Foreword
Much of the discussion that is entered into [in the UK] about maternity services focuses on the need for us to improve services from good to excellent. This report however shows very clearly that there are groups of women who are receiving care that is way below even minimum expected standards… It is shocking that in a country which, arguably, has one of the best maternity services in the world more is not being done to prevent such vulnerable women being denied high quality care.
“High quality care in maternity services is about far more than recognising major complications of pregnancy… Women need support in pregnancy. They need to be surrounded by a network of friends and family. They need stable and adequate housing. They need good nutrition, rest and exercise. Not only does stress and isolation impact negatively on the mother herself but it is now well known that it impacts firstly on the developing brain of the baby and secondly on the health of the baby after birth. A woman’s mental health impacts on her child’s future life chances… Dispersal of asylum seekers tears the woman away not only from her social network but from midwives with whom she needs to build a trusting and compassionate relationship… Our society is failing these women and their babies. This is not acceptable, particularly when the solutions are so obvious.” (Cathy Warwick, General Secretary, Royal College of Midwives, UK)
Executive Summary
The study
In the first half of 2011 we estimated that there were approximately 500 pregnant women seeking asylum and receiving support in the UK, and about 125 pregnant women whose claim for asylum had been refused, also receiving support. Both destitute asylum seekers awaiting a decision and refused asylum seekers who qualify for support are normally dispersed to a number of locations in the UK away from London and South East England in which, according to the UK Border Agency (UKBA), there is a “ready supply of accommodation”. They may also be relocated elsewhere after an initial dispersal.
Most pregnant women seeking asylum are likely to have been dispersed. Anecdotal reports by current or former asylum-seeking women and midwives, and interviews with midwives in an earlier study have indicated that a substantial number of pregnant women seeking asylum were dispersed during pregnancy, often very late in pregnancy and sometimes very soon after delivery. Such reports suggested that dispersal has a severe impact on women’s mental and physical health and on their maternity care. However, until now there has been no study which specifically addresses the experiences of asylum-seeking women dispersed during pregnancy, or of midwives who have looked after such women before and after dispersal. This study attempts to fill this gap.
This report is a collaboration between Maternity Action and the Refugee Council to investigate the health impact of dispersal and relocation on pregnant women seeking asylum and new mothers. The study reviewed UKBA asylum dispersal policy relating to pregnant women, and maternity policy and good practice on the care of vulnerable women.
Qualitative interviews were carried out with 20 women who had been dispersed and/or relocated by the UKBA while pregnant. The women interviewed had been in receipt of either section 95 support (support during an ongoing asylum claim) or section 4 support (support for asylum seekers whose claim has been refused). Recipients of both types of support are normally dispersed to ‘no-choice’ accommodation away from London. Financial support on section 95 is provided in cash, and in cashless form on section 4. Seventeen midwives were interviewed by phone about their experiences of working with asylum seeking women either before or after they were dispersed.
Maternity care policy and asylum seekers
Refugees and asylum seekers are an especially vulnerable group in relation to maternity care and pregnancy outcomes. National Institute for Health and Care Excellence (NICE) Guidance and other policy documents draw attention to the need for special efforts and service provision for disadvantaged and vulnerable pregnant women in order to reduce levels of maternal and infant mortality.
Despite the complex social and health needs of pregnant women seeking asylum being clearly recognised in NICE guidance, the UK Border Agency has only acknowledged pregnancy as representing a very limited health need unless there is a major pregnancy complication. Its dispersal policies made very little allowance for the healthcare and social needs of pregnant women. Its guidance, until recently, specified no time limit for dispersal during pregnancy and expected women to be able to be dispersed within two weeks of giving birth.
The UKBA introduced new guidance on pregnancy and dispersal in 2012 in response to concerns about the impact of dispersal on pregnant women. This study provides an opportunity to explore how adequately the new policy responds to the expressed concerns of asylum seekers and midwives, and to determine the compatibility of UKBA policies on dispersal of pregnant women with mainstream maternity care policy for women with complex social factors.
Physical and mental health during pregnancy
Most women interviewed reported feeling unwell during their pregnancy. Midwives and women reported serious underlying health conditions including HIV, diabetes, other sexually transmitted diseases, female genital mutilation, as well as particular problems of pregnancy, such as severe headaches, elevated blood pressure, repeated urinary tract infections. Two thirds of the women had their first contact with a midwife later than recommended in NICE guidance, which increased risks for their pregnancies.
Over half the women described suffering from mental health conditions such as depression, anxiety and flashbacks, and very high levels of stress. Two had attempted suicide during the pregnancy under discussion. Midwives reported a disturbingly high incidence of mental health problems among the dispersed or pre-dispersal women they had looked after.
The social impact of dispersal
All the women interviewed had been dispersed or relocated during their pregnancy though only two of them were moved away from London and South East England. Fourteen women experienced multiple moves during pregnancy or immediately after the birth, including one woman, who was moved six times during her pregnancy and once after delivery before she found settled accommodation.
Women were very distressed about being dispersed away from areas in which they had strong social networks and established healthcare provision. In several cases dispersal separated women from the father of their baby.
Initial accommodation
Over half the women spent time in Initial Accommodation before being moved on. Women’s feelings about Initial Accommodation were generally very adverse. They complained about dirty bathrooms and toilets, bad or inedible food, being forced to sterilise bottles in the toilets, safety issues, rooms on upper floors without lifts, and being assigned top bunks.
One woman was sent to Initial Accommodation within London and had to stay there for a ‘protected period’ of four weeks either side of delivery, in accordance with new UKBA guidance. However, this provided no improvement over dispersal to other areas in terms of social support, access to healthcare, suitable accommodation or even the experience of travel.
Timing of dispersal
Fourteen women were in their final trimester of pregnancy and eight were in their last month when they were moved. Two women were dispersed one day before they gave birth and another woman gave birth two days after dispersal. Women reported being moved despite their treating clinicians advising against travel.
Travel to the dispersal areas
The journeys were often very distressing. Women were often moved at very short notice, without being informed of their destination or the distance to be travelled until the last minute, or when they would be picked up. Several women reported not being able to eat during the journey, inadequate toilet breaks, and lack of assistance with luggage.
Conditions on arrival
Some women received little help to register with a GP in their new location. Women with other children faced problems enrolling their existing children into school or nursery.
Accommodation for pregnant women or those who had recently given birth was often inappropriate. There was rudimentary equipment for the baby but little effort was made to ensure adequate hygiene and sanitary facilities for newborns. Women often had to climb several flights of stairs to their rooms.
Managing financially
Women found that they had insufficient money for essential needs. The worst affected were those receiving cashless support, either on section 4 or because they were based in full-board hostels and also received no cash except a minimal pregnancy payment of £3, or £5 per week once their baby was born. One woman’s support was stopped while she was in hospital having her baby, because her asylum claim had been refused, and it took two weeks to get section 4 support during which time she had no money.
The impact of dispersal on women’s health and maternity care
Midwives attached great importance to regular antenatal contact with vulnerable women, emphasising especially continuity of care and of carer in order to build up trust where there were evident health and social care issues. However, most women’s antenatal care was interrupted as a result of dispersal, often with breaks of several weeks before they could again receive maternity care in the new area, mainly due to difficulties in registering with GPs. Two women interviewed had been booked into three different maternity units because of multiple moves.
The interruption of care could have serious consequences for conditions such as diabetes or hepatitis, which required regular monitoring or where treatment needed to be sustained during pregnancy. It also prevented the implementation of multi-agency care packages which were particularly important if children were deemed to be at risk.
Although nearly all women who had booked into maternity services before they were dispersed had handheld records, nevertheless, booking appointments, tests and scans often had to be repeated in the new unit to ensure that results were accurate and referred to the right woman. Information on sensitive issues such as domestic violence was not normally stored on handheld records.
Dispersal had an extremely adverse impact on women’s mental health. At least five women had clinically diagnosed postnatal depression. Many women found themselves in the dispersal area with no social support. They therefore had to make their own arrangements to go into hospital when they went into labour, and in some cases were frightened to call ambulances. They also had anxieties about who would look after their children, and in some cases arranged very ad hoc childcare.
None of the midwives interviewed were informed by UKBA of when women were being moved, or whether they were fit to travel. This wasted valuable time and public resources looking for them, and prevented planning or information sharing between maternity units. Midwives often asked women due to be dispersed to contact them on arrival at their dispersal destination, so that they could alert the maternity service in the new area, but this left the responsibility for doing this with the woman.
Where there were anxieties about a woman’s or baby’s welfare, midwives often tried to get a dispersal deferred or stopped, but letters to UKBA were rarely acknowledged or responded to. Midwives frequently spent a great deal of time trying to liaise with UKBA on behalf of a woman about whom they were concerned.
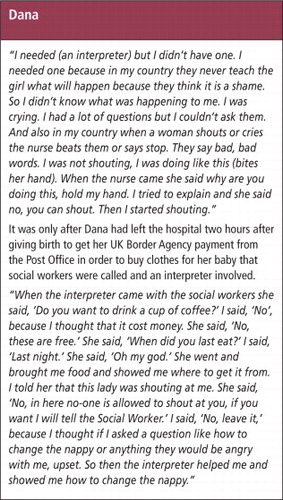
Women’s experience of labour and the postnatal period
Eight women interviewed were in labour without any birth companion present. None of the women had an interpreter present during labour, and four had no one with them who could help interpret. While the provision of an interpreter is not the responsibility of UKBA, the lack of continuity of maternity care makes it less likely that appropriate interpreting services would be provided.
Almost all women found the postnatal period very stressful. Some felt completely unsupported because they had been moved from family and friends. Accommodation on upper floors was unsuitable for women who were in pain and weak after giving birth. Financial provision was inadequate to meet their needs, and many women had problems obtaining UKBA Maternity Payments. Women on section 4 support were unable to use public transport even though they were in pain after surgical interventions in delivery because their support was cashless.
Addressing complex social factors among pregnant women seeking asylum
In spite of some improvement, the UKBA’s 2012 Healthcare and Pregnancy Dispersal Guidance falls far short of addressing the issues identified in the interviews with the women and midwives or in the NICE Guidelines on Pregnancy and Complex Social Factors. The most important recommendation of the UKBA 2012 guidance is for dispersal to be deferred during the ‘protected period’. However, this fails to recognise the importance of postnatal care and tests for at least six weeks postnatally.
The UKBA 2012 guidance makes no mention of mental health issues, or other health needs arising in pregnancy, nor of many underlying health problems that may affect women during their pregnancies. It does not address women’s need for social support throughout pregnancy and labour. Loss of social support, not only on dispersal, but also for women kept in Initial Accommodation for at least eight weeks during the ‘protected period’, is very damaging to women’s well-being.
The study shows that Initial Accommodation is wholly inappropriate for women in advanced pregnancy. In opting for women in the ‘protected period’ to be accommodated in Initial Accommodation, the UKBA is continuing to regard pregnancy and birth as a logistic rather than as a health care issue.
While formally recognising some aspects of antenatal care such as the need not to delay tests or to disrupt a programme of tests, the 2012 guidance does not indicate how its policy can contribute to avoiding such disruption earlier than four weeks before the expected date of delivery.
The policy of maintaining very low levels of cashless support forces women into poverty and limits the uses to which the support may be put, especially by denying them cash for public transport or preferred types of food from small shops rather than supermarkets.
Dispersal of women in pregnancy, especially late in pregnancy, inevitably disrupts maternity care which is a continuous and cumulative process. Maternity care costs are increased by wasting valuable resources in searching for women who have been moved without the service being informed, and by generating a need for repeat tests and scans.
The way forward
This study demonstrates a need for the UKBA to reconsider its policy of dispersing pregnant women, and for new guidance to be developed in conjunction with experts in the maternity care of vulnerable women. We urge it to take seriously the recommendations stemming from this study.
Recommendations
1. Recognise complex needs in pregnancy
UKBA should recognise pregnancy in women seeking asylum as involving complex needs, including mental health, family and social circumstances, experience of trauma and violence, pregnancy-related conditions, and underlying health conditions, and reflect this in its policies and processes.
2. Maintain women’s residence where they can access existing support
Pregnant women should not normally be dispersed. Case owners should ensure that pregnant women are accommodated in an area where they can continue to access existing GP and maternity care. This should mean that they are also within reach of existing social and family support.
3. Women pregnant on arrival in the UK
In order to avoid lengthy stays in Initial Accommodation women asylum seekers who arrive in the UK already pregnant, should be prioritised for dispersal and moved quickly, if they are in the early stages of pregnancy. If they are in a later stage of pregnancy they should be offered suitable accommodation near the port of entry.
4. Women applying for support late in pregnancy
No woman should be dispersed after 34 weeks gestation, or sooner than 6 weeks postnatally. This means extending the ‘protected period’ from at least 6 weeks before the expected date of delivery to at least 6 weeks after. No woman should be dispersed after delivery until she has been discharged from postnatal care and a full medical report is available on her and her baby.
If women apply for support late in pregnancy and support is granted while they are within the ‘protected period’ and they cannot be accommodated where they were formerly living, their accommodation needs should be met in safe, suitable accommodation outside Initial Accommodation. Women at this late stage of their pregnancy should not be moved out of their area and suitable private accommodation should be commissioned if necessary.
5. Full risk assessment before unavoidable dispersal
If a dispersal is unavoidable, before any dispersal takes place there must be a full assessment of needs and risk associated with dispersal, to be carried out by the woman’s current treating midwife/obstetrician and other clinician (if she is receiving care for another long-term condition). If the woman is not receiving maternity or other healthcare this assessment should be carried out by a midwife with expertise in the care of vulnerable women. | |||||
Such an assessment should specify any accommodation requirements that need to be met. | |||||
Such an assessment should certify the woman’s fitness to travel. | |||||
No dispersal of a pregnant woman should take place before such an assessment has been carried out. | |||||
Responsibility for ensuring such an assessment takes place lies with UKBA, not with the woman seeking asylum. | |||||
6. Transfer arrangements before unavoidable dispersal
If a pregnant woman has unavoidably to be dispersed to another area, case owners should notify both her current treating midwife/obstetrician and other clinician (if she is receiving care for another long-term condition) and a named contact in the Healthcare team at the dispersal destination. No pregnant woman who has booked into maternity care should be dispersed without arrangements having been made for her to be received into maternity care in the dispersal area. The receiving midwife/obstetrician and other relevant clinician should have received a full medical report and detailed medical records as well as the woman having her handheld notes.
7. Ensure adequate financial support throughout pregnancy
Given the particular health risks facing asylum seeking women during pregnancy and after birth, asylum support levels for pregnant women on both section 95 and section 4 support should never fall below the equivalent of 70% of Income Support. | |||||
Financial support should always be provided in cash during pregnancy and until the end of the postnatal period for women on section 4 support. | |||||
Sufficient financial support should be provided to pregnant women and new mothers in full- board hostels in recognition that full-board does not adequately meet their needs. | |||||
No pregnant woman’s asylum support payments and accommodation should be stopped until after completion of all antenatal and postnatal care, regardless of any decision on her asylum case. | |||||
In view of the health problems for both pregnant women and their unborn babies caused by destitution, UKBA should provide support to all pregnant women seeking asylum whose asylum claim has been refused. | |||||
The timeframes for application for Maternity Payments should be eleven weeks before the expected date of delivery until three months after the birth (thereby matching those of the Sure Start Maternity Grants). Section 4 Maternity Payment levels should be raised to section 95 levels. | |||||
8. Monitor negative impacts of dispersal on maternity care
The Department of Health should facilitate data collection by NHS Trusts of incidents in which UKBA dispersal and relocation practices have prevented delivery of effective maternity care. The Department of Health should also facilitate communication of the data to the UKBA.
9. Develop improved support guidance for pregnant women seeking asylum
The UKBA should, as a matter of urgency, engage in discussions with representatives of midwives, obstetricians, general practitioners, and relevant voluntary organisations to develop dispersal policies for pregnant women and women who have recently delivered, which are compatible with NICE guidance on the maternity care of women with complex social factors.
Note
Reprinted with kind permission of Maternity Action. Full report is at: http://www.refugeecouncil.org.uk/assets/0002/6402/When_Maternity_Doesn_t_Matter_-_Ref_Council__Maternity_Action_report_Feb2013.pdf.
A short film describing the situation of pregnant women asylum seekers in the UK, including several of the women in the study and a midwife, which was prepared to accompany the report, is at: http://www.refugeecouncil.org.uk/maternity.
A two-part video of a seminar about this report was held on 9 July 2013. The two parts can be accessed at: http://vimeo.com/70620053 and http://vimeo.com/70641681.