Abstract
Abstract
In Vietnam, despite the possibility of living healthy sexual lives and bearing children due to the increasing availability of antiretroviral therapy and prevention of mother-to-child transmission services, HIV programming has given little attention to the sexual and reproductive health of people living with HIV. Our study explored factors influencing sexual and reproductive health decision-making, needs, rights and access to services for women living with HIV in Hai Phong and Ho Chi Minh City. Nearly half of the women were sexually active at the time of the study and 15% reported wanting a child or another child. Only 14% of women who did not want a child used contraceptive services in the last six months. More than 40% of women reported being advised, primarily by health care providers and family members, to abstain from sex, and more than 13% who were pregnant at the time of the study said that they had been advised to have an abortion. As with all women, women living with HIV must be informed of their sexual and reproductive rights and must have access to medically sound counseling and services to facilitate informed reproductive health decision-making. Sexual and reproductive health services are urgently needed for this population.
Résumé
Au Viet Nam, en dépit de la possibilité de mener une vie sexuelle saine et d’avoir des enfants grâce à la disponibilité croissante de thérapie antirétrovirale et de services de prévention de la transmission mère-enfant, les programmes relatifs au VIH ont accordé peu d’attention à la santé génésique des personnes vivant avec le virus. Notre étude analyse les facteurs influençant les décisions de santé génésique, les besoins, les droits et l’accès aux services des femmes vivant avec le VIH à Hai Phong et Ho-Chi-Minh-Ville. Près de la moitié des femmes étaient sexuellement actives au moment de l’étude et 15% ont indiqué qu’elles souhaitaient devenir mères ou avoir un autre enfant. Seulement 14% des femmes qui ne voulaient pas d’enfant avaient utilisé des services contraceptifs les six derniers mois. Plus de 40% des femmes ont affirmé avoir reçu des conseils, principalement de prestataires de soins de santé et de membres de leur famille, leur recommandant de ne pas avoir de rapports sexuels et plus de 13% des femmes enceintes au moment de l’étude ont déclaré qu’on leur avait conseillé d’avorter. Comme toutes les femmes, les femmes vivant avec le VIH doivent être informées de leurs droits génésiques et avoir accès à des services et des conseils médicalement valables pour faciliter une prise de décision bien informée. Des services de santé génésique sont requis de toute urgence pour cette population.
Resumen
En Vietnam, pese a la posibilidad de vivir una vida sexual saludable y tener hijos debido a los servicios cada vez más disponibles de terapia antirretroviral y prevención de la transmisión materno-infantil, los programas de VIH han prestado poca atención a la salud sexual y reproductiva de las personas que viven con VIH. Nuestro estudio exploró los factores que influyen en la toma de decisiones, necesidades y derechos relacionados con la salud sexual y reproductiva de las mujeres que viven con VIH en Hai Phong y Ciudad Ho Chi Minh, así como su acceso a los servicios. Casi la mitad de las mujeres eran sexualmente activas cuando se realizó el estudio y el 15% informó querer tener un hijo u otro hijo más. Solo el 14% de las mujeres que no querían un hijo usaron servicios de anticoncepción en los últimos seis meses. Más del 40% de las mujeres relataron haber sido aconsejadas, principalmente por profesionales de la salud y miembros de su familia, que se abstuvieran de tener relaciones sexuales y más del 13% de las mujeres que estaban embarazadas cuando se realizó el estudio dijeron que les habían aconsejado tener un aborto. Al igual que todas las mujeres, las que viven con VIH deben ser informadas de sus derechos sexuales y reproductivos y deben tener acceso a consejería y servicios médicamente confiables que faciliten una toma de decisiones informadas sobre la salud reproductiva. Esta población necesita urgentemente servicios de salud sexual y reproductiva.
Globally, more than 5.2 million people are currently on antiretroviral therapy. Improved access to antiretroviral therapy has enabled people living with HIV to live longer and healthier lives,Citation1–3 enjoy healthy sexual relationships, and bear and raise children. Yet the rights of people living with HIV to make informed sexual and reproductive health decisions have been contested and in some cases violated around the world.Citation4–7 In many countries, the beliefs and practices of health care providers and community members have not kept pace with the health, economic and social potential for people living with HIV to live healthy sexual and reproductive lives.Citation8,9 Stigma and discrimination on the part of providers and the community, as well as power imbalances between providers and clients have led to missed opportunities to fulfill sexual and reproductive health desires as well as to egregious violations of rights.Citation10–16
In concentrated epidemic settings, like Vietnam – where HIV programs and policies focus on prevention among injecting drug users, female sex workers and men who have sex with men – little attention has been given to the sexual and reproductive health needs of people living with HIV. The Vietnam Ministry of Health estimates that between 250,000 and 300,000 people currently have HIV.Citation17,18 Although the major behavioral driver of the Vietnamese epidemic to date has been injecting drug use, recent data show increasing sexual transmission and HIV prevalence among women and a decline in the male-to-female ratio of infections (3:1 in 2007 compared to 2.6:1 in 2012).Citation17
By the end of 2009, approximately 54% of those eligible were on antiretroviral therapy, an increase from 2006 when only 14% were receiving treatment.Citation19 The number of facilities in Vietnam providing antiretroviral therapy increased from 74 sites in 2005 to 287 in 2009,Citation20 and the proportion of pregnant women accessing prevention of mother-to-child transmission (PMTCT) services increased from 14% in 2007 to 32% in 2009.
Yet, recent research in Vietnam indicates that women’s use of voluntary HIV counseling and test ing services, an important gateway to other critical HIV services including PMTCT and antiretroviral therapy, is low. Indeed, the majority of women receive antenatal care at the commune level where antenatal HIV testing remains unavailable.Citation19 A study in the Bavi district of Hanoi found that only 6% of pregnant women were tested for HIV and that 79% of those who perceived they were at risk of HIV infection had never been tested.Citation21 Little is known about access to sexual and reproductive health services among people living with HIV,Citation22 and there is evidence that women who are not drug users or sex workers are not accessing HIV prevention, care and treatment.Citation23 A recent study in Hai Phong found that pregnant women do not get tested for HIV in the course of antenatal care,Citation24 suggesting that some women living with HIV (WLHIV) may lack the knowl edge of and access to treatment and prevention of mother-to-child transmission services.
Stigma and discrimination in health care settings may also deter women from receiving the services they need. In 2005–2006, Oosterhoff and colleagues found that health care providers in Hanoi disclosed the HIV status of pregnant women to local authorities without permission.Citation25 Khuat, Nguyen and Ogden explored the “double stigma” faced by WLHIV: in addition to prevailing gender expectations of women as guardians of family values and educators of the young, there is also a widespread association of HIV with marginalized groups and illegal behavior such as injecting drug use and sex work.Citation26 Research on WLHIV in Hai Phong and Ho Chi Minh City found that women were often more adversely affected than men by the challenges associated with HIV.Citation27
To address the research and program gaps regarding access to sexual and reproductive health services for women living with HIV, including knowledge about and use of sexual and reproductive health services and barriers to informed reproductive health decision-making, we conducted a cross-sectional study of 300 HIV-infected women living in two urban centers in Vietnam. We also aimed to explore any differences in program needs between the women in the two study sites.
Methodology
In a two-phase, mixed-method study in Ho Chi Minh City and Hai Phong, quantitative data were collected using a cross-sectional survey of 300 WLHIV. In this paper, we present results of the baseline survey of WLHIV, with a focus on sexual and reproductive health outcomes such as desire for chil dren; knowledge and use of sexual and reproductive health services; and the advice WLHIV receive regarding sexual behavior and pregnancy. We also investigate differences in service needs between the two study sites and correlations with demographic and health characteristics. Additional findings from other components of the study are available elsewhere.Citation22
Research setting
In both sites, HIV prevalence among women attending antenatal care exceeds 1%.Citation28 Yet, important differences exist between the settings and the HIV epidemics. The epidemic in Hai Phong, a northern port city near the China border with a population of 1.9 million, is associated primarily with injecting drug use; 66% of injecting drug users and 7% of female sex workers tested HIV-positive in 2005–2006.Citation29,30 Ho Chi Minh City, with an official population of 6.0 million, is the commercial center of Vietnam. During the 1990s and early 2000s, the HIV epidemic in Ho Chi Minh City was associated with injecting drug use, first among older and then among a younger generation of users. However, since the mid-2000s, new infections have been increasingly driven by sexual transmission.Citation31 Governmental and international and national non-governmental organizations in both cities currently implement HIV prevention programs among most-at-risk populations and PMTCT antiretroviral services.Citation32 In its 2010 UNGASS report, the government highlighted substantial increases in the number of people on antiretroviral therapy in Vietnam – where antiretrovirals now reach nearly 60% of all treatment-eligible people living with HIV – including increases in Hai Phong and in Ho Chi Minh City, where more than 14,500 people were receiving antiretroviral services by the end of 2009.Citation19
Recruitment and sampling
Selection of study districts was based on severity of the epidemic relative to other districts. In each city, four districts were randomly selected from a list provided by local AIDS authorities of the seven most heavily HIV-affected districts. Using probability-proportionate-to-size sampling, study personnel randomly selected potential study participants from lists of women living with HIV provided by the Provincial AIDS Center (PAC) in Ho Chi Minh City and district-level Preventive Medicine Centers (PMCs) in Hai Phong. The lists were devoid of personal identifying information. Then PAC and PMC outreach workers made initial contact in person or by phone with potential participants to describe the study and ask women if they might be interested in enrolling. Those who expressed an interest were given an interview time and location, where they were met by research field supervisors who conducted formal screening and, if the woman was found eligible (at least 18 years old and self-identified as having HIV), requested informed consent. PAC/PMC outreach workers did not know who among the women contacted in the first step subsequently presented for interviews. The research team never had access to identifying information for these women.
Women living with HIV who were peer support group leaders assisted in the design of the questionnaire and were trained to conduct survey interviews. Interviewer training covered study purpose, methods and ethical issues. These interviewers neither interviewed women from their home districts nor women they knew.
The sample size of 300 was adequate to detect a 20% improvement between baseline and month 12 in antiretroviral literacy (specifically, the proportion of respondents with knowledge of the purpose of antiretroviral therapy) at each of the two sites, with 96% power and a two-sided alpha of 0.05, using a standard formula for sample size calculation for paired-sample analysis. We assumed a baseline proportion of 40% with accurate knowledge, based on previous studies of HIV prevention and treatment knowledge among people living with HIV in Vietnam.Citation33
Data collection
In January 2009, the trained interviewers collected baseline survey data in both study locations. Face-to-face survey interviews, lasting 90–120 minutes, were conducted in Vietnamese in private locations convenient to participants. Supervisors oversaw daily enrollment progress and data collection, including checking questionnaires for completeness and consistency. Questions addressed reproductive health characteristics, risk behaviors, and knowledge and use of HIV and sexual and reproductive health services. The survey instrument was pilot-tested and revised prior to initiating data collection. All participants received 50,000 Vietnamese Dong (approximately US$ 2.85 at the time of data collection)Citation34 to cover the costs of travel and/or lost work time. The study protocol was approved by institutional review boards at Boston University Medical Center and Hanoi School of Public Health.
Analytic methods
Quantitative data were summarized using frequencies and proportions for categorical variables; means, standard deviations and medians were used for continuous variables. Bivariate logistic regression was used to identify correlates of the outcomes of interest (knowledge, utilization or access to services, either as single-question binary outcomes or continuous constructed scores). Multivariate logistic regression was used to assess potential confounders for their impact on odds ratios. Variables that created more than 10% change in the odds ratio were retained. Multivariate models included individual demographic and socioeconomic characteristics such as age, city of residence, antiretroviral status and having a living child.
Results
Demographic profile of participants
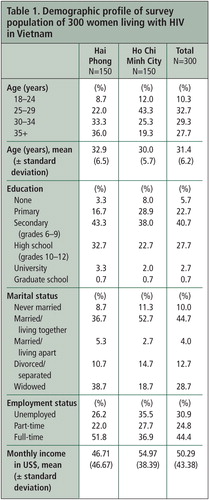
The survey sample was divided evenly between the two cities (Table 1). The majority of study participants were at least 25 years old, were educated through lower secondary school, and had ever been married. Differences between study participants in the two cities are notable. Women in Ho Chi Minh City were younger, had lower levels of education, and were more likely to be unemployed and less likely to be widowed compared to women in Hai Phong.
Reproductive health history and characteristics
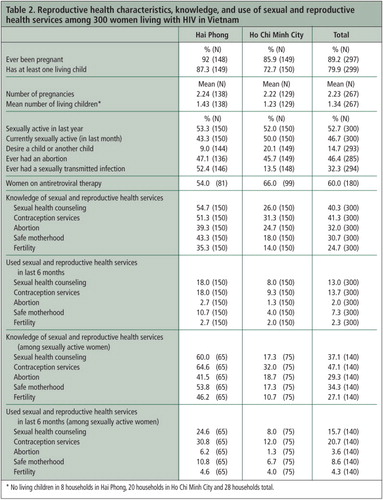
The majority of women at both sites had been pregnant at least once, with a mean of 2.2 pregnancies (Table 2). The proportion of currently pregnant women was low (data not shown). The mean number of living children was 1.3; women in Hai Phong reported slightly more children than those in Ho Chi Minh City (1.4 vs. 1.2). Just over half of study participants (52%) reported sexual activity in the last year.
With respect to desire for more children, 13 women in Hai Phong (9%) and 30 women in Ho Chi Minh City (20%) indicated that they would like a/another child. Most women who desired a child were between 25 and 34 years old (49%), currently married (51%) and on antiretroviral therapy (74%), and did not have at least one living child (56%) (data not shown). Higher proportions of women in Hai Phong knew about the following sexual and reproductive health services: sexual health counseling, contraception, abortion, safe motherhood and fertility services; had ever used those services; and had used those services in the last six months.
Overall, knowledge and use of sexual and reproductive health services among women in our study were low compared to women surveyed in routine demographic and family planning surveys.Citation35 While 40% of women in the study knew about sexual health counseling, only 13% had used those services in the last six months. Similarly, 41% of women had knowledge of contraceptive services, yet only 14% had used those services in the past six months. In contrast, more than 99% of married women nationwide had knowledge of modern contraceptive methods and more than 68% of married women reported the use of modern contraception.Citation36
Correlations between demographic characteristics and knowledge and use of sexual and reproductive health services
Crude logistic regression analysis was used to determine correlations between demographic characteristics and knowledge and use of sexual and reproductive health services. Place of residence, educational level, employment status, insurance status and current antiretroviral use were found to be significantly associated with knowledge of one or more types of sexual and reproductive health services (data not shown). WLHIV in Hai Phong compared to those in Ho Chi Minh City were more than three times as likely to know about sexual health counseling (odds ratio [OR] =3.40), more than twice as likely to know about contraceptive services (OR=2.29) and nearly twice as likely to know about abortion services (OR=1.96). Women with higher levels of education were much more likely to know about contraceptive services (secondary school compared to uneducated women: OR=6.48; university compared to uneducated women: OR=26.25), but no significant association was found between level of education and knowledge of other sexual and reproductive health service types.
WLHIV in Hai Phong were more than twice as likely to have ever used or used in the last six months any of the following: sexual health counseling, contraceptive services or abortion services (OR=2.17). Women aged 25–29 were more likely to have used any of those services in the last six months compared to women aged 18–24 (OR=3.92); and women with children were also more likely to have done so (OR=2.80). None of the following was a significant predictor of use of those services: marital status; education; income; employment status; having health insurance or social insurance; having a partner or child who has HIV; or having a partner or child on antiretroviral therapy.
Advice about sexual abstinence and abortion
Participants were asked if they had ever been advised to be abstinent or to have an abortion because they were HIV-positive and from whom they received the advice. Half of the women (50%) in Hai Phong and 31% in Ho Chi Minh City (40% of all women) had been advised to abstain from sexual activity (data not shown). Of the women advised to abstain, 66% were advised by health care providers, 32% by family members and 16% by peer educators. Of all WLHIV pregnant at the time of the study, 13% were advised to have an abortion due to their HIV status; this advice came primarily from health care providers (41%), family members (44%) and friends (26%).
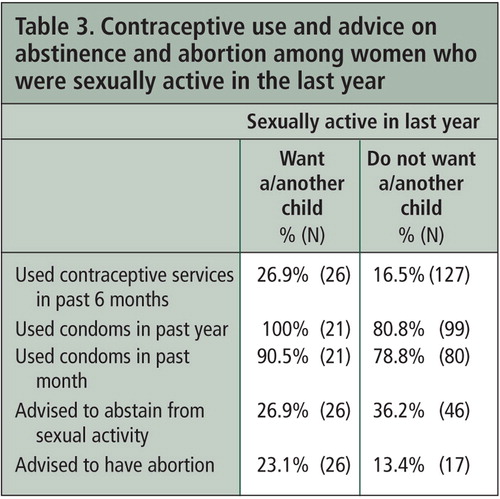
More than one-third (35%) of all sexually active women had been advised to be abstinent. Of women who were sexually active and desired a child, 27% had used contraceptive services in the previous six months, while 100% had used condoms in the previous year (Table 3). Twenty-seven percent of women who desired a child had been advised to abstain from sexual activity because of their HIV status and 23% had been advised to have an abortion. Similarly, among women who did not want children but were sexually active, 17% had accessed contraceptive services in the last six months. Again, condom use was very high.
Variables associated with desire for children and advice about sexual abstinence and abortion
Crude logistic regression was used to identify variables associated with the desire for children and with having been advised to be sexually abstinent or to have an abortion when pregnant (Table 4). Women in Hai Phong were more than twice as likely as women in Ho Chi Minh City to have been advised to abstain from sex. They were also less likely to desire a child or more children. Women aged 35 and older were more than twice as likely as women aged 18–24 to have been advised to be sexually abstinent. Women who were never married were much more likely to want a child or another child. Women who were employed full-time were more than twice as likely to have been advised to be abstinent as women who were unemployed. Women on antiretroviral therapy were twice as likely as women not on antiretroviral therapy to want a child or another child and were less likely to have been advised to be abstinent. However, they were nearly three times as likely to have been advised to abort a pregnancy. Women with at least one living child were much less likely to want a child or another child and were much less likely to have been advised to abort a pregnancy than were women who did not have at least one living child.
Multivariate logistic regression to determine predictors of key sexual and reproductive health outcomes
Multivariate logistic regression was used to determine whether, after controlling for other factors, specific predictors were significantly associated with important sexual and reproductive health outcomes, including service use in last six months, advice to abstain from sex, advice to have an abortion and desire to have a child or more children. After adjusting for age, marital status, antiretroviral use and existence of a least one living child, women in Hai Phong were much more likely than women in Ho Chi Minh City to have used sexual health counseling (OR=2.44) and contraceptive services (OR=2.79) in the previous six months (data not shown). Women in Hai Phong were also more likely to have been advised to be sexually abstinent (OR=1.88). There were no significant differences by age after adjusting for other demographic characteristics. However, women on antiretroviral therapy compared to those not on antiretroviral therapy were more likely to have used sexual health counseling services (OR=2.27) and also were more likely to have been advised to have an abortion (OR=2.82). Women with one or more children were significantly less likely to want another child (OR=0.14).
Discussion
These findings highlight the continuing challenges faced by women living with HIV in accessing the full range of reproductive health services they need to live healthy lives. Given the importance of enabling women living with HIV to make fully informed and safe decisions about their sexual and reproductive lives, these findings are worrisome. Low knowledge and use levels affect women’s sexual and reproductive decision-making in negative ways, and may contribute to vulnerability to HIV infection in the first place.
Although only 14% of women in this study wanted a child or another child, a relatively small proportion of currently sexually active women reported using contraceptive services in the past six months. A substantial proportion of the women in both cities (over 40%) had been advised to abstain from sex. To the degree that women were following this advice, their need for contraceptive services would be low. But this does not explain why women who were sexually active at the time of the study and did not want to get pregnant did not access contraceptive services.
One explanation may be that some women did not seek services because their health care providers had already advised them to be abstinent; to request contraception would have been to go against the advice of their providers. Interestingly, our analysis indicated that, in both cities, women on antiretroviral therapy were twice as likely as those not on antiretroviral therapy to want a child or another child and were less likely to have been advised to be abstinent, suggesting that access to treatment and care in different service settings (HIV services versus reproductive health services) may affect the sexual and reproductive health advice given to women.
Since it is well established that antiretroviral therapy can greatly reduce the risk of transmission between sexual partners and that PMTCT can greatly reduce the risk of transmission from mother to child, our finding that a large proportion of women had been advised to abstain from sex because of their HIV-positive status is alarming. This apparent disconnect between the scientific evidence and the advice given by some providers may be the result of an entrenched vertical program structure that separates reproductive health and HIV services in Vietnam. Provider advice to be abstinent and to have an abortion may reflect discrimination in health care settings which has been documented in other studies in Vietnam.Citation26,37 Additional analysis is underway to explore differences in attitudes between HIV providers and sexual and reproductive health providers who may impact women’s decision-making. Regardless of why it occurs, such advice is counter to the desires of many women to have healthy sexual lives and to choose to have children – both of which are fundamental human rights.
Visitor and counsellor at a reproductive health clinic discuss HIV educational materials, Vietnam, 2005
That such advice often came from providers and peer educators, who are widely respected as authorities on HIV, is disconcerting since guidance from such figures is likely to carry a good deal of weight. Also, given the importance of the family (including in-laws) in reproductive health decision-making in Vietnam,Citation38,39 it is not surprising that many women in our study reported that family members advised abstinence and abortion. This advice may stem from the belief of family members that pregnancy will lead to further ill health in the woman and HIV infection in the child.
Our analysis revealed differences between the two study sites in a number of important outcomes. We believe these findings are related to differences between the socio-economic environments of the two cities and geographical variations in the HIV epidemic across Vietnam. Hai Phong is a much smaller city, where the population is more stable and information regarding services is likely to be better known to residents than in Ho Chi Minh City, a dynamic mega-city characterized by a highly mobile population. Mobile populations often do not have the same access to health services as registered residents of the city and therefore may be less likely to use them.
Taken as a whole, major differences in findings between the two sites are noteworthy considering that Vietnam has different trends in HIV transmission dynamics which may in turn affect knowledge of services and the willingness of WLHIV to access them. Differences in socioeconomic environments, the state of the epidemic and the personal characteristics of WLHIV between the two cities must be considered in order to design and implement effective programs to meet their needs. Our continuing analysis of other components of the larger WLHIV study may shed further light on these issues.
Our findings suggest recommendations to improve knowledge of and access to HIV, PMTCT and sexual and reproductive health services for WLHIV across Vietnam. First, efforts should be made to ensure that all sexual and reproductive health providers and HIV providers understand the importance of informing WLHIV about how they can benefit from these services and where specialized information can be obtained. As part of this effort, training of providers should emphasize sexual and reproductive health and rights of all people living with HIV. One training program in Vietnam was effective in reducing stigma and discrimination on the part of providers toward their clients,Citation40–42 but greater efforts are needed to scale up such programs. In addition, family members must also know about these services and the potential these services have to facilitate healthy outcomes for women and their children.
Second, these findings underscore the need to integrate HIV and sexual and reproductive health services in order to provide people living with HIV with the information required to make informed sexual and reproductive health decisions. While important efforts are underway to integrate HIV services into sexual and reproductive health programs in An Giang, Soc Trang, Can Tho and Quang Ninh,Citation43 evaluation of this work and expansion to other hard-hit provinces is an important next step. HIV services need to also expand their offerings to include at a minimum sexual health counseling and referral to sexual and reproductive health service delivery points that are receptive to the needs of WLHIV.
Third, just as HIV prevention and treatment efforts are increasingly recognizing the need to tailor programs to specific populations in order to improve effectiveness, programs aimed at women living with HIV must recognize the diversity of this population. It includes older widows, young single women, married women of all ages, women taking antiretrovirals and not taking antiretrovirals, and women who need a range of services for their children. Importantly, our study found that the programmatic needs of women may be very different depending on the nature of the epidemic and specific location. Although both study sites show increasing sexual transmission and infection among women, the service needs of these women are diverse. Responding effectively to such a heterogeneous mix of women, families and locales will require greater flexibility to apply location-specific research findings to program design and implementation, as well as greater collaboration between a number of government and civil society organizations, including health, social affairs, the Women’s Union (a government organization with networks from the national to local level) and support groups of women living with HIV. The last must play a prominent role in building the capacity of women to demand their rights and the services to meet their needs.
Conclusion
This study highlights the current disconnects between the reproductive desires and needs of women living with HIV, what is medically possible and available in Vietnam (namely antiretroviral therapy, PMTCT and contraception) and the advice given by health care providers and families. Existing health services and infrastructure in most parts of Vietnam have the capacity to support women living with HIV to more fully enjoy their sexual and reproductive health and rights, but political will and leadership are needed in the health policy realm to promote strategies and interventions that advance this aim. So often in developing country settings, services are simply not available for women, let alone women living with HIV, to make informed decisions about their reproductive health. Vietnam has this capacity and is providing these services to women not living with HIV, indicating a moral and rights imperative that cannot be ignored. Indeed, if this opportunity is seized, Vietnam could serve as a global model for how health care providers and systems and the women they serve can make a difference in the fulfillment of sexual and reproductive health and wellbeing.
Acknowledgements
We would like to express our sincere thanks to all of the WLHIV who agreed to participate in this study – as advisors to the study design, interviewers and respondents. We are grateful to the Hai Phong and Ho Chi Minh City provincial leaders for their support of the research including Mr. Hoang Van Ke, Vice Chairman of Hai Phong People’s Committee; Dr. Nguyen Van Vi, Director of Hai Phong Health Services; Dr. Nguyen Quang Thinh, Director of Hai Phong Communication and Health Education Center; the Hai Phong Women’s Union; the participating District Health Prevention Centers; Legal Aid Center; and the Voluntary Counseling and Testing Center at Cat Bi. In Ho Chi Minh City we would like to thank Dr. Le Truong Giang, Vice Director of the Ho Chi Minh City Department of Health; Dr. Tieu Thi Thanh Van, Vice Director of the Ho Chi Minh City HIV/AIDS Executive Office of the Ho Chi Minh City AIDS Committee; and the Medical Research Center. We also thank Thomas Kane, Jordan Tuchman and Cheryl McClurg for their contributions. This research was supported by USAID/PEPFAR and Pact Vietnam under the project entitled “Engendering the care and treatment response: addressing the needs of women living with HIV in Vietnam.” Some of the data in this paper were presented in a poster at the 2010 International AIDS Conference in Vienna.
References
- WHO UNAIDS UNICEF. Towards universal access: scaling up priority HIV interventions in the health sector: progress report 2010. At: http://whqlibdoc.who.int/publications/2010/9789241500395_eng.pdf Accessed 10 May 2012
- M Mahy, J Stover, K Stanecki. Estimating the impact of antiretroviral therapy: regional and global estimates of life-years gained among adults. Sexually Transmitted Infections. 86(suppl 2): 2010 Dec; ii67–ii71.
- WHO UNAIDS UNICEF. Global HIV/AIDS Response: epidemic update and health sector progress towards universal access 2011. At: http://www.who.int/hiv/pub/progress_report2011/en/index.html Accessed 14 May 2012
- W Holmes. Having a safe pregnancy must be a right, not a privilege. Population Action International; 2007. At: http://www.populationaction.org/Publications/Reports/Measure_of_Survival/sec4.shtml Accessed 10 May 2012
- International Community of Women Living with HIV/AIDS. Positive prevention and the sexual and reproductive rights of HIV-positive people. 2005. At: http://www.icw.org/node/161 Accessed 14 May 2012
- J Kaufman, L Messersmith. Integrating the fields of sexual and reproductive health and HIV/AIDS [unpublished]. 2005. 52p. At: http://paa2006.princeton.edu/download.aspx?submissionId=60226 Accessed 14 May 2012
- B Nattabi, J Li, SC Thompson. A systematic review of factors influencing fertility desires and intention among people living with HIV/AIDS: implications for policy and service delivery. AIDS and Behavior. 13(5): 2009 Oct; 949–968.
- The pregnancy intentions of HIV-positive women: forwarding the research agenda [conference report]. 2010 March 17–19; Harvard School of Public Health, Boston, MA.
- Center for Reproductive Rights Federation of Women Lawyers – Kenya. At risk: rights violations of HIV-positive women in Kenyan health facilities. 2008. At: http://reproductiverights.org/sites/default/files/documents/At_Risk.pdf Accessed 14 May 2012
- D Cooper, J Harries, L Myer. “Life is still going on”: reproductive intentions among HIV-positive women and men in South Africa. Social Science and Medicine. 65(2): 2007 Jul; 274–283.
- V Paiva, E Filipe, N Santos. The right to love: the desire for parenthood among men living with HIV. Reproductive Health Matters. 11(22): 2003 Nov; 91–100.
- L Nyblade, A Stangl, E Weiss. Combating HIV stigma in health care settings: what works?. Journal of the International AIDS Society. 12: 2009 Aug 6; 15.
- M Gogna, M Pecheny, I Ibarlucía. The reproductive needs and rights of people living with HIV in Argentina: health service users’ and providers’ perspectives. Social Science and Medicine. 69(6): 2009 Sep; 813–820.
- V Paiva, R Latorre Mdo, N Gravato. [Sexuality of women living with HIV/AIDS in São Paulo]. Cad Saude Publica. 18(6): 2002 Nov–Dec; 1609–1620.
- L Myer, K Rebe, C Morroni. Missed opportunities to address reproductive health care needs among HIV-infected women in antiretroviral therapy programmes. Tropical Medicine and International Health. 12(12): 2007 Dec; 1484–1489.
- J Mallet, V Kalambi. The forced and coerced sterilization of HIV-positive women in Namibia. HIV/AIDS Policy and Law Review. 13(2–3): 2008 Dec; 77–78.
- Vietnam Ministry of Health. Official HIV/AIDS estimates and projections for Viet Nam, 2007–2012. 2009. At: http://www.fhi360.org/en/HIVAIDS/pub/survreports/res_VN_EstimatesandProjections07-12.htm Accessed 14 May 2012
- Population Reference Bureau. HIV/AIDS in Vietnam: the current situation, the national response, the emerging challenges. 2007. At: http://www.prb.org/Reports/2007/VietnamHIVChartbook.aspx Accessed 14 May 2012
- UNGASS Report: Socialist Republic of Vietnam. 2010. At: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CFMQFjAA&url=http%3A%2F%2Fwww.unaids.org%2Ffr%2Fdataanalysis%2Fmonitoringcountryprogress%2F2010progressreportssubmittedbycountries%2Ffile%2C33682%2Cfr..pdf&ei=p2ixT_jPOuKI6QGVraGdCQ&usg=AFQjCNF759f7g3AbQjsTiwM9pkNmL_BIqg Accessed 14 May 2012
- USAID/Vietnam. HIV/AIDS health profile. At: www.usaid.gov/our_work/global_health/aids/.../vietnam_profile.pdf Accessed 14 May 2012
- A Pharris, TKC Nguyen, C Tishelman. 2011. Expanding HIV testing efforts in concentrated epidemic settings: a population-based survey from rural Vietnam. PLoS ONE. 6(1): 2011; e16017. At: http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0016017 Accessed 25 May 2012
- L Messersmith, L Sabin, K Semrau. Engendering the care and treatment response: addressing the needs of women living with HIV in Vietnam: baseline assessment report. 2009. Boston University Center for International Health and Development (CIHD). At: http://www.bu.edu/cghd/projects/addressing-the-needs-of-women-living-with-hiv-in-vietnam/ Accessed 14 May 2012
- T Nguyen, P Oosterhoff, A Hardon. A hidden HIV epidemic among women in Vietnam. BMC Public Health. 8: 2008 Jan 28; 37.
- L Nguyen, S Christoffersen, V Rasch. Uptake of prenatal HIV testing in Hai Phong Province, Vietnam. Asia Pacific Journal of Public Health. 22(4): 2010 Oct; 451–459.
- P Oosterhoff, AP Hardon, TA Nguyen. Dealing with a positive result: routine HIV testing of pregnant women in Vietnam. AIDS Care. 20(6): 2008 Jul; 654–659.
- HT Khuat, TVA Nguyen, J Ogden. Because this is the disease of the century: understanding HIV-and AIDS-related stigma and discrimination in Vietnam. International Center for Research on Women; 2004. At: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CFAQFjAA&url=http%3A%2F%2Fpdf.usaid.gov%2Fpdf_docs%2FPNADJ668.pdf&ei=f3KxT_a8HKTM6QGhtIG8CQ&usg=AFQjCNGG_JQBcADubGCrEG9ZL1CBIF-FrA Accessed 14 May 2012
- Center for Community Health and Development. A rapid assessment of women living with HIV/AIDS in Hai Phong and HCMC [unpublished]. Project entitled “support to HIV-positive women.” 2006.
- Vietnam Ministry of Health. HIV prevalence and epidemiological status. 2005. At: http://www.vaac.gov.vn/Desktop.aspx/Content/Prevalence-data/VIETNAM_HIV_and_AIDS_Data/ Accessed 14 May 2012
- Vietnam Ministry of Health. Results from the HIV/STI integrated biological and behavioral surveillance (IBBS) in Vietnam 2005–2006. 2006. At: http://aidsdatahub.org/en/reference-librarycols2/surveillance-situational-analysis-assessments/item/12668-results-from-the-hiv/sti-integrated-biological-and-behavioral-surveillance-ibbs-in-vietnam-2005%E2%80%932006-national-institute-of-hygiene-and-epidemiology-vietnam-fhi-vietnam-administration-of-hiv/aids-control-et-al-2006 Accessed 14 May 2012
- Central Intelligence Agency. The World Factbook. Last updated: 10 January 2012. At: https://www.cia.gov/library/publications/the-world-factbook/geos/vm.html Accessed 14 May 2012
- Analysis and Advocacy Project. The HIV epidemic in Ho Chi Minh City: where is it going? 2009. At: http://www.fhi360.org/en/HIVAIDS/pub/survreports/res_HIVepidemicHCMc.htm Accessed 14 May 2012
- Vietnam Ministry of Health. The national strategy on HIV/AIDS prevention and control in Vietnam till 2010 with a vision to 2020. 2004. At: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=3&ved=0CFUQFjAC&url=http%3A%2F%2Fwww.unaids.org.vn%2Findex.php%3Foption%3Dcom_docman%26task%3Ddoc_download%26gid%3D3%26Itemid%3D%26lang%3Den&ei=enixT6vJJ8SX6QGfhbCfCQ&usg=AFQjCNGyxZ-P9GGFhvcTThv-LCdhQIvhcw Accessed 14 May 2012
- L Sabin, T Vian, D Hamer. Evaluation of President’s Emergency Plan for AIDS Relief (PEPFAR)-funded community outreach HIV prevention programs in Vietnam: report on findings, 2008. Hanoi, Vietnam: PEPFAR Vietnam; January 2010. At: http://www.bu.edu/cghd/projects/evaluation-of-community-outreach-hiv-prevention-programs-in-vietnam/ Accessed 14 May 2012
- USD-VND exchange rate 15 January 2009. At: http://www.gocurrency.com/v2/historic-exchange-rates.php?ccode2=VND&ccode=USD&frMonth=0&frDay=15&frYear=2009 Accessed 25 May 2012
- Committee on Population, Family and Children ORC Macro. Vietnam 2002 Demographic and Health Survey. At: http://surveynetwork.org/home/index.php?q=activities/catalog/surveys/ihsn/704-2002-001 Accessed 14 May 2012
- J Wamoyi, M Mbonye, J Seely. Changes in sexual desires and behaviours of people living with HIV after initiation on ART: implications for HIV prevention and health promotion. BMC Public Health. 11(633): 2011 Aug 8
- Messersmith L, Semrau K. Report of the national study on the levels and types of discrimination against people living with HIV/AIDS in Vietnam [unpublished]. Boston University Center for Global Health and Development; 2011.
- P Oosterhoff, NT Anh, NT Hanh. Holding the line: family responses to pregnancy and the desire for a child in the context of HIV in Vietnam. Culture, Health and Sexuality. 10(4): 2008 May; 403–416.
- BK Chi, V Rasch, N Thi Thuy Hanh. Pregnancy decision-making among HIV-positive women in northern Vietnam: reconsidering reproductive choice. Anthropology and Medicine. 18(3): 2011 Dec; 315–326.
- KTH Oanh, K Ashburn, J Pulerwitz. Improving hospital-based quality of care in Vietnam by reducing HIV-related stigma and discrimination: a Horizons final report. Population Council; 2008. At: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CF4QFjAA&url=http%3A%2F%2Fpdf.usaid.gov%2Fpdf_docs%2FPNADL301.pdf&ei=tXaxT53QB-Kf6AGg8eCUCQ&usg=AFQjCNECV_EaAcGcrnO_5J5mWjkvbzP6ng Accessed 14 May 2012
- S Wu, L Li, Z Wu. A brief HIV stigma reduction intervention for service providers in China. AIDS Patient Care and STDs. 22(6): 2008; 513–520.
- VS Mahendra, L Gilborn, B George. Reducing AIDS-related stigma and discrimination in Indian hospitals. Population Council; 2006. At: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CFsQFjAA&url=http%3A%2F%2Fwww.popcouncil.orPg%2Fpdfs%2Fhorizons%2Finplhafriendly.pdf&ei=ZHaxT9qTKOSD6AGEz5SSCQ&usg=AFQjCNGRQ6RnNMWvRbNAtRjBa1ru3KqC4A Accessed 14 May 2012
- Pact Viet Nam. Women and HIV in Vietnam: Meeting the needs. 2011. At: http://www.pactworld.org/galleries/default-file/Pact_Vietnam_Women_HIV.pdf Accessed 3 August 2012. Hanoi, Vietnam