs remained low, and the family did not prematurely leave the hospital in panic. Studies from three West African countries have revealed that the physical and social distance between the community and personnel at health facilities is a major barrier to obstetric referral.Citation28 We therefore recommend that the provision of referral support for indigent families be prioritised when planning maternal health services. A role for NGOs in helping to facilitate admission and inpatient stay could be explored on a larger scale.
Service guidelines tend to assume that a primary care provider's clinical decision to refer would be agreed to by the patient or family, provided transport is assured. Our own experience has been that decisions on treatment and referral in a time of crisis are often taken by family members without consulting the patient.Citation29 Despite our offer of support for hospitalisation, families of over a fourth of women did not comply with advice on referral. While we did not systematically document the reasons, some families appeared to feel that the condition could well be managed at the health centre, or (in the absence of overt symptoms) that it was not severe enough to require hospitalisation. In some instances, fear of having to donate blood at the city hospital added to their reluctance. Guidelines for peripheral-level providers should therefore recognise that referral might not always be possible and include advice on treatment options in cases where families refuse referral.
Our experience suggests that trained nurse-midwives can significantly improve access to skilled maternal and neonatal care in rural areas of India, and manage life-threatening maternal complications with and without the need for referral. This could be tested as part of a larger trial in a low-resource setting, comparing midwife-led rural maternal health facilities with services led by doctors.
Acknowledgements
We acknowledge the commitment and effort invested by nurse-midwives who staffed the two health centres during the reporting period, in providing round-the-clock services to women and newborns. The intervention in the field programme of Action Research and Training for Health (ARTH) has been funded by the John D and Catherine T MacArthur Foundation, Chicago, and Sir Ratan Tata Trust, Mumbai. These donors have had no involvement in the documentation or writing, or in the decision to submit the paper for publication.
References
- W Van Lerberghe, V De Brouwere. Of blind alleys and things that have worked: history's lessons on reducing maternal mortality. V De Brouwere, W Van Lerberghe. Safe Motherhood Strategies: A Review of the Evidence. 2001; ITG Press: Antwerp.
- M Kowalewski, A Jahn. Health professionals for maternity services: experiences on covering the population with quality maternal care. V De Brouwere, W Van Lerberghe. Safe Motherhood Strategies: A Review of the Evidence. 2001; ITG Press: Antwerp.
- World Health Organization. Skilled professional care: at birth and afterwards. World Health Report 2005: Make every mother and child count. 2005; WHO: Geneva.
- SF Murray, SC Pearson. Maternity referral systems in developing countries: current knowledge and future research needs. Social Science and Medicine. 61: 2006; 2205–2215.
- P Bossyns, R Abache, MS Abdoulaye. Unaffordable or cost effective? Introducing an emergency referral system in rural Niger. Tropical Medicine and International Health. 10(9): 2005; 879–887.
- India. Ministry of Health and Family Welfare. Janani Suraksha Yojana: features & frequency asked questions and answers. New Delhi: Ministry of Health and Family Welfare, Government of India, 2006. At: <http://mohfw.nic.in/dofw%r4920website/JSY_features_FAQ_r50Nov_2006.htm>. Accessed 4 May 2009.
- World Health Organization. Integrated management of pregnancy and childbirth. Pregnancy, Childbirth, Postpartum and Newborn Care: a guide for essential practice. 2003; WHO Department of Reproductive Health and Research: Geneva.
- Government of India. Guidelines for skilled attendance at antenatal and delivery care for ANMs and LHVs. 2005; Ministry of Health and Family Welfare, GOI: New Delhi.
- S Ramarao, L Caleb, ME Khan. Safer maternal health in rural Uttar Pradesh: do primary health services contribute?. Health Policy and Planning. 16(3): 2001; 256–263.
- SA Harvey, YCW Blandón, A McCaw-Binns. Are skilled birth attendants really skilled? A measurement method, some disturbing results and a potential way forward. Bulletin of World Health Organization. 85: 2007; 783–790.
- Registrar General of India. Sample registration system. Maternal mortality in India: 1997–2003: trends, causes and risk factors. 2006; Registrar General of India: New Delhi. 29 p.
- International Institute of Population Sciences. National Family Health Survey (NFHS-2), 1998–99: Rajasthan. 2000; IIPS & ORC Macro: Mumbai.
- International Institute of Population Sciences & ORC Macro. National Family Health Survey (NFHS-3), 2005–2006: Rajasthan. 2007; IIPS & ORC Macro: Mumbai.
- K Iyengar, SD Iyengar. Skilled care for maternal–neonatal health: practical guideline for nurse midwives (Hindi). 2005; Action Research and Training for Health: Udaipur.
- World Health Organization. Standards of Midwifery Practice for Safe Motherhood, Vol. 1–4. 1999; WHO Regional Office for South East Asia: New Delhi.
- World Health Organization. Education Material for Teachers of Midwifery (5 modules). 1996; WHO Maternal Health and Safe Motherhood Programme: Geneva.
- World Health Organization. Care in Normal Birth: a practical guide. WHO/FRH/MSM/96.24. 1996; WHO Maternal and Newborn Health/Safe Motherhood Unit, Family and Reproductive Health: Geneva.
- World Health Organization. Postpartum Care of the Mother and Newborn: a practical guide. WHO/RHT/MSM/98.3. 1998; WHO Maternal and Newborn Health/Safe Motherhood Unit, Division of Reproductive Health Technical Support: Geneva.
- World Health Organization. The Partograph: A Managerial Tool for the Prevention of Prolonged Labour. WHO/MCH/88.3.h. 1988; WHO Maternal and Child Health Unit, Division of Family Health: Geneva.
- World Health Organization. WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. 2001; UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction: Geneva.
- D Beck, F Ganges, S Goldman. Care of the newborn: reference manual. 2004; Save the Children: Oxford.
- A Jahn, V De Brouwere. Referral in pregnancy and childbirth: Concepts and strategies. V De Brouwere, W Van Lerberghe. Safe motherhood strategies: a review of the evidence. 2001; ITG Press: Antwerp. (Studies in Health Services Organisation and Policy), 17:229-246).
- J Hitesh. Perceptions and constraints of pregnancy related referrals in rural Rajasthan. Journal of Family Welfare. 42(1): 1996; 24–29.
- A George. Persistence of high maternal mortality in Koppal District, Karnataka, India: observed service delivery constraints. Reproductive Health Matters. 15(30): 2007; 91–102.
- HK Bachman, KD Freeborn. HMO Physicians use of referrals. Social Science and Medicine. 48: 1999; 547–557.
- P Bossyns, W Van Lerberghe. The weakest link: competence and prestige as constraints to referral by isolated nurses in rural Niger. Human Resources for Health. 2: 2004; 1. <www.human-resources-health.com/content/2/1/1. >. Accessed 9 May 2009.
- K Iyengar, SD Iyengar, V Suhalka. Pregnancy related deaths in southern Rajasthan: exploring context, causes and care seeking. Journal of Health, Population and Nutrition. 27(2): 2009; 293–302.
- Prevention of Maternal Mortality Network. Barriers to treatment of obstetric emergencies in rural communities of West Africa. Studies in Family Planning. 23(5): 1992; 279–291.
- SD Iyengar, K Iyengar, JC Martines. Childbirth practices in rural Rajasthan, India: implications for neonatal health and survival. Journal of Perinatolology. 28: 2008; S23–S30.