Abstract
Introduction
The occipitocervical junction presents a unique, complex, biomechanical interface between the cranium and the upper cervical spine. Occipitocervical fixation has undergone significant evolution due to advances in operative techniques and instrumentation techniques.
Objective
This study was done to evaluate clinical picture, radiographic findings and results of occipitocervical fusion in 10 patients with craniocervical instabilities. Also to compare these results with other results reported in the literature.
Methods
This retrospective study reviewed 10 patients who underwent occipitocervical fixation for craniocervical instabilities between April 2007 and October 2010 in Alexandria hospitals. There were 7 males and 3 females and their ages ranged from 16 to 63 years with mean age of 42.1 years. As regards the clinical presentation, all patients had presented with neck pain before surgery, 8 patients (80%) with myelopathy, and 8 patients (80%) had presented with a neurological deficit either motor or sensory or both. The etiologies of occipitocervical instability in this study were trauma in three patients, rheumatoid arthritis in three patients, tumor in two patients and Down syndrome in two patients. All patients had preoperative craniocervical plain X-ray, CT and MRI examination. All patients underwent occipitocervical fixation surgery with various fixation systems and autologous bone grafts for fusion. Fusion was assessed by plain cervical X-ray films and CT scan, and the neurological outcome by Frankel grade. The mean follow-up period was 14.7 months (range, 4–24 months) including both clinical and radiological examinations.
Results
There were no operative mortalities or vascular injuries in this series. Two patients showed transient neurological deterioration postoperatively that had resolved within three months. Two cases had superficial wound infection and one case had cerebrospinal fluid leak. The mean operation time was 207 min (range 130–320 min) and the mean volume of blood loss was 354 mL (range 120–750 mL). Neck pain improved in all patients and no new instability developed at adjacent levels. Regarding the Frankel grade, five patients had shown improvement (Three patients improved from Frankel grade C to grade D, one patient from grade A to grade B and one patient from grade D to grade E), while five patients remained stationary at the same grade. At the last follow-up examination period, a solid fusion was achieved in nine patients out of ten (90%).
Conclusion
Occiptocervical fixation is indicated in the management of craniocervical instabilities resulting from trauma, rheumatoid arthritis, tumors and congenital anomalies of the craniocervical junction. Accurate imaging studies and proper patient selection are the keys to a successful outcome. Occipitocervical fusion procedures can be performed with low morbidity. A comprehensive knowledge of the anatomy of the occipital-cervical junction is imperative. A wide variety of stabilization techniques and instrumentation systems are currently available, each of which has its own advantages and disadvantages.
1 Introduction
The occipitocervical junction presents a unique, complex, biomechanical interface between the cranium and the upper cervical spine.Citation1 Occipitocervical fusion is performed primarily in craniocervical instability due to congenital and post-traumatic deformities, infections, tumors and inflammatory conditions.Citation2–Citation9
Occipitocervical instability may manifest as disabling pain, cranial nerve dysfunction, paralysis, or even sudden death. Stabilization and fusion is required to prevent these complications. Occipitocervical fusion and instrumentation is a technically challenging procedure that can be accomplished successfully with careful attention to local anatomy and working knowledge of the various fixation options. The aim in occipitocervical fixation is to avoid injuring the nerve root, the spinal cord and the vertebral artery, and to obtain rigid fusion.Citation10 Absence or hypoplasia of the occipital bone and co morbidities that would prevent an operative procedure or the prone positioning are contraindications for occipitocervical fusion.Citation2
Occipitocervical fixation has undergone significant evolution due to advances in operative techniques and instrumentation techniques. This procedure has evolved from simple autograft on lay fusion techniques to sublaminar wiring techniques and, most recently, rigid occipital plating with bicortical screws connected via rods to atlantoaxial or subaxial screw fixation.Citation3,Citation11–Citation17
This study was aimed to evaluate clinical picture, radiographic findings and results of occipitocervical fusion in 10 patients with craniocervical instabilities. Also to compare these results with other results reported in the literature.
2 Methods
This retrospective study was carried out on 10 patients who underwent occiptocervical fixation in Alexandria hospitals between April 2007 and October 2010. Their medical records and imaging studies were reviewed. There were 7 males and 3 females and their ages ranged from 16 to 63 years with mean age of 42.1 years.
As regards the clinical presentation, all patients had presented with neck pain before surgery, 8 patients with myelopathy, and 8 patients had presented with a neurological deficit either motor or sensory or both (Frankel classification of these 10 patients are shown in ).
Table 1 Frankel classification of 10 patients with occipitocervical instability.
The etiologies of occipitocervical instability in this study were trauma in three patients, rheumatoid arthritis in three patients, tumor in two patients and Down syndrome in two patients. All cases had preoperative craniocervical plain X-ray, CT and MRI examination. Preoperative traction was performed in two patients; one patient with trauma and the other with rheumatoid arthritis. All patients wore rigid neck collar postoperatively until fusion was achieved.
All patients underwent occipitocervical fixation surgery with various fixation systems and autologous bone grafts for fusion. All patients received awake intubation, and the surgical position was prone. The incisions were at midline, from external occipital protuberance to cervical area. After adequate exposure of suboccipital and posterior cervical areas, The methods used for occipitocervical fixation included; sublaminar wires and cables in three cases, wire-rod system in two cases and screw-rod system in five cases.
Cervical laminectomy was done in three cases depending on the clinical and radiological findings. Finally, the autologous bone grafts harvested from posterior iliac crest were put between C1 and C2 or posterolaterally. Transoral decompression was performed in one patient with basilar invagination due to rheumatoid arthritis prior to the posterior fixation procedure.
The Frankel grade () was used to assess neurological outcome postoperatively. Fusion was assessed by plain cervical X-ray films and CT scan. Fusion was defined as successful if 2 criteria were met: (1) there was no relative movement between the fused motion segments in dynamic views of cervical X-ray; (2) the bone grafts became a uniform bone mass in imaging studies. The mean follow-up period was 14.7 months (range, 4–24 months).
Summary data for these 10 patients are listed in
Table 2 Summary data of 10 patients who underwent occiptocervical fixation.
3 Results
The most common pattern of occipitocervical instability in this study was atlantoaxial sublaxation observed in eight patients (80%). Subaxial cervical instability was associated to occipitocervical instability in four cases (40%). In the present study, occipitocervical fixation was performed from occiput to C2 in two cases, occiput to C4 in two cases, occiput + C3 to C5 in one case, Occiput + C3 + C5 in one case, occiput + C1 + C3 in one case, occiput + C2 + C3 in one case, occiput + C2 to C5 in one case, and occiput to C3 in one case (). The mean operation time was 207 min (range 130–320 min) and the mean volume of blood loss was 354 mL (range 120–750 mL).
Perioperative mortalities and morbidity
There were no operative mortalities or vascular injuries in this series. Two patients showed transient neurological deterioration postoperatively that had resolved within three months. Two cases had superficial wound infection; one of them responded to antibiotic treatment and the other required surgical debridement. CSF leak occurred in one case that stopped with conservative measures in the form of lumbar puncture and diuretics.
Outcome of cases
Patients with preoperative complaint of neck pain respond well to surgery with complete resolution in all cases (100%). On contrast only 37.5% of the patients with myelopathic manifestations had improved (three patients out of eight). At the last follow up postoperative examination period, five patients had improved (Three patients improved from Frankel grade C to grade D, one patient from Frankel grade A to grade B and one patient from Frankel grade D to grade E), while five patients remained stationary at the same Frankel grade (). No new instability developed at adjacent levels in the follow-up radiographs. A solid fusion was achieved in nine patients out of ten (90% of the cases). The mean fusion time of these 9 patients was 5.3 months (range, 4–8 months).
Table 3 Outcome of patients in relation to the etiology and the technique of fixation.
4 Discussion
The craniocervical junction is the most mobile of the upper cervical spine especially in children. It is uniquely adapted for stability and motion.Citation18 Occipitocervical instability may be caused by trauma, rheumatoid arthritis, neoplastic disease, inflammatory disease and congenital anomalies. The common result of occipitocervical instability is cervicomedullary neural tissue compression, with development of symptoms and signs of cervical radiculomyelopathy and brain stem compression as well as deformities of the craniocervical region.Citation19,Citation20 The solution to occipitocervical instability is occipitocervical fixation with bone fusion. The goals of occipitocervical fixation are regaining normal alignment, ensuring adequate neural tissue decompression and achieving structural stability. Occipitocervical fixation is a challenging field in spinal surgery. Many techniques for occipitocervical fixation had been reported in the literatureCitation21–Citation29 using various internal fixation instruments.
This study focused on occipitocervical fixation whether traumatic or non traumatic. Similar reports in the literature were found to be matching with this study as Hsu et al.Citation20, Ogihara et al.Citation30, and Song et al.Citation31 series, while other reports were focused either on traumatic cases alone as Lee et al.Citation32 series or non traumatic cases as in Bongartz et al.Citation33 and Motosuneya et al.Citation34 series.
Like the previously published seriesCitation20,Citation32,Citation33 neck pain was a main presenting symptom in all cases of occipitocervical instability. Neurological deficit (motor, sensory or both) and myelopathy were also found to be a common clinical presentation in this study (80% with neurological deficit and 80% with myelopathy). Although cranial nerve deficit and ventilation impairment were not a presenting feature in this series, othersCitation19,Citation35 had reported in their cases.
Trauma and rheumatoid arthritis were the most frequent causes of occipitocervical instability in this study (three cases each) followed by tumor and Down syndrome (two cases each). This was consistent with what was reported by Song et al.Citation31 who operated 32 patients with craniocervical instabilities and found that trauma and rheumatoid arthritis were the main etiology in 22 cases.
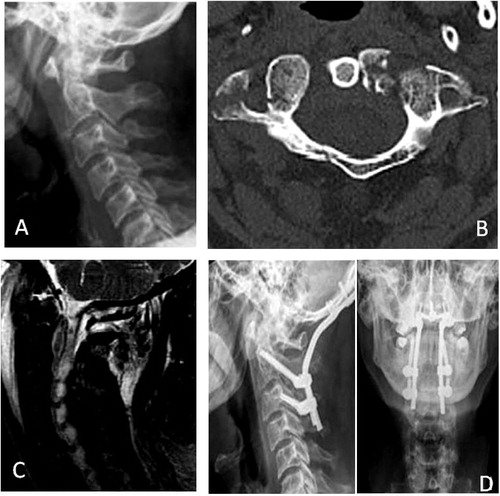
The indication of occipitocervical fixation in the traumatic cases was atlantoaxial sublaxation in two cases () and atlantoaxial sublaxation associated with C2–C3 sublaxation in the third case. Atlantoaxial fixation was not feasible in these cases (due to fractured C1 posterior arch in one case, C1 lateral mass fracture in the second case, fracture C2 pedicle and lamina in the third case) and occipitocervical fixation was mandatory. This was consistent with what was found in the literature.Citation30,Citation32 Other indications of occipitocervical fixation in trauma cases include; atlantooccipital dislocation, C1–C2 instability which cannot be completely reduced, patients who have had a transoral odontoidectomy, those who have an incompetent C1 lamina or abnormal course of the vertebral artery, all of which make a C1–C2 posterior fusion impossible.Citation36–Citation39
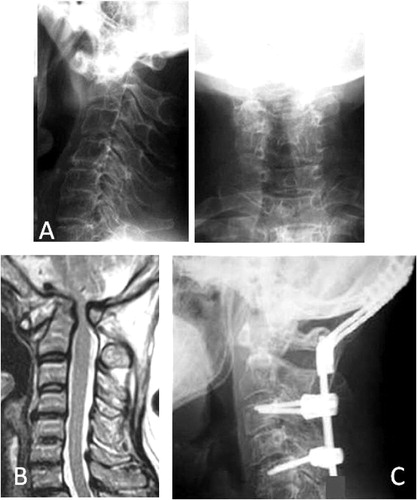
The second common cause of occipitocervical instability in this series was rheumatoid arthritis that found in three patients (). Rheumatoid arthritis of the cervical spine leads to a spectrum of joint erosions and deformity resulting in spinal stability. The most common patterns of cervical instability seen in rheumatoid arthritis are atlantoaxial subluxation (AAS), followed by basilar invagination (superior migration of odontoid = SMO) and subaxial subluxation (SAS). Combined patterns of cervical instabilities are not uncommon in rheumatoid arthritis.Citation40–Citation43 The indications of occipitocervical fusion in the three rheumatoid patients in this study was the combination of AAS, SMO and SAS. This was consistent with the indications mentioned in Pham et al.Citation44 series in which occipitocervical fixation was performed in 18 patients with rheumatoid arthritis.
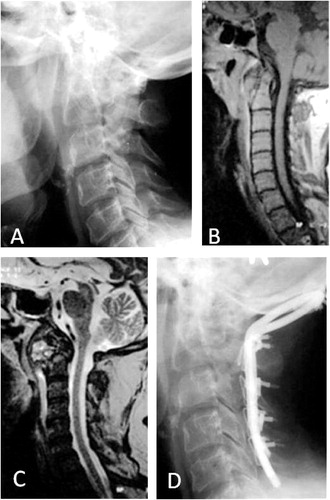
Metastatic spine tumors occur in 5–10% of all cancer patients.Citation45 Cervical spine involvement is relatively uncommon, accounting for less than 10% of all spinal metastases. The most prevalent tumors are lung, breast, prostate, kidney, and thyroid.Citation46 Two cases of metastatic cervical tumors were included in this series; one male suffered from metastasis from lymphoma and the second was a female with metastatic tumor from breast cancer. In these two cases there was a variable degree of neoplastic destruction of C1 and C2 vertebrae with a resultant compression of the cervicomedullary junction. Cervical laminectomy and decompression were needed in these two cases together with occipitocervical fixation (). These findings correspond to the results of Hsu et al.,Citation20 Song et al.Citation31 and Bongartz et al.Citation33 who performed occipitocervical fixation for similar pathologies.
Two patients with Down syndrome were operated upon in this series for occipitocervical fusion. Atlantoaxial subluxation was the main pathology in these two cases accompanied by atlantooccipital subluxation. Down syndrome is the commonest inherited chromosomal disorder occurring in 1 in 660 live births. Children and adults with Down syndrome are prone to cervical spine disease, including instability, although the natural history is unclear. The majority of pathology occurs at the craniocervical junction particularly at the atlantoaxial and atlantooccipital joints.Citation47,Citation48 About 1% only of all patients with Down syndrome who present with instabilities that require surgical intervention.Citation49
Various systems had been developed for internal fixation of the occipitocervical spine including; sublaminar wires and cables, wire-rod construct, hook-rod system, plate-screw system, and rod-screw system.Citation50 The methods of occipitocervical fixation used in this series included; sublaminar wires and cables in three cases, wire-rod system in two cases and screw-rod system in five cases.
The sublaminar wire and cable method is an easy and simple method however is not indicated after laminectomy or laminoplasty because the wires cannot be anchored at the laminae. In addition, passing a wire under the lamina may cause spinal cord injury during the procedure and possibly spinal cord compression due to recoil of the wire. Also passing wire through the occiput can be dangerous because the incidence of dural tears reported with this procedure was 25%.Citation27
Sonntag and DickmanCitation22 described the wire-rod technique; they used a grooved titanium fixation rod which was bent into a “U” shape and contoured to fit the cervical curvature and fixed to the occipital bone and cervical laminae using wires. This construct also needs intact posterior cervical elements for sublaminar wiring, and is not suitable for patients whose posterior elements are defective or have to be removed for decompression. The advantages of the wire-rod construct include being technically simple, safe and economical. For patients with poor bone quality, such as rheumatoid arthritis with osteoporosis, this technique may be the surgery of choice because the screw purchase is not secured. However the wire rod construct does not provide immediate postoperative stability and postoperative rigid external fixation such as halo-vest is necessary, usually for at least 12 weeks.Citation11,Citation23
Recently the screw-based construct (plate-screw system, rod-screw system) for occipitocervical fixation had been developed. This system fixes the occipital bone to the atlantoaxial and subaxial cervical spine through plates or rods. Transarticular C1–C2 screws, C1 lateral mass screws, C2 pedicle screws and subaxial lateral mass screws are the most commonly used with occiput fixation and have shown to increase construct rigidity of occipitocervical fixation.Citation51 The screw-based construct (plate-screw system, rod-screw system) provides immediate postoperative stability, so postoperative rigid external fixation is not needed in most cases, which makes patients more comfortable.Citation24,Citation25,Citation27,Citation28 This construct provides more rigidity biomechanically than the wire-rod construct, and can be applied to patients whose posterior elements are defective or need to be removed for decompression. The disadvantages include potential vertebral artery and cervical root injury due to cervical screw purchase, consequently these techniques should be considered technically demanding.Citation51–Citation53 Potential vascular injuries with occipitocervical fixation include excessive venous hemorrhage and vertebral artery injury. These complications are especially frequent in patients with severe deformity or shortening of the vertebral body and misalignment of the spinal column. Most vascular complications occur during the exposure of the C1 lateral mass or the C2 pars interarticularis and introduction of screws.Citation54–Citation56 There were no operative mortalities or vascular injuries in this series. These findings correspond to the results of Bongartz seriesCitation33 in which nine patients were operated for occipitocervical fusion without any vascular complications. However the screw-based construct is expensive and not suitable in patients with poor bone quality as occurred in one patient with rheumatoid arthritis in whom C1 C2 C4 screws could not be applied
In this study two patients showed transient neurological deterioration postoperatively. In one of them, the neurological deterioration was believed to be related to the introduction of the sublaminar wires while in the second, laminectomy in a stenotic canal may be the cause. However the neurological deterioration in these two patients was transient and both had shown improvement with conservative treatment and physiotherapy. Such complications had been reported in the literatureCitation57 to be associated with occipitocervical fixation. Two cases had superficial wound infection in this series. One case was treated successfully using the proper antibiotic after performing culture and sensitivity from the wound, while the second patient was diabetic and required a surgical debridement with the antibiotic management. Similarly Hsu and colleaguesCitation20 who retrospectively reviewed 9 patients with occipitocervical fixation had reported a case of wound infection. One case with cerebrospinal fluid leak was reported in this study. Intraoperative dural tear was found in one of traumatic cases with fracture of posterior arch of atlas that was repaired immediately. However CSF leak had occurred postoperatively but responded well to repeated lumbar puncture and diuretics. This finding was not consistent with Ogihara et al.Citation30 who treated 23 patients with disorders at the craniocervical junction that required posterior occipitocervical reconstruction and did not report any case of CSF leak. In this study, the mean operation time was 207 min (range 130–320 min) and the mean volume of blood loss was 354 mL (range 120–750 mL. Similar to this study, Motosuneya et al.Citation34 in their series of 11 patients who had undergone occipitocervical fusion for non-traumatic upper cervical instability had reported a mean operative time of 189 min (range 120–240 min), and a mean volume of blood loss of 297 mL (range 135–850 mL). While in Ogihara et alCitation30 series of twenty three patients with occipitocervical fusion, the mean operative time was averaged 350 min (range 163–660 min) and the mean intraoperative blood loss 579 (range 20–1870 mL).
In this study, neck pain had improved in all patients while myelopathic manifestations had improved in three patients (37.5%). Three patients improved from Frankel grade C to grade D, one patient from Frankel grade A to grade B and one patient from Frankel grade D to grade E while the other patients remained at the same Frankel grade. In Lee and colleaguesCitation32 series in which 16 patients with traumatic upper cervical spinal instability were operated for occipitocervical fixation; three patients improved from Frankel grade D to grade E while other patients remained at the same Frankel grade. Many authors had reported a high incidence of successful postoperative fusion (range from 75% to 100%) with occipitocervical fixation regardless the fusion method and underlying pathologies.Citation25,Citation38 In the present study, successful fusion had occurred in nine patients (90% fusion rate). Only one patient with rheumatoid arthritis did not show any signs of fusion at the last follow up period after 4 months. This patient was the last patient in this study and there was no enough time to follow him for a longer period where a successful fusion can still occur. The mean fusion time in this series was 5.3 months (range 4–8 months) which is similar to that reported in other series.Citation20 No new instability developed at adjacent levels in the follow-up radiographs of our patients.
5 Conclusion
Occiptocervical fixation is indicated in the management of craniocervical instabilities resulting from trauma, rheumatoid arthritis, tumors and congenital anomalies of the craniocervical junction. Accurate imaging studies and proper patient selection are the keys to a successful outcome. Occipitocervical fusion procedures can be performed with low morbidity. A comprehensive knowledge of the anatomy of the occipital-cervical junction is imperative. A wide variety of stabilization techniques and instrumentation systems are currently available, each of which has its own advantages and disadvantages.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine
Reference
- J.R.VenderP.J.HouleS.HarrisonOccipital-cervical fusion using the Locksley intersegmental tie bar technique: long-term experience with 19 patientsSpine J22002134141
- C.G.RandazzoB.LeBudeJ.RatliffOcciput–Cervical FixationSpine Trauma, Part 11192010127
- K.AbumiA.AvadhaniA.ManuOccipitocervical fusionEur Spine J192010355356
- B.GuiotR.G.FesslerComplex atlantoaxial fracturesJ Neurosurg (Spine 2)911999139143
- M.VisocchiF.D.RoccoM.MeglioCraniocervical junction instability: instrumentation and fusion with titanium rods and sublaminar wires. Effectivenes and failures in personal experienceActa Neurochir.1452003265272
- C.A.DickmanS.M.PapadopoulosV.K.H.SonntagTraumatic occipitoatlantal dislocationsJ Spinal Disor61993300313
- F.H.ShenD.SamartzisL.G.JenisRheumatoid arthritis: evaluation, surgical management of the cervical spineSpine J6892004700
- L.LablerK.EidA.PlatzAtlanto-occipital dislocation: four case reports of survival in adults and review of the literatureEur Spine J1322004172180
- H.KollerU.HolzA.AssuncaoTraumatic Atlantooccipital Dislocation Critical Review: Diagnosis, Classification and Treatment, and Explanative Case Report. European J of Trauma 2006; 32: 271–9. 3- Abumi K, Avadhani A, Manu A, et al. Occipitocervical fusionEur Spine J192010355356
- A.VaccaroM.LimJ.LeeIndications for surgery and stabilization techniques of the occipito-cervical junctionInjury Int J Care Injured362005SB44SB53
- J.J.BaskinC.A.DickmanV.K.H.SonntagOccipitocervical fusionH.R.WinnR.G.DaceyYoumans Neurological Surgery2004SaundersPhiladelphia46554670
- N.A.EbraheimH.ElgafyR.XuBone graft harvesting from iliac and fibular donor sites: techniques and complicationsJ Am Acad Orthop Surg92001210218
- K.AbumiT.TakadaY.ShonoPosterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systemsSpine24199914251434
- A.FaureE.BordR.Monteiro da SilvaOccipitocervical fixation with a single occipital clamp using inverted hooksEur Spine J719988083
- V.HeideckeN.G.RainovW.BurkertOccipito-cervical fusion with the cervical Cotrel-Dubousset rod systemActa Neurochir1401998969976
- P.KorovessisP.KatonisA.AligizakisPosterior compact Cotrel-Dubousset instrumentation for occipitocervical, cervical and cervicothoracic fusionEur Spine J101998385394
- P.PaquisV.BreuilM.LonjonOccipitocervical fixation using hooks and screws for upper cervical instabilityNeurosurgery441999324331
- A.H.MenezesV.C.TraynelisAnatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b)Nerv Syst24200810911100
- R.P.NockelsC.I.ShaffreyA.S.KanterOccipitocervical fusion with rigid internal fixation: long-term follow-up data in 69 patientsJ Neurosurg Spine72007117123
- Y.H.HsuM.L.LiangY.S.YenUse of Screw-Rod System in Occipitocervical FixationJ Chin Med Assoc72120092028
- C.E.WolflaAnatomical, biomechanical, and practical considerations in posterior occipitocervical instrumentationSpine J62006225S232S
- V.K.SonntagC.A.DickmanCraniocervical stabilizationClin Neurosurg401993243272
- J.R.VenderA.J.RekitoS.J.HarrisonThe evolution of posterior cervical, occipitocervical fusion, instrumentationNeurosurg Focus162004E9
- H.DeutschR.W.HaidJrG.E.RodtsJrOccipitocervical fixation: long-term resultsSpine302005530535
- I.OdaK.AbumiL.C.SellBiomechanical evaluation of five different occipito-atlanto-axial fixation techniquesSpine24199923772382
- S.C.LeeJ.F.ChenS.T.LeeComplications of fixation to the occiput—anatomical and design implicationsBr J Neurosurg182004590597
- C.E.SutterlinJ.R.BianchiD.N.KunzBiomechanical evaluation of occipitocervical fixation devicesJ Spinal Dis142001185192
- B.L.CurrierP.J.PapagelopoulosP.G.NealeBiomechanical evaluation of new posterior occipitocervical instrumentation systemClin Orthop Rel Res4112003103115
- G.H.StockA.R.VaccaroA.K.BrownContemporary posterior occipital fixationJ Bone Jt Surg Am88200616421649
- N.OgiharaJ.TakahashiH.HirabayashiLong-term results of computer-assistedposterior occipitocervical reconstructionWorld Neurosurg7362010722728
- G.C.SongK.S.ChoD.S.YooSurgical Treatment of Craniovertebral Junction Instability: Clinical Outcomes and Effectiveness in Personal ExperienceJ Korean Neurosurg Soc4820103745
- S.C.LeeJ.F.ChenS.T.LeeClinical experience with rigid occipitocervical fusion in the management of traumatic upper cervical spinal instabilityJournal of Clinical Neuroscience132006193198
- E.B.BongartzTwo asymmetric contoured plate-rods for occipito-cervical fusionEur Spine J1332004266273
- T.MotosuneyaS.HirabayashiH.YamadaOccipitocervical fusion usin g a hook and rod system between cervical levels C2 and C3J Clin Neurosci162009909913
- H.KollerU.HolzA.AssuncaoTraumatic Atlantooccipital Dislocation Critical Review: Diagnosis, Classification and Treatment, and Explanative Case ReportEur J Trauma322006271279
- R.C.SassoB.JeanneretK.FischerOccipitocervical fusion with posterior plate and screw instrumentation: a long term follow-up studySpine19199423642368
- C.B.HuckellJ.M.BuchowskiW.J.RichardsonFunctional outcome of plate fusions for disorders of the occipitocervical junctionClin Ortho Rel Res3591999136145
- F.L.ValeM.OliverD.W.CahillRigid occipitocervical fusionJ Neurosurg (Spine 2)911999144150
- A.A.MadawiA.T.H.CaseyG.A.SolankiRadiological and anatomical evaluation of the atlantoaxial transarticular screw fixation techniqueJ Neurosurg861997961968
- F.H.ShenD.SamartzisL.G.JenisRheumatoid arthritis: evaluation and surgical management of the cervical spineSpine J42004689700
- E.R.KolenM.H.SchmidtRheumatoid arthritis of the cervical spineSemin Neurol222002179186
- S.D.BodenL.D.DodgeH.H.BohlmanRheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recoveryJ Bone Joint Surg Am75199312821297
- C.R.ClarkD.D.GoetzA.H.MenezesArthrodesis of the cervical spine in rheumatoid arthritisJ Bone Joint Surg Am711989381392
- X.V.PhamP.BancelC.J.MenkesUpper cervical spine surgery in rheumatoid arthritis: retrospective study of 30 patients followed for two years or more after Cotrel- Dubousset instrumentationJoint Bone Spine672000434440
- K.HammerbergSurgical treatment of metastatic spine diseaseSpine17199211481153
- T.TolliF.CammisaJ.LaneT.MartinMetastatic disease of the spineS.WieselS.BodenSeminars in Spine Surgery1995WB SaundersPhiladelphia, PA277287 Vol. 7
- J.RossL.MylesCervical spine problems in childrenCurr Orthopaed202006274285
- M.CrostelliM.MarianiO.MazzaCervical fixation in the pediatric patient: our experienceEur Spine J182009S20S28
- U.WeberY.RobinsonR.KayserRare pathological alterations of the upper cervical spine requiring surgical treatmentOrthopade J3532006296305
- C.D.WinegarJ.P.LawrenceB.C.FrielA systematic review of occipital cervical fusion: techniques and outcomesJ Neurosurg Spine1312010516
- J.GabrieA.M.MuzumdarS.KhalilA novel crossed rod configuration incorporating translaminar screws for occipitocervical internal fixation: an in vitro biomechanical studySpine J1120113035
- C.M.PuttlitzR.P.MelcherF.S.KleinstueckJ.HarmsD.S.BrafordJ.C.LotzStability analysis of craniovertebral junction fixation techniquesJ Bone Joint Surg Am86A2004561568
- A.ShadS.S.ShariffP.J.TeddyT.A.D.Cadoux-HudsonCraniocervical fusion for rheumatoid arthritis: comparison of sublaminar wires and the lateral mass screw craniocervical fusionBr J Neurosurg162002483486
- R.LallN.J.PatelD.K.ResnickA review of complications associated with craniocervical fusion surgeryNeurosurgery J675201013961403
- H.S.AnR.GordinK.RennerAnatomic considerations for plate-screw fixation of the cervical spineSpine101991S548S551
- R.AhmedV.C.TraynelisA.H.MenezesFusions at the craniovertebral junctionChilds Nerv Syst2410200812091224
- J.JonssonW.RauschingAnatomical and morphometric studies in posterior cervical spinal screw-plate systemsJ Spinal Disord51994429438