Abstract
This study assessed trends in equity of access to reproductive health services and service utilization in terms of coverage of family planning, antenatal care and skilled birth attendance in Thailand. Two health indicators were measured: the prevalence of low birthweight and exclusive breastfeeding. Equity was measured against the combined urban–rural areas and geographic regions, women's education level and quintiles of household assets index. The study used data from two nationally representative household surveys, the 2006 and 2009 Reproductive Health Surveys. Very high coverage of family planning (79.6%), universal antenatal care (98.9%) and skilled birth attendance (99.7%), with very small socioeconomic and geographic disparities, were observed. The public sector played a dominant role in maternity care (90.9% of all deliveries in 2009). The private sector also had a role among the higher educated, wealthier women living in urban areas. Public sector facilities, followed by drug stores, were a major supplier of contraception, which had a high use rate. High coverage and low inequity were the result of extensive investment in the health system by successive governments, in particular primary health care at district and sub-district levels, reaching universality by 2002. While maintaining these achievements, methodological improvements in measuring low birthweight and exclusive breastfeeding for future reproductive health surveys are recommended.
Résumé
Cette étude a analysé l'évolution de l'équité de l'accès aux services de santé génésique et l'utilisation des services avec la couverture de la planification familiale, les soins prénatals et l'assistance qualifiée à l'accouchement en Thaïlande. Deux indicateurs sanitaires ont été examinés : la prévalence de l'insuffisance pondérale à la naissance et l'allaitement exclusivement au sein. L'équité a été mesurée par rapport aux données combinées des régions géographiques et des zones urbaines-rurales, au niveau d'instruction des femmes et aux quintiles de la richesse des ménages. L'étude a utilisé les informations de deux enquêtes auprès des ménages représentatives à l'échelon national : les enquêtes de santé génésique de 2006 et 2009. Elle a observé une très vaste couverture de la planification familiale (79,6%), la généralisation des soins prénatals (98,9%) et de l'assistance qualifiée à l'accouchement (99,7%), avec très peu de disparités géographiques et socio-économiques. Le secteur public jouait un rôle prédominant dans les soins obstétricaux (90,9% des accouchements en 2009). Le secteur privé apportait aussi sa contribution pour les femmes les plus instruites et vivant dans les zones urbaines. Les centres du secteur public, suivis des pharmacies, représentaient une source majeure d'approvisionnement en contraception orale, largement utilisée. La couverture élevée et les faibles inégalités résultent d'investissements considérables réalisés par les gouvernements successifsdans le système de santé, en particulier les soins de santé primaires au niveau du district et du sous-district, qui sont devenus universels en 2002. Tout en maintenant ces progrès, il est recommandé d'apporter desaméliorations méthodologiques aux mesures de l'insuffisance pondérale à la naissance et de l'allaitement exclusif pour les futures enquêtes de santé génésique.
Resumen
Este estudio evaluó las tendencias en equidad de acceso a los servicios de salud reproductiva e infantil y en el uso de estos con relación a la cobertura de planificación familiar, atención antenatal y atención calificada del parto en Tailandia. Se midieron dos indicadores de salud: prevalencia de bajo peso al nacer y lactancia exclusiva. Se midió la equidad contra las zonas urbanas-rurales y las zonas geográficas, el nivel de escolaridad de las mujeres y los quintiles del índice de bienes. Se utilizaron datos de dos encuestas domiciliarias nacionalmente representativas: las Encuestas de Salud Reproductiva de 2006 y 2009. Se observó una cobertura muy alta de los servicios de planificación familiar (79.6%), atención antenatal universal (98.9%) y atención calificada del parto (99.7%), con muy pequeñas diferencias socioeconómicas y geográficas. El sector público desempeñó una función dominante en la atención obstétrica (el 90.9% de todos los partos en 2009). El sector privado también desempeñó un rol entre las mujeres más cultas y con mayores recursos financieros que viven en las zonas urbanas. Las unidades de salud del sector público, seguidas por las farmacias, fueron uno de los principales proveedores de anticonceptivos, cuya tasa de prevalencia de uso fue elevada. La alta cobertura y la baja inequidad fueron el resultado de extensas inversiones en el sistema de salud por parte de sucesivos gobiernos, en particular en la atención primaria a nivel distrital y sub-distrital, alcanzando universalidad para el año 2002. A la vez que se mantienen estos logros, se recomienda mejorar la metodología para medir el bajo peso al nacer y la lactancia exclusiva para futuras encuestas de salud reproductiva.
Equity in access to reproductive health (RH) services has been adopted internationally under the Millennium Development Goals.Citation1 In Thailand, the whole range of RH services are provided in a comprehensive manner, while a draft law on RH protection was under discussion by stakeholders.Citation2 Universal coverage of these services, free at the point of care, was reached by 2002 for the entire population.Citation3Citation4
In the 2006 Multi-Indicator Cluster Survey (MICS), it was learned that underweight children and stunting in Thailand were disproportionately concentrated among the poor and those living in rural areas. The risk ratio between the top and bottom wealth quintiles and between the urban and rural areas ranged from 0.24 and 0.52 for child underweight to 0.34 and 0.66 for child stunting, respectively. Utilization of basic maternal and child health (MCH) interventions were almost equitable with a very small rich–poor and urban–rural gap observed. Antenatal care and delivery by a skilled health worker or in a health facility had a modest pro-rich coverage. The ratio of the service coverage between richest and poorest quintiles was 1.05 for antenatal care and 1.10 for skilled and facility-based delivery. The most equitable coverage was in the use of modern contraceptive methods (rich–poor ratio, 0.99) and child immunization (rich–poor ratios, 0.91–0.99). All undesirable health outcomes prevailed more among the rural than urban residents, whereas MCH coverage had a small gap. Education of women or caregivers was a major determinant of MCH inequity, and the subgroup with no education shared the burden more than the most educated in all outcome indicators. For example, the risk ratio for teen pregnancy and child stunting between those with higher education and those with no formal education was 0.10 and 0.29, respectively.Citation5
Despite the high level of reproductive and child health service coverage, progress towards reducing maternal mortality has been affected over the last two decades by the HIV epidemic, starting in the 1990s. The maternal mortality ratio (MMR) according to WHO data was 50 per 100,000 live births in 1990 and 63 in 2000, and then dropped to 48 in 2008. AIDS contributed to 23.1% of total maternal deaths in 2008.Citation6
Since 1975, the National Statistical Office of Thailand has periodically conducted a Reproductive Health Survey, a nationally representative, structured, face-to-face, interview-based household survey. These are an important means for evaluating progress towards the MDG goal of universal access to reproductive health. The two most recent surveys were in 2006 and 2009.
This study assessed the extent of progress in Thailand between 2006 and 2009 in equity of reproductive and child health outcomes and service utilization. First, prevalence of low birthweight was a measure of maternal health outcome and coverage of exclusive breastfeeding was a measure of child health. Low birthweight, a determinant of long-term, adverse outcomes from cardiovascular diseasesCitation7 in adult life, and the protective benefit of exclusive breastfeedingCitation8 for child health were selected for analysis, as previous evidence from the Multi- Indicator Cluster Survey 2006 showed that these were major reproductive and child health challenges in Thailand.Citation5 Second, equity in service utilization among Thai women of reproductive age was measured by coverage of family planning (FP), antenatal care (ANC), and skilled birth attendance (SBA). Equity in health outcomes and service coverage were determined against women's economic status, education and geographic location.
Methods
For the 2006 Reproductive Health Survey, 56,658 women aged 15–49 years and for the 2009 survey 37,511 women aged 15–59 years were interviewed. Based on a stratified two-stage sampling, the surveys covered all 76 provinces of Thailand, each stratified between urban (municipal) and rural (non-municipal) areas.
In the interviews, the following questions were asked:
| • | FP: “Are you or your husband/partner using any family planning?”; “Which family planning are you mostly using?”; “Where do you get family planning services?” | ||||
| • | ANC: “Did you receive any antenatal care services when you had your last child?” | ||||
| • | Delivery: “Who assisted with the delivery of your last child?” and “Where did you deliver the last birth?” | ||||
| • | Low birthweight infants: “How much did your last child weigh when he/she was delivered?” For 2006, the birthweight in grams was reported by mothers or caregivers, whereas for 2009, birthweight as recorded on the birth certificate or the immunization record card (pink book) were requested for inspection by the interviewers in order to increase the accuracy of surveyed birthweights. | ||||
| • | Exclusive breastfeeding for 2006: “During the last 24 hours, did you breastfeed without giving water or any food?” “Is your child breastfed currently?” For 2009, detailed questions were asked: “In the last 24 hours, did you also give the following to your child: (a) vitamins or mineral supplements/medicines, (b) plain water, (c) juice, fruit juice, tea, (d) oral re-hydrating solution, (e) instant food, (f) condensed milk, fresh milk, powdered milk, (g) other drinks, porridge soup, (h) other solid food, crushed banana and porridge?” Each of these (b to h) must be responded to with “no”, in order to firmly conclude breastfeeding was exclusive. | ||||
To make the estimates comparable between the two surveys, service coverage was calculated as the number of women receiving the service proportional to all women aged 15–49 who were eligible for these services. Although for 2009, women aged 15–59 years were interviewed, for the purposes of this study, we selected only women aged 15–49 years for analysis.Footnote*
Assessment of equity was based on the following characteristics of women and households: level of woman's education, quintiles based on household asset index and the combined urban–rural areas and geographic regions of Thailand. To compute the household asset index, the presence of selected assets and durables in households was used. These included housing materials, toilet, transportation, and electrical equipment. Households with these assets were considered better off economically than those without. The asset index is the weighted sum of these household assets, with weights derived from principal components analysis.Citation9 The 2006 survey did not contain questions on ownership of household durables; hence, the asset index for 2006 was not available.
Findings
General characteristics
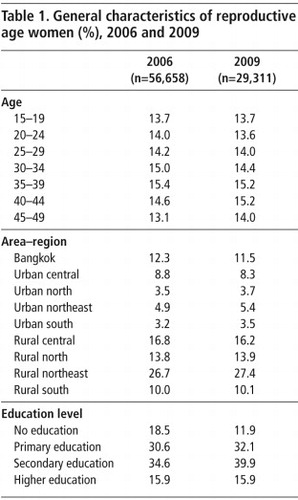
Using the individual sampling weights of the RHS, the total numbers of women in the population aged 15–49 years in Thailand for the years 2006 and 2009 were estimated, 18.7 and 18.8 million respectively. Age distribution between the two surveys was almost homogeneous (Table 1
). Rural residents were a majority, and over a quarter of all reproductive age women lived in the rural northeast region. Over the three-year period, women educated post-primary school increased from 50% to 56% and the uneducated dropped sharply from 18% to 12%.Coverage of reproductive health services
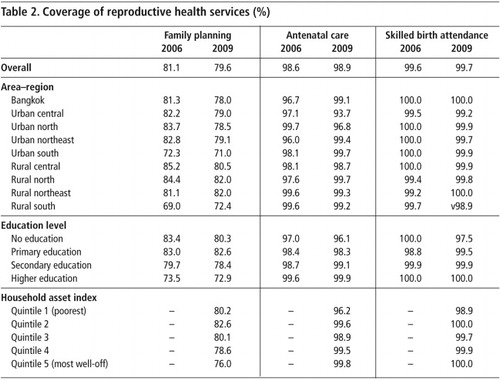
The national contraceptive prevalence rate was around 80% for both years, and antenatal care and skilled birth attendance coverage was over 99% (Table 2
).As a result of very high and stable coverage, services were distributed equally between urban and rural areas and across geographic regions, except for the rural–south region which had lower than average family planning coverage.
With regard to socio-economic factors, the coverage gaps between the higher educated and low or uneducated women were very narrow, in particular for ANC and SBA (97% to 100%). However, a reverse gap in contraceptive prevalence rate was observed, namely, higher rates of 80–83% among the uneducated and a lower rate of 73% among the higher educated women.
There was a minimal rich–poor gap, as measured by the household's asset index for ANC and SBA, though a small reverse gap for contraceptive prevalence rate was also observed. Higher rates among poorer women and lower rates among richer women were probably due to differences in age composition and demands for fertility control between the different classes.
Services and providers attended
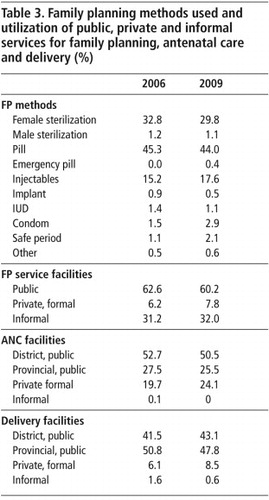
The choices of contraceptive methods were relatively consistent between 2006 and 2009. Almost half of women (44–45%) used contraceptive pills. Female sterilization and injectables were the second and third most common choices, used by 30–33% and 15–18% of women, respectively (Table 3
).FP services were obtained from public facilities by 60–63% of women, including from health centres, district hospitals and provincial hospitals. However, the private sectors, including drug stores and other informal private providers, such as village health volunteers and other small outlets, accounted for about one-third of total choices. Public health care facilities at the provincial and district levels played a significant role in service provision for ANC (76–80%) and delivery (91–92%) services.
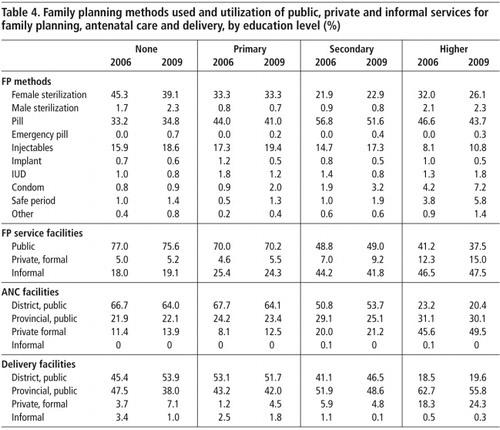
Choice of FP method varied according to the education level of the users (Table 4
). Female sterilization was popular among uneducated and primary-level educated women, whereas use of the contraceptive pill was more prevalent among secondary and higher educated counterparts. More use of injectables among lower educated women was also observed. Public facilities were the major FP providers for women with no education and primary education, whereas the private sector served more for the higher educated women.Similarly, the women with up to primary education relied on the district-level facilities for ANC and delivery services. The private sector provided ANC and delivery care to less than 8–14% of the women who had achieved below secondary schooling. The women with post-secondary school education received 2–3 times more ANC and delivery care from private providers than their less educated counterparts.
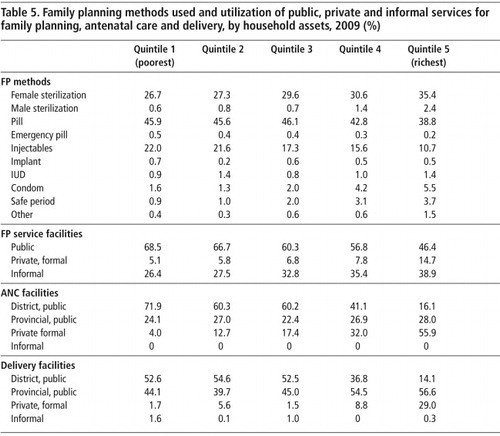
With respect to household economic status, the 20% richest women (the top asset quintile) chose female sterilization as a method more than those who were poorer (Table 5
). Use of contraceptive pills and injectables was more popular among women in the lower asset quintiles. The women in economically better-off households chose FP, ANC and delivery services from the private sector, whereas those in the poorer quintiles received the services more from the public providers.Low birthweight and exclusive breastfeeding
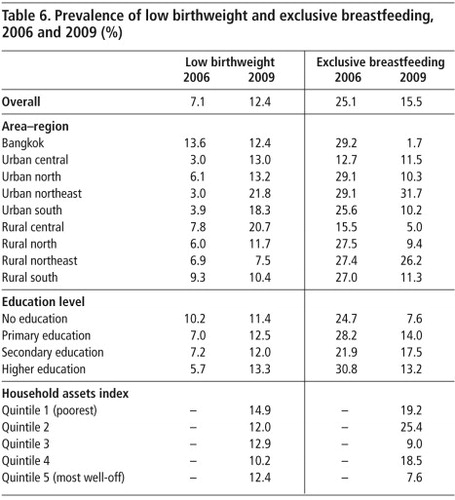
The overall prevalence of low birthweight infants was 7.1% in 2006 but 12.4% in 2009, a rise that might be explained by the difference in how the data were collected, with the 2009 figures likely to be more accurate (Table 6
). The implication – that one in eight pregnant women has poor health, poor enough that the baby's health is also compromised – is worrying and needs attention.Distribution in the prevalence of low birthweight across urban–rural areas and geographic regions was inconsistent over time. In 2006, Bangkok was the highest prevalence (13.6%) area–region, whereas in other regions, except for the north, the low birthweight prevalence in rural areas was double that of urban areas. In 2009, the low birthweight prevalence decreased in Bangkok but increased in all other regions. In addition, except for the central region, the urban areas had a higher prevalence than their rural counterparts.
With respect to education level, an uneducated or lower educated woman in 2006 was more likely to have a low birthweight baby. The picture in 2009 was quite different; the prevalence of low birthweight among higher educated women was higher than among the lower educated. In 2009, women living in the poorest quintile households had a higher prevalence of low birthweight than the economically better-off quintiles.
The rate of exclusive breastfeeding in 2006 was 25.1%, which dropped by almost 10 percentage points by 2009 to 15.5% (Table 6). Again, given the change in how the question was asked, it may be that the figure for 2009 is more accurate, because more detail was provided, or it could be that breastfeeding alternatives were being promoted more by 2009, or mothers were not in a position to breastfeed exclusively as often. This would require qualitative research and data from a further survey to measure against.
Across different areas–regions, Bangkok experienced a sharp drop in the prevalence of exclusive breastfeeding from 29% in 2006 to less than 2% in 2009. Other area–regions with a sharp drop included the urban and rural north, the urban and rural south, and the rural central regions. A reduction in the prevalence of exclusive breastfeeding occurred at every level of women's education, although the uneducated women experienced a relatively larger decline. With respect to economic quintiles, there was no clear gradient pattern; exclusive breastfeeding was relatively higher for the poorer quintiles (1 and 2) and quintile 4 and relatively lower for quintiles 3 and 5 (richest).
Discussion
Universal coverage supports equitable access
In the MDG tracking, by 2010 all health-related MDGs in Thailand were fully achieved.Citation10 The 2008 maternal mortality ratio (MMR) estimated by WHO, UNICEF, UNFPA and the World BankCitation10 for Thailand was 48 per 100,000 live births, with a range of uncertainty between 32 and 68. That report noted that AIDS contributed to 23.1% of the total 470 maternal deaths in the same year.
Despite the high coverage of reproductive health services, there are a number of remaining challenges: the need to reduce maternal mortality due to AIDS, the low level of exclusive breastfeeding, and the prevalence of low birthweight. There was an increase in the prevalence of births to adolescents (ages 11–19 years), from 12.5% of the total in 1996 to 16.1% in 2009.Citation11 This paper contributes to global policy debates on how reproductive and child health interventions can be improved, by taking into account the equity gaps across different socio-economic and geographic groups and what has caused them, such as malnutrition.
Near universal ANC (98.6% in 2006 and 98.9% in 2009) and universal SBA (99.6% in 2006 and 99.7% in 2009) were confirmed by this study. There is almost zero inequity across geographic areas, women's level of education and household wealth. This confirms the assertion by Houweling et alCitation12 of the negative correlation between health service coverage and the rich–poor gap; the higher the coverage, the lower the rich–poor inequity will be. However, there are still poor people in Thailand and the existence of low birthweight in infants, with the implied poor health in their mothers, is indicative of the need to address the social determinants of health, which health services cannot do on their own.
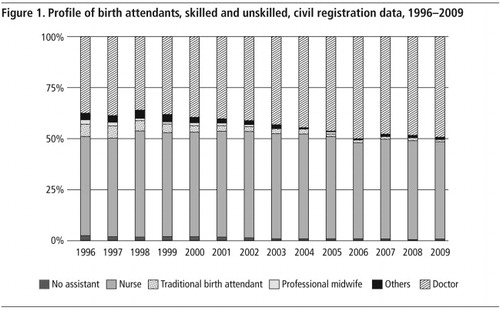
The near universal SBA coverage reported by this study confirms data from the national birth registration records, which are part of the mandatory national civil registration of births and deaths, and cover more than 98% of total births in Thailand.Citation13 In
the proportion of non-assisted deliveries as recorded in birth registration fell from 2.7% in 1996 to 0.5% in 2009. The SBA coverage in 2009 was 99.5%, in which as many doctors as nurses attended births, 49.2% and 48.3% respectively, in total birth attendance. Traditional birth attendants were already few by 1996 and had also almost disappeared by 2000. Midwives per se played only a small role, as today there is no stand-alone midwifery training. Nursing and midwifery have been integrated into the nurse-and-midwifery curriculum for professional nurses since 1975.Citation14 The last cohort of midwives will reach retirement age in a few years.
The contraceptive prevalence rate was maintained at a high level of 81.1% in 2006 and only slightly dropped to 79.6% in 2009, demonstrating the high level of public awareness of FP on the demand side, as well as the capacity of public and private providers to deliver the services as needed. Although FP services are free and universally available from public sector providers, these providers cater mainly for the rural population, who are mostly poor, while the private sector is the provider of choice for well-off urban women, who pay for the services, mostly from drug stores, which played a major role in contraceptive pill provision, classified in this paper as part of the informal private sector.
The Thai health system: a major contributor to universal coverage
Universal reproductive health services had been covering the entire population well before the implementation of Universal Health Coverage in 2002. This is the result of commitments by successive governments since the 1970s in investing in the health of the population, when consistent favourable economic growth was the main determinant of health infrastructure development.Citation15 Huge investment in the district health system and efforts to protect the poor and underprivileged from catastrophic health care costs, through targeted approaches since 1975 until the universal coverage policy in 2002, contributed significantly to health outcome achievements in both level and distribution.Citation16Citation17
Functioning primary health care services were an outcome of the national policy on rural health infrastructure extension to all sub-districts and districts, and on compulsory working in rural health services by all medical and nursing graduates since the 1970s. The district health system serves as a “close-to-patient” service hub which was more accessible to the rural poor majority. Not only was a high coverage of MCH services evident, but the 98% immunization coverage of DTP3 was sustained for the last two decades.Citation18
With the application of policy analysis, the experience of the Thai national FP programme was compared with that of the Philippines (together with three other pairs: Bangladesh and Pakistan, Tunisia and Algeria, Zimbabwe and Zambia). The formation of coalitions among policy elites, spread of policy risk, allocation of adequate resources, and institutional and financial stability were factors enabling the adoption and sustainability of strong population policies and FP programmes.Citation19
A reverse inequity in the FP services, whereby the poorer and lower educated women had a higher contraceptive prevalence rate (80–83%) than their richer and higher educated counterparts (73%), can be explained by the higher demand for fertility regulation and the relatively younger age of this group, or the higher income women belonging to an older age group.
Interestingly, the private sector played a role in FP and ANC services but not in delivery (see Table 3). This is witnessed by the affordable private FP and ANC services and more convenient opening hours. Public facilities provide these services during the daytime, while curative, emergency and accident services were 24-hour services. In contrast, the public sector is the dominant provider of delivery services in rural areas, where 70% of the population lives. The high confidence in the quality of public sector delivery servicesCitation20 results in the high level of public hospital delivery.
The low contraceptive prevalence rate, especially in the southernmost Muslim majority provinces, was carefully scrutinized. The Reproductive Health Survey showed that 52.4% of Muslim women in 2006, and 56.8% in 2009 were using a contraceptive method. This was higher than the rate of Christian and Buddhist women in the same areas. Only 3.2% of Muslim women were not practising contraception due to religious reasons. The low use rate was rather the result of armed conflict and insecurity.
Methodological issues
A few methodological weaknesses in the Reproductive Health Survey were identified through this study. First, the low birthweight prevalence in 2006 seems to be unrealistically low due to recall or other bias in reporting the birth weight in grams by mothers or caregivers. Eyewitness by the NSO interviewers in the 2009 survey of the birth weight as recorded on the birth certificate is a more reliable method. An actual increase in the low birthweight prevalence from 7.1% in 2006 to 12.4% in 2009 is unlikely, because there were no major adverse events to cause such a rapid change during this short, three-year period. The Asian economic crisis in 1997–1998Citation21 was too remote to have had such an impact in those years. However, the prevalence of low birthweight in 2009 based on the birth registration records of 9.6% (range across the 76 provinces across the country of 8%–13.2%) compared to 12.4% in the 2009 Reproductive Health Survey is a major discrepancy, which warrants further in-depth investigations.
Second, exclusive breastfeeding referred to infants who received only breastmilk and vitamins, mineral supplements and medicines during the last 24 hours. The 2006 survey did not apply a standard questionnaire as the 2009 survey did. As a result, the prevalence of 25.1% in 2006 is unreliably high. The figure of 15.5% in the 2009 survey should be more reliable. However, the 2006 MICS, based on a similar definition to the one applied in the 2009 Reproductive Health Survey, reported 5.4% exclusive breastfeeding among children below 6 months old. There was therefore progress in the prevalence of exclusive breastfeeding between 2006 and 2009.
Third, the face-to-face interview used in the Reproductive Health Survey may limit the accurate measurement of unmet need for FP services; it is embarrassing and socially stigmatising to ask unmarried adolescents about their use of contraception. A self-administered questionnaire survey would be a better approach.
Fourth, we used point estimates without statistically bound uncertainty for calculating the prevalence and coverage in this study. Finally, the Reproductive Health Survey only captures the native Thai population (64 million). The non-Thai highlanders in the Northern mountainous areas (approximately 0.5 million) and migrant workers (approximately 1 million women migrants) were not enumerated by the survey. Their reproductive health needs and coverage are not well captured by this survey.
The use of the household asset index in 2009 as the equity stratifier was a major strength of this study. The asset index quintiles have been commonly applied in the equity analysis with respect to an economic gradient, for example in an assessment of unwanted births and contraceptive use between rich and poor women in 41 countries.Citation22
Recommendations
In future Reproductive Health Surveys, a standard definition of exclusive breastfeeding must be strictly followed and applied to children under six months. Accuracy in recording this from the birth certificates is essential, as respondents' recall is less reliable. The measurement of unmet need for family planning services among adolescents and young people should also be improved.
Thailand has benefited from steady economic growth and government commitment to human development to achieve the MDGs early. The equitable access to MCH services is a result of wide geographic coverage of well-functioning primary health care, especially at the district and sub-district levels. The adoption of the principle of universality is a major contributor to the achievement of the health-related MDGs. Accurate measurement of low birthweight and exclusive breastfeeding requires methodological improvements in the survey. Investment in the health sector and in extending coverage of reproductive and child health services, while crucial, are not sufficient on their own. Effective policy interventions addressing the social determinants of ill-health, such as poverty, gender inequity, teenage and unplanned pregnancies, unmet need for contraceptive services among unmarried adolescents and young people, and other social inequity, are equally important.
Acknowledgements
The valuable institutional relationship between the National Statistical Office and the Ministry of Public Health is a key platform for improving national household surveys in responses to policy demands for monitoring progresses towards health-related MDG. We acknowledge their contributions to producing the 2006 and 2009 Reproductive Health Surveys, and the different development partners and the Ministry of Public Health who contributed to the design of the 2009 survey. The inclusion of standard parameters to facilitate the computation of the household asset index in all social and health surveys by the National Statistical Office for routine health equity monitoring is highly appreciated.
Notes
* Coverage criteria were as follows: family planning included use of a modern method by women married or living with a partner; antenatal care included at least four visits during the last pregnancy; skilled birth attendance included the last baby being delivered by a physician, nurse, midwife or auxiliary midwife; delivery care at a health facility included a district, provincial or private hospital; low birthweight infant was one that weighed less than 2.5 kg; exclusive breastfeeding in a baby under six months of age was breastfeeding without water, any other foods or supplements.
References
- United Nations Population Fund. Human rights: supporting the constellation of reproductive rights. At: <www.unfpa.org/rights/rights.htm. >. Accessed 24 February 2011.
- Bureau of Reproductive Health. Reproductive Health Protection statute (draft). At: <http://rh.anamai.moph.go.th/index.html. >. Accessed 10 January 2011.
- V Tangcharoensathien, S Tantivess, Y Teerawattananon. Universal coverage and impact on reproductive health services in Thailand. Reproductive Health Matters. 10: 2002; 59–69.
- Y Teerawattananon, V Tangcharoensathien. Designing a reproductive health service package in the universal health insurance scheme in Thailand: match and mismatch of need, demand and supply. Health Policy and Planning. 19: 2004; i31–i39.
- S Limwattananon, V Tangcharoensathien, P Prakongsai. Equity in maternal and child health in Thailand. Bulletin of World Health Organization. 88: 2010; 420–427.
- WHO UNICEF UNFPA World Bank. Trends in maternal mortality: 1990 to 2008. 2010; WHO: Geneva.
- BC Tanis, K Kapiteijn, RM Hage. Dutch women with a low birthweight have an increased risk of myocardial infarction later in life: a case control study. Reproductive Health. 2: 2005; 1. DOI: 10.1186/1742-4755-2-1.
- K Molbak, A Gottschau, P Aaby. Prolonged breastfeeding, diarrhoeal disease, and survival of children in Guinea-Bissau. BMJ. 308: 1994; 1403–1406.
- Quantitative techniques for health equity analysis: technical note #4: measuring living standards: household consumption and wealth indices. World Bank. At: <http://siteresources.worldbank.org/INTPAH/Resources/Publications/Quantitative-Techniques/health_eq_tn04.pdf. >. Accessed 12 March 2011.
- Tracking the Millennium Development Goals, Thailand national government report. At: <www.mdgmonitor.org/country_progress.cfm?c=THA&cd=764#. >. Accessed 12 March 2011.
- J Lertiendumrong, V Wongmongkol, H Sumalee. The 2008–2009 economic crisis and its impact on health and health systems in Thailand. 2010; Ministry of Public Health, International Health Policy Program.
- TAJ Houweling, C Ronsmans, OMR Campbell. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bulletin of World Health Organization. 85: 2007; 745–754.
- V Tangcharoensathien, P Faramnuayphol, W Teokul. A critical assessment of mortality statistics in Thailand: potential for improvements. Bulletin of World Health Organization. 84: 2006; 233–238.
- W Patcharanarumol, V Tangcharoensathien, S Limwattananon. Why and how did Thailand achieve Good Health at Low Cost? A research report. 2011; Ministry of Public Health, International Health Policy Program: Nonthaburi.
- V Tangcharoensathien, P Prakongsai, S Limwattananon. From targeting to universality: lessons from the health system in Thailand. P Townsend. Building decent societies: rethinking the role of social security in development. 2009; Palgrave Macmillan: London, 310–322.
- V Tangcharoensathien, W Teokul, L Chanwongpaisarn. Challenges of implementing universal health care in Thailand. Social Policy in a Development Context Series: transforming the developmental welfare state in East Asia. 2005; UN Research Institute for Social Development: Geneva, 257–282.
- P Vapattanawong, MC Hogan, P Hanvoravongchai. Reductions in child mortality levels and inequalities in Thailand: analysis of two censuses. Lancet. 369: 2007; 850–855.
- J Rohde, S Cousens, M Chopra. 30 years after Alma-Ata: has primary health care worked in countries?. Lancet. 370: 2008; 950–961.
- K Lee, L Lush, G Walt, J Cleland. Family planning policies and programmes in eight low-income countries: a comparative policy analysis. Social Science and Medicine. 47: 1998; 949–959.
- S Wilbulpolprasert, S Thaiprayoon. Thailand: good practice in expanding health coverage – lessons from Thai health care reform. PE Gottret, G Schieber, H Waters. Good practices in health financing: lessons from reforms in low and middle-income countries. 2008; World Bank: Washington DC.
- V Tangcharoensathien, P Harnvoravongchai, S Pitayarangsarit. Health impacts of rapid economic changes in Thailand. Social Science and Medicine. 51(6): 2000; 789–807.
- D Gillespie, S Ahmed, A Tsui. Unwanted fertility among the poor: an inequity?. Bulletin of World Health Organization. 85: 2007; 100–107.