Abstract
Abstract
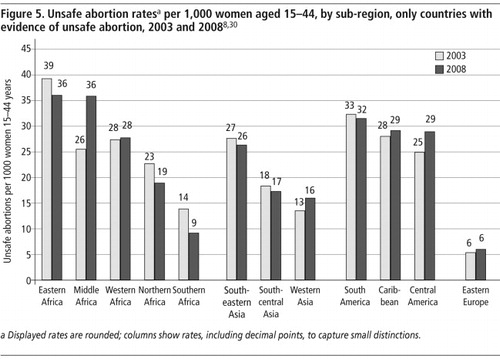
Despite the availability of safe and highly effective methods of abortion, unsafe abortions continue to be widespread, nearly all in developing countries. The latest estimates from the World Health Organization put the figure at 21.6 million unsafe abortions worldwide in 2008, up from 19.7 million in 2003, a rise due almost entirely to the increasing number of women of reproductive age globally. No substantial decline was found in the unsafe abortion rate globally or by major region; the unsafe abortion rate of 14 per 1,000 women aged 15–44 years globally remained the same from 2003 to 2008. Modest reductions in unsafe abortion rates were found in 2008 as compared to 2003 in most sub-regions, however. The upward changes in rates in Middle Africa, Western Asia and Central America were due to better coverage and more reliable information in 2008 than in 2003. Eastern and Middle Africa showed the highest rates of unsafe abortion among all sub-regions. Some 47,000 women per year are estimated to lose their lives from the complications of unsafe abortion, almost all of which could have been prevented through better access to sexuality education, fertility awareness, contraception and especially safe abortion services.
Résumé
En dépit de la disponibilité de méthodes sûres et très efficaces d'avortement, les avortements à risque continuent d'être nombreux, presque toujours dans les pays en développement. Les dernières estimations publiées par l'Organisation mondiale de la Santé chiffrent à 21,6 millions les avortements à risque dans le monde en 2008, contre 19,7 millions en 2003, une augmentation presque entièrement imputable au nombre croissant de femmes en âge de procréer. Aucun recul n'a été signalé dans les taux d'avortement à risque au niveau mondial ou par grande région ; le taux d'avortement à risque dans le monde, soit 14 pour 1000 femmes âgées de 15 à 44 ans, est demeuré le même de 2003 à 2008. Néanmoins, la plupart des sous-régions ont obtenu de modestes réductions des taux d'avortement à risque en 2008 par rapport à 2003. Les progrès notés en Afrique moyenne, en l'Asie de l'Ouest et en Amérique centrale étaient dus à une meilleure couverture et à des informations plus dignes de foi qu'en 2003. L'Afrique de l'Est et moyenne enregistraient les taux les plus élevés d'avortement à risque dans tous les sous-régions. On estime que près de 47 000 femmes perdent chaque année la vie en raison des complications d'un avortement à risque. Presque toutes auraient pu être sauvées par un meilleur accès à l'éducation sexuelle, la connaissance de la fécondité, la contraception et tout spécialement des services d'avortement sûr.
Resumen
A pesar de que existen métodos de aborto seguros y muy eficaces, el aborto inseguro continúa siendo una práctica generalizada, principalmente en los países en desarrollo. Según los últimos cálculos de la Organización Mundial de la Salud, la tasa mundial de aborto inseguro en 2008 fue de 21.6 millones; subió de 19.7 millones en 2003, un aumento atribuible casi totalmente al creciente número de mujeres en edad reproductiva a nivel mundial. No se encontró ningún descenso significativo en la tasa de aborto inseguro globalmente o por región principal; entre 2003 y 2008, la tasa mundial de aborto inseguro continuó siendo 14 por cada 1000 mujeres de 15 a 44 años de edad. Sin embargo, en 2008 se encontraron moderadas reducciones en las tasas de aborto inseguro comparadas con las tasas en 2003 en la mayoría de las subregiones. Los aumentos en las tasas de Ãfrica Central, Asia Occidental y Centroamérica se debieron a una mejor cobertura e información más fidedigna en 2008 que en 2003. Las tasas más altas de aborto inseguro en todas las subregiones se encontraron en Ãfrica Oriental y Central. Se calcula que cada año unas 47,000 mujeres pierden la vida a consecuencia de las complicaciones del aborto inseguro, la gran mayoría de las cuales pudieron haberse evitado con mejor acceso a educación sexual, conocimiento de la fertilidad, anticonceptivos y especialmente servicios de aborto seguro.
Millions of unsafe abortions continue to take place globally every year despite the high prevalence of contraception and the existence of safe and effective methods of abortion. This is not only because all contraceptive methods occasionally fail and people fail to use them correctly or consistently, leading to unintended pregnancies, but also because millions of women around the world do not have access to safe abortion services when they decide to terminate a pregnancy. Where abortion is legally restricted, some women go on to have unwanted children; most women, however, end up having unsafe abortions.
The World Health Organization (WHO) definition of unsafe abortion since 1992 is: “a procedure for terminating an unintended pregnancy that is carried out either by a person lacking the necessary skills or in an environment that does not conform to the minimal medical standards, or both”.Citation1 This definition is linked to the skill of the person carrying out the abortion and the conditions in which the procedure was carried out. It was developed in the late 1980s, at a time when most methods of abortion being used were surgical and/or invasive, that is, an instrument had to be inserted into the uterus to carry out the procedure that would terminate the pregnancy. Abortion methods have changed greatly since then and those currently recommended by WHO are among the safest clinical interventions available in health care today.Citation2
Unsafe abortion providers largely continue relying on risky or traditional methods; studies show a range of unsafe abortion methods and actions that are taken to abort a pregnancy. However, with the advent of medical abortion pills, in countries where abortion remains legally restricted, women are using these pills to induce an abortion on their own.Citation3 The typical characteristics of an unsafe abortion where medical abortion pills have been used involve the woman using too little or too much medication, or using pills of dubious quality, obtained from unreliable sources. There are, however, indications that use of medical abortion has contributed to lowering both the number of severe complications and of maternal deaths in the countries where the medication is accessible.Citation4–6
No matter what the abortion method used, the abortion may be incomplete or serious complications may occur, and post-abortion care will be necessary. If the woman then seeks help for complications and there is insufficient capacity to manage these conditions, or the woman delays seeking medical care because of legal restrictions, stigma or financial constraints, complications may worsen and become a medical emergency, presenting a risk to the woman's life and health.
It is important to add that not all unsafe abortions lead to complications. It is estimated that approximately one in four women who have had an unsafe abortion will need medical attention.Citation7 According to the new WHO estimates, among the estimated 358,000 maternal deaths in 2008, 47,000 were due to complications of unsafe abortion.Citation8 Some of the women who survive will suffer long-term health consequences, including infertility due to untreated infection, however, while many more will experience short-term morbidity.Citation7
This paper provides the most recent estimates of unsafe abortion, for 2008, compiled by WHO. It also examines trends in the incidence and rates of unsafe abortion, and compares the estimates for each region when countries with no evidence of unsafe abortion are included in the estimates to when they are excluded.
Methods
WHO maintains a database on unsafe abortion and associated mortality, which at this writing contains almost 4,000 documents, mainly relating to developing countries. Information relevant to understanding and measuring unsafe abortion covers data from hospital records and surveys, studies on abortion providers, unsafe abortion methods, abortion-seeking behaviour, post-abortion care, and legal developments.
Where induced abortion is highly restricted, its occurrence can be estimated only indirectly, using the available, albeit incomplete, information on incidence and mortality due to unsafe abortion.Citation9 For these estimates thousands of papers were screened to select relevant materials that provided new data or information. These materials were identified from bibliographic databases; websites of relevant organizations; and by country searches for the most up-to-date data, including ministry of health and other official sites. Both published and unpublished studies and data were included after reviewing the critical elements such as study design, coverage, and defined outcome variables. Abortions in highly restricted legal contexts were considered unsafe, as were abortions taking place outside the legal framework.
Correcting for misreporting and under-reporting, unsafe abortion rates and ratios were generated first by country, and then aggregated, after weighting by numbers of women or live births as appropriate, by sub-region, region and globally.
To deal with the problem of induced abortion being misreported as spontaneous, the combined incidence of spontaneous and induced abortion is used for estimation, correcting for the likely incidence of spontaneous abortion, as described in detail below. Where induced abortions take place both within and outside the legal context of a country, officially sanctioned abortions are excluded from the unsafe abortion estimate.
Hospital abortion admission data over-represent the occurrence of spontaneous abortions. In most instances, it is not clinically possible to separate spontaneous from induced abortions and therefore estimates must rely on a biological model to account for the percentage of spontaneous abortions represented in the hospital data. The number of women not receiving care relative to hospitalized women will have to be estimated through special studies.Citation10Citation11 Only some of the women having an unsafe abortion will need and be able to seek hospital care; such a decision is not only influenced by the severity of the symptoms (e.g. bleeding, pain, fever, infection) but also by the availability of and access to medical services, the (perceived) legal conditions of induced abortion, and the fear of being reported. Hesitation to seek care increases the health risks to women and may lead to permanent disability or death.
National unsafe abortion incidence was estimated from hospital data by simulating the hospitalization complications method (HCM).Citation10Citation11 The abortion-to-birth ratio in hospitals is adjusted for spontaneous abortions that occur at 13–22 weeks of pregnancy that may require hospital treatment. Women who have a miscarriage before 13 weeks of pregnancy rarely need hospital care. Using modified life-table data, Singh and WulfCitation12 estimated that the number of pregnancies ending in spontaneous abortion within 13–22 weeks of pregnancy corresponds to 3.41% of all live births. They further assumed that the percentage of women with spontaneous abortion who are hospitalized is approximately equal to the percentage of women who deliver in a hospital in a given country. The hospital unsafe abortion ratio so derived – the tip of the iceberg – is further adjusted based on the evidence that most unsafe induced abortions do not lead to complications requiring hospitalization; therefore a multiplier of between 2 and 7Citation10–14 is applied to the hospital unsafe abortion ratio to arrive at an estimate of the national unsafe abortion ratio. The multiplier is implemented from the above-mentioned studies in various locations on the basis of similarity to a country with a known multiplier. Generally, the magnitude of the multiplier implies that the lower the risk to women's health that is associated with unsafe abortions in a country, the higher the multiplier will be. The calculated abortion ratio is finally converted into an abortion rate, based on UN Population Division estimates of the numbers of women aged 15–44 years, and of births, for that calendar year.Citation15
Women are often reluctant to admit to having had an induced abortion, especially when its availability is restricted by law. However, surveys show that substantial under-reporting occurs even where abortion is both accessible and available within the legal framework.Citation16–19 It appears that early pregnancy terminations and events occurring some time back in the past are less frequently reported.Citation20 When abortions are clandestine, women tend to under-report induced abortions in surveys despite assurance of confidentiality, and because of the stigma attached to the event, or may only admit to a spontaneous abortion (miscarriage).Citation21Citation22 Data from surveys therefore have to be adjusted for under-reporting and account for spontaneous abortion when included. To avoid the dilemma and difficulty in distinguishing spontaneous as compared to induced abortions, it was considered more reliable to start with the combined numbers, finally deducting spontaneous abortions, estimated at 10% of survey data on births,Citation20 from the combined national incidence to account for numbers of spontaneous abortions.
Surveys on abortion have shown that women under-report their abortion experience in face-to-face interviews and in self-completed forms. Studies in the USA show that fewer than one half of induced abortions performed in the preceding five years were reported in interviews,Citation17,20,23,24 while just over 50%, admitted induced abortion in a self-report procedure (audio-computer assisted).Citation23 Although sensitive interviewingCitation25 may render somewhat better results, an augmenting factor of two is applied when estimating unsafe abortion from surveys, that is, assuming that one in two women will admit to an abortion.
Country-specific estimates were corroborated with information from other sources on total fertility rate, use of modern and traditional contraceptive methods, and other proximate determinants of fertility, as available. The latest estimates are based on data available as of 30 April 2010. Estimates were calculated for the geographical regions, as defined by the United Nations. Further details of data, methods and estimation procedures as of 2010 are available in WHO.Citation8
Unsafe abortion in 2008
WHO estimates that 21.6 million unsafe abortions took place worldwide in 2008, almost all in developing countries.Citation8 The number of unsafe abortions, though sizeable, is not a valid measure for comparison of the magnitude across regions and over time because of the differences in size of population in the different regions and sub-regions as well as differences in the growth of population in each region over time. Appropriate indicators for such comparisons are the unsafe abortion rate, that is, the number of unsafe abortions per 1,000 women aged 15–44 years, and the unsafe abortion ratio, that is, the number of unsafe abortions per 100 live births. Table 1 summarizes the estimated unsafe abortion numbers, rates and ratios by geographical region, as defined by the United Nations Population Division (UNPD).
Worldwide, in 2008, the estimated annual number of unsafe abortions had increased by about two million from the estimate of 19.7 million in 2003; this is due to the increasing number of women of reproductive age globally. Nearly all unsafe abortions (98%) occurred in developing countries, and the rates were significantly higher in the least developed countries and in sub-Saharan Africa, 27 and 31 respectively, than the average for all less developed regions (16 per 1,000 women aged 15–44 years). Unsafe abortion ratios were, however, relatively low (18 and 17 per 100 live births, respectively). When fertility is high and there are large numbers of births, as is the case for Eastern, Middle and Western Africa, the abortion ratios are lower despite the high numbers of abortions because the denominator of births for computing the ratio is large. The opposite holds for regions with low fertility and fewer births, as can be seen for Latin America and South-Eastern Asia.
The Africa region shows contrasting patterns by sub-region. Unsafe abortion rates per 1,000 women aged 15–44 years range widely, from a low of 9 in Southern Africa to 36 in Eastern and Middle Africa. Unsafe abortion rates are higher in Eastern and Middle Africa (36 per 1,000) than for any other sub-region and are among the most elevated in Western Africa. Total fertility rates remain well above five children per woman in Eastern, Middle, and Western Africa and the overall contraceptive use is low: 26%, 19% and 15%, respectively. All other sub-regions of Africa, as well as Asia and Latin America, show contraceptive prevalence above 50%.Citation26 In the central belt across Africa, unsafe abortion rates may remain high until contraceptive use shows an increase to over 30%, which Streatfield found in Matlab, Bangladesh, in a study of the relationship between rates of contraceptive use, total fertility and abortion.Citation27
The picture is quite different in the Southern and Northern sub-regions of Africa. Northern and Southern Africa include countries where contraceptive prevalence is high and safe abortion is partially accessible. Unsafe abortion rates are, therefore, low in these sub-regions. Abortion is legal on broad grounds in South Africa and safe abortion services are increasingly available, although unsafe abortions are not yet entirely eliminated. In Tunisia, abortion has long been legal and safe, with functioning abortion services. Contraceptive prevalence in Southern and Northern Africa among married women is 58% and 50%, respectively, and couples rely mainly on modern methods. Thus, these two sub-regions have total fertility rates that are below three children per woman and unsafe abortion rates that are 25% and 50% of those of Eastern Africa, respectively. Nevertheless, restrictive legal conditions continue to account for unsafe abortions in the Northern African sub-region.
With 4.2 million unsafe abortions in 2008, numbers and rates of abortions in the Latin America and Caribbean regions have increased slightly. This is due to the availability of new and more complete information for Central America in 2008 than in 2003. The rate was 29 per 1,000 women aged 15–44 in Central America in 2008, and lower in the Caribbean at 18 per 1,000, a region that also includes Cuba, where abortion is available on request and services are easily available. On the other hand, though the rate still is high, the incidence of unsafe abortion at 32 per 1,000 women aged 15–44 for South America appears to have stabilized. The use of modern contraceptives ranges from 58% to 65% in Latin America, of which approximately 50% is accounted for by sterilization. The moderate 29–35% reliance on modern reversible methods could mean that abortion is also being used to space births to reach the total fertility rate of 2.2 children per woman in South America and 2.4 elsewhere in the region.Citation15
The unsafe abortion rate for Asia is estimated at 11 per 1,000 women aged 15–44 years in 2008. Estimates for Asia as a whole include the demographically large region of Eastern Asia, where safe abortion is generally available. The South-Central Asia sub-region has the highest number of unsafe abortions of any subregion, owing to the size of its population. In 2008, more than 6.8 million unsafe abortions, or 17 per 1,000 women of reproductive age are estimated to have taken place in the South-Central region, which poses a formidable challenge. India, the most populous country in the region, legalized abortion in 1971; however, it is recognized that some two-thirds of all abortions still take place outside the authorized health services,Citation28 contributing large numbers of unsafe abortions. These numbers are unlikely to decrease until women become better informed about their right to legal and safe abortion, and where to find safe abortion (including effective medical abortion regimens) and post-abortion care, particularly the millions of poor and young women. In addition, reversible contraceptive prevalence in the sub-region is moderate at 54% and two-thirds of contraceptive use is of female sterilization. As in Latin America, the high incidence of (unsafe) abortions is probably due to women's need to space births before having a sterilization. Among Asia's sub-regions, South-Eastern Asia has the highest unsafe abortion rate at 22 per 1,000 women aged 15–44 years. Only 8% of couples in this sub-region rely on traditional methods while 53% use modern, mostly reversible, family planning methods (47%). It appears, though, that abortion is used to keep fertility at 2.3 children per woman.
The total fertility rate of Western Asia is 2.9 children per woman and the contraceptive prevalence is 54%, of which more than one in three are users of traditional methods, which signals a shortfall of modern contraceptives. The estimated unsafe abortion rate for Western Asia is 16, lower than that for the Northern Africa sub-region, which has a similar total fertility rate and contraceptive prevalence, though modern contraceptive use is higher in Northern Africa at 45%.
The low level of unsafe abortion long seen in some European sub-regions appears to have further reduced in 2008 compared to 2003; only in the Eastern European region are unsafe abortions still identifiable, i.e. in Poland where the law has severely restricted access and barriers to safe abortion have increased.Citation29 Unsafe abortion numbers for Russia, the most populous country in the region, are difficult to assess and numbers for the Eastern Europe sub-region could therefore be higher than indicated, especially since socially indicated and late abortions were legally restricted several years ago. The less reliable (or under-estimated) number of unsafe abortions in Russia may have a major impact on the East European regional estimate because of its large population size.
While it is acknowledged that there is a problem of unsafe abortion in Oceania, excluding Australia and New Zealand, data are exceptionally scant and, as a consequence, estimates are imprecise. However, Oceania seems unlikely to attain a total fertility rate below 4 children per woman with a low contraceptive use of 27% (21% for modern methods) and as few as 8 unsafe abortions per 1,000 women; the rate of unsafe abortions could therefore be much higher.
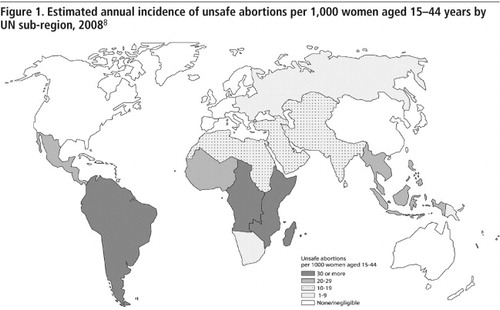
The map in gives an overview of unsafe abortion rates in sub-regions and shows that the rates are the highest in South America and in the regions across the belt of Africa. Unsafe abortion features prominently in all developing regions, however, with the exception of Eastern Asia. Southern Africa shows the lowest range of abortion rates. By comparison, in developed regions unsafe abortions are found only in the Eastern European region.
All countries vs. countries with evidence of unsafe abortion
Some regions and countries show no or little evidence of unsafe abortion, while there are others where some or all abortions are undoubtedly unsafe. In still others, small or large numbers of unsafe abortions co-exist with safe abortions, e.g. in India. Some unsafe abortions take place in countries in transition to full implementation of abortion law reform intended to make abortions safe, such as Cambodia, South Africa, Ethiopia, and Nepal. In others, safe abortion may be widely available, but due to barriers such as poor access, cost, restrictive regulations such as parental consent, lack of confidentiality and/or social reasons, women may resort to unsafe abortion.
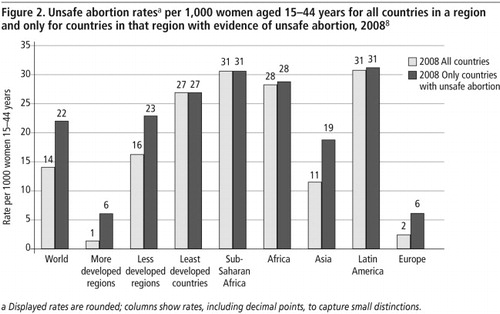
Rates shown in Table 1 were calculated to include all countries in each region whether or not there was any evidence of unsafe abortion. For 2008, estimates were also derived solely for the countries in the region with evidence of unsafe abortion, which is probably a more meaningful indicator, especially for regions such as Asia and Europe which include demographically large sub-regions with safe abortions. Two set of estimates were made: (1) for all countries in a sub-region (as shown in Table 1); and (2) for countries of that sub-region with evidence of unsafe abortion, thereby excluding from the denominator of both abortion rates per 1,000 women and abortion ratios per 100 live births the population of countries where there is no evidence of unsafe abortion. With a smaller but more appropriate denominator the unsafe abortion rates are higher, providing a better reflection of the global situation of unsafe abortion ().
The global rate of unsafe abortion increases dramatically from 14 to 22 per 1,000 women aged 15–44 as this figure shows, and in less developed regions it becomes 23 with countries of Eastern Asia and others with safe abortion excluded. When countries with no evidence of unsafe abortion are excluded for the more developed regions, the unsafe abortion rate goes up from 1 to 6 per 1,000 women aged 15–44 years. For the least developed countries and sub-Saharan Africa the two rates coincide, as abortion is highly restricted legally and most abortions are classified as unsafe. The small differences for Africa and Latin America are due to abortion being legal and on request in Tunisia and Cuba, respectively.
Trends in unsafe abortion: 2003–2008
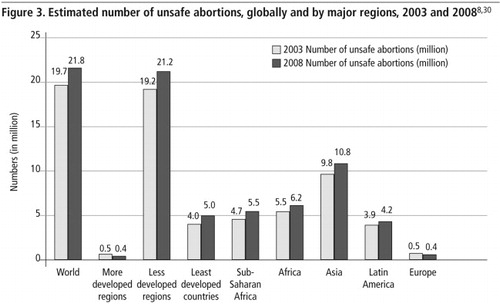
The numbers of unsafe abortions increased from 19.7 million in 2003 to 21.6 million in 2008 () but the overall unsafe abortion rate has remained the same. The increase in numbers is because of the growth in the population of women aged 15–44, from 1,465,354,000 in 2003 to 1,553,217,000 in 2008.Citation15
Numbers are slightly higher in all regions in 2008; however, the largest population increases are in the least developed countries, sub-Saharan Africa and the Africa region as a whole, where the number of women of reproductive age grew most rapidly. In Asia, unsafe abortions increased by approximately one million, while in Latin America the increase between 2003 and 2008 was modest. captures the magnitude of the problem in different regions of the world. However, regional and time trends can be gleaned better with the standardized measure of abortion rates.
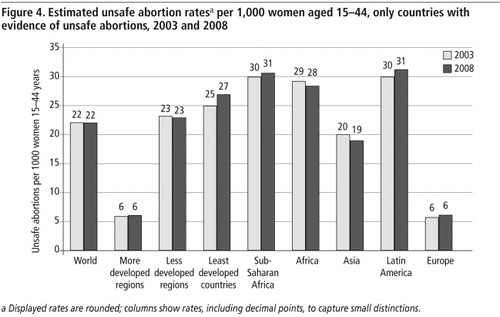
Global, regional and sub-regional rates () are based only on countries in the regions with evidence of unsafe abortion. There was little change in the unsafe abortion rates for the major regions between 2003 and 2008 (); however, the contrast between developing and developed regions is striking – from over 30 per 1,000 women aged 15–44 years in sub-Saharan Africa and Latin America to 20 per 1,000 in Asia (excluding Eastern Asia), to 6 per 1,000 for the more developed regions, represented only by Eastern Europe. The unsafe abortion rate for Africa was slightly lower in 2008 than in 2003, mainly because of a decline in Southern and Northern Africa ().
Trends by sub-region
The average represented by global rates and the grouping of rates by continent absorbs the differentials found between sub-regions, yet these distinctions are important. Modest reductions in unsafe abortion rates were found in 2008 as compared to 2003Citation30 in most sub-regions (). The upward changes in rates, notably for Middle Africa, Western Asia and Central America, were due to better coverage and more reliable information in 2008 than in 2003. Limitations in the 2003 data were pointed out for these regions when they were published in 2007; former cautious estimates turn out largely to have been underestimates. The highest rates for any sub-region in 2008 were in Eastern and Middle Africa at 36 per 1,000 women 15–44. Nevertheless, there was a reduction for Eastern Africa from 39 in 2003, while the 2008 rate for Middle Africa adjusts the underestimated figure for 2003. In Western Africa, the rate was slightly lower at 28 at both points in time. For both Northern and Southern Africa, there were substantial improvements: from 22 and 14 per 1,000 in 2003 down to 18 and 9 per 1,000 in 2008, respectively.
In South-Central Asia there was a modest reduction from 18 per 1000 in 2003 to 17 per 1,000 women aged 15–44 in 2008, which is actually one of the lowest rates among the sub-regions with unsafe abortions; however, it is a significant drop because of the huge population it applies to. The South-Eastern Asia region shows the highest rates (in the high 20s) among the Asian sub-regions both in 2003 and in 2008 (Viet Nam and Singapore, where abortion is legal, are excluded). Better and more complete data for Western Asia produced a noticeably higher rate than in 2003, though it remains modest. Eastern Asia has no or negligible unsafe abortion and is not shown in .
The rate in 2008 for South America is lower than in 2003, continuing a trend seen since 2000, which shows that unsafe abortions are consistently decreasing in that region. As indicated earlier, Central America and the Caribbean have equally high unsafe abortion rates (Cuba and Caribbean islands where induced abortion is legal and safe are excluded).
Discussion
In spite of major increases in contraceptive uptake and significant advances in safe abortion technologies, unsafe abortions continue to occur in much of the developing world, killing and injuring many women each year. When contraceptive services are unable to meet the demand for family planning, and when contraception fails, women and couples turn to abortion to regulate their fertility. Where access to safe abortion is restricted, women are forced to rely on unskilled providers or use methods and drugs without clinical support.
Based on 2007 data on contraceptive prevalenceCitation26 and the typical failure rates of contraception, it has been estimated that approximately 33 million women each year will experience an unintended pregnancy while using a contraceptive method.Citation30 In addition, the contraceptive needs of at least 110 million married women with unmet need for family planning and over 400 million unmarried women of reproductive age, including adolescents, are poorly addressed.
However, contraception alone cannot and will not reduce women's need for abortion, which is as much a part of women's life experience as their ability to become pregnant. At a minimum, safe abortion services should be accessible in every country to the full extent of the law. However, it remains vital that countries, inter-governmental and non-governmental organizations address unsafe abortion as a major public health concern. Where legal, social and political norms restrict and criminalize abortion, women nevertheless continue to seek abortion, even at the risk of their health and lives. The numbers of unsafe abortions will not fall unless women's access to safe abortion and effective family planning services is greatly improved, most urgently in the countries where they are least accessible, affordable and available.
We hope the information presented in this paper will assist informed discussion of unsafe abortion around the globe and lead to concerted efforts to make all abortions safe.
Note
The authors alone are responsible for the views expressed in this paper, they do not necessarily represent the decisions, policy or views of the World Health Organization.
Acknowledgements
The authors are most grateful to Svetlin Kolev for drawing the map in .
Notes
References
- World Health Organization. The prevention and management of unsafe abortion: report of a technical working group. (WHO/MSM/92.5). 1992; WHO: Geneva.
- World Health Organization. Safe abortion: technical and policy guidance for health systems. 2003 and forthcoming; WHO: Geneva.
- L Ramachandar, PJ Pelto. Medical abortion in rural Tamil Nadu, South India: a quiet transformation. Reproductive Health Matters. 13(5): 2005; 54–64.
- CC Harper, K Blanchard, D Grossman. Reducing maternal mortality due to elective abortion: potential impact of misoprostol in low-resource settings. International Journal of Gynecology and Obstetrics. 98(1): 2007; 66–69.
- S Miller, T Lehman, M Campbell. Misoprostol and declining abortion-related morbidity in Santo Domingo, Dominican Republic: a temporal association. BJOG: an International Journal of Obstetrics and Gynaecology. 112(9): 2005; 1291–1296.
- J Sherris, A Bingham, MA Burns. Misoprostol use in developing countries: results from a multicountry study. International Journal of Gynecology and Obstetrics. 88(1): 2005; 76–81.
- S Singh. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. Lancet. 368(9550): 2006; 1887–1892.
- World Health Organization. Unsafe abortion. Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. 2010; WHO: Geneva.
- JJ Llovet, S Ramos. Induced abortion in Latin America: strategies for future social research. Reproductive Health Matters. 6(11): 1998; 55–65.
- S Singh, E Prada, F Mirembe. The incidence of induced abortion in Uganda. International Family Planning Perspectives. 31(4): 2005; 183–191.
- S Singh, E Prada, E Kestler. Induced abortion and unintended pregnancy in Guatemala. International Family Planning Perspectives. 32(3): 2006; 136–145.
- S Singh, D Wulf. Estimated levels of induced abortion in six Latin American countries. International Family Planning Perspectives. 20(1): 1994; 4–13.
- Huntington D. Abortion in Egypt: official constraints and popular practices. Paper presented at IUSSP Seminar on Cultural Perspectives on Reproductive Health, Rustenburg, South Africa, 16–19 June 1997.
- D Ferrando. El aborto inducido en el Peru. Hechos y cifras. 2002; Centro Flora Tristan and Pathfinder International: Lima.
- UN Department for Economic and Social Information and Policy Analysis. World population prospects: the 2008 revision. 2009; UN: New York.
- AJ Wilcox, LF Horney. Accuracy of spontaneous abortion recall. American Journal of Epidemiology. 120(5): 1984; 727–733.
- EF Jones, JD Forrest. Under-reporting of abortion in surveys of US women: 1976 to 1988. Demography. 29(1): 1992; 113–126.
- RJ Udry, M Gaughan, PJ Schwingl. A medical record linkage analysis of abortion underreporting. Family Planning Perspectives. 28(5): 1996; 228–231.
- BA Anderson, K Vatus, A Puur. The validity of survey responses on abortion: evidence from Estonia. Demography. 31(1): 1994; 115–132.
- RK Jones, K Kost. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Studies in Family Planning. 38(3): 2007; 187–197.
- M-J Osis, E Ardí, A Faúndes. Dificuldades para obtener informações da população de mulheres sobre aborto ilegal. Revista de Saúde Pública. 30(5): 1996; 444–451.
- TE Canto de Cetina, CE Colven, JM Hernández Cano. Aborto incompleto: características de las pacientes tratadas en el Hospital O’Horan de Merida, Yucatán. Salúd Pública de México. 27(6): 1985; 507–513.
- H Fu, JE Darroch, SK Henshaw. Measuring the extent of abortion underreporting in the 1995 National Survey of Family Growth. Family Planning Perspectives. 30(3): 1998; 128–133, 138
- C Moreau, N Bajos, J Bouyer. Question comprehension and recall: the reporting of induced abortions in quantitative surveys on the general population. Population (English ed.). 3–4: 2004; 439–454.
- V Rasch. Self-reports of induced abortion: an empathetic setting can improve the quality of data. American Journal of Public Health. 90(7): 2000; 1141–1144.
- United Nations Population Division. World Contraceptive Use 2007. 2009; UN: New York.
- PK Streatfield. Role of abortion in fertility control. Journal of Health, Population and Nutrition. 19(4): 2002; 265–267.
- Ministry of Health & Family Welfare, India. Annual report 2006–2007. 2008; MoHFW, Government of India: New Delhi.
- W Nowicka. Reproductive rights in Poland. 2008; Federation for Women and Family Planning: Warsaw.
- World Health Organization. Unsafe abortion. Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003. 5th ed. 2007; WHO: Geneva.