Abstract
Abstract
Introduction
Selective peripheral neurotomies (SPN) are proposed when spasticity is focalized on muscles that are under the control of a single or few peripheral nerves.
Objective
This study was done to evaluate the functional results of SPN of median and ulnar nerves in 10 patients who had spastic hyperflexion of the wrist and fingers.
Methods
All patients preoperatively had spasticity either G3 or G4 as measured by modified Ashworth scale. All cases underwent surgery in the form of variable combination of SPN of median and ulnar nerves depending on the pattern and distribution of spasticity. Depending on the degree of preoperative spasticity, 50–80% of the isolated motor branches of fascicles were resected under the operating microscope. Mean postoperative follow up examination period was 21 months.
Results
There was no operative mortality. One patient had wound infection. Transient paresis of flexors of the wrist and fingers because of excessive nerves sectioning occurred in one patient that responded well to physiotherapy. Postoperatively, all the patients had immediate improvement of their spasticity grade. After initial improvement, recurrence of spasticity occurred in one patient 6 months postoperatively and that might be due to insufficient amount of nerve sectioning. Abnormal hand posture that was present in all cases improved in 9 patients (90%) postoperatively, while pain that was present in 50% of cases improved in all these cases postoperatively as measured by visual analogue scale. Assessment of outcome after surgery was done by comparing modified Ashworth scale preoperatively and postoperatively. At the last follow up examination period, excellent results were obtained in 40% of patients, good results in 40% of patients, fair results in 10% of patients, and poor results in 10% of cases. Conclusion: In well-selected patients, SPN can yield good effects on refractory spasticity of the hand and its consequences.
1 Introduction
Selective peripheral neurotomies (SPN) were first introduced for the treatment of spastic deformities of the foot by Stoffel.Citation1 Selectivity is required to suppress the spasticity without excessive weakening of motor power and without producing exaggerated amyotrophy.Citation2 To achieve this goal at least one fifth of the motor fibers are preserved. Selective fascicular neurotomies can be performed in the median and ulnar nerves for spastic hyperflexion of the wrist and fingers.Citation1,Citation3 A temporary local anesthetic block with xylocaine can be useful. Such test can determine if articular limitation results from spasticity or musculotendinous contractures and/or articular ankylosis.Citation4
Selective peripheral neurotomies are proposed when spasticity is focalized on muscles that are under the control of a single or few peripheral nerves.Citation5 Careful selection of patients is crucial to obtain worthwhile outcomes. SPN aims at re-equilibrating the tonic balance between agonist and antagonist muscles by reducing excess spasticity.Citation6 The surgical procedure therefore must be as selective as possible; that is, it must not abolish useful muscular tone and must not decrease residual motor and sensory functions.Citation7 Reduction of spasticity is obtained by sectioning both afferents and efferents fibers of the stretch-reflex at the level of the muscular nerve.Citation8 Selectivity of the lesion is assured when using fine microsurgical dissection and accurate localization of motor nerves with intraoperative electrical nerve stimulation.Citation9
The aim of this work was to evaluate the functional results of selective peripheral neurotomies of median and ulnar nerves in 10 patients who had spastic hyperflexion of the wrist and fingers. Also to compare these results with the results of the other authors reported in the literature.
Methods
This retrospective study was carried out on 10 patients who had spastic hyperflexion of the wrist and fingers. This study was done in Alexandria hospitals over a period of 4 years starting from January 2006 to December 2009. The male to female ratio was 1 to 1 (5 males and 5 females) and their ages ranged from 15 to 58 years with mean age of 34 years.
Selection and assessment of patients were performed carefully that included observation of posture, assessment of passive range of motion, orthopedic status (musculoskeletal contractures), and quantification of the degree of spasticity using modified Ashworth scale. In this study all patients preoperatively had spasticity either G3 or G4 as measured by modified Ashworth scale (). The determination of the respective involvement in the abnormal posture of spasticity (treated with SPN) and only articular, muscular, tendinous, and/or ligamentous limitations (relieved by orthopedic procedures) was important. If doubt persisted after detailed clinical examination, nerve blocks with 3 mL of 0.25% xylocaine were used for testing of passive articular mobility. When spasticity plays the larger role in the articular limitations, abnormal postures were significantly diminished after the test. If this was not the case, orthopedic surgery may be the initial or the only treatment. Also functional outcome was assessed using Oswestry scale of spasticity grading ().
Table 1 Modified Ashworth scale.
Table 2 Functional outcome of 10 patients who underwent SPN using Oswestry scale.Citation6
All cases underwent surgery in the form of selective peripheral neurotomies of median and ulnar nerves under general anesthesia but without long-lasting muscle relaxants so that the motor responses elicited by bipolar electrical stimulation of motor branches could be detected to identify the motor nerve.
The skin incision began 3 cm above the flexion line of the elbow, medial to the biceps brachii tendon; both median and ulnar nerves were exposed with the same incision.
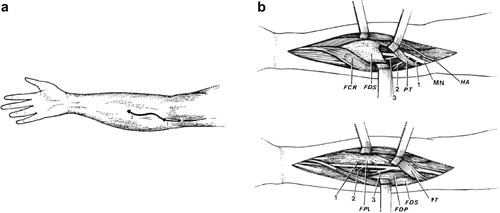
The identification of motor branches of pronator teres (PT), flexor carpi radialis (FCR) and to the flexor digitorum superficialis (FDS) was done. The muscular branches of flexor digitorum profondus (FDP), the flexor pollicis longus (FPL) and the pronator quadratus (PQ) might be individualized as separate branches or remain together in the distal trunk of the anterior inter-osseous nerve. The ulnar nerve was identified medially to the medial epicondyle, where it enters between the two heads of the flexor carpi ulnaris. There, the two motor branches to the flexor carpi ulnaris (FCU) muscle were identified. More distally, the branches to the medial half of the FDP were found. () This was an essential step to avoid sensory impairment and usually requires the use of the operating microscope and intra-operative nerve stimulation at low intensity (1 mA) to avoid electrical diffusion and an incorrect interpretation.
Depending on the degree of preoperative spasticity, 50–80% of the isolated motor branches of fascicles were resected under the operating microscope. The resection was 5 mm long from the proximal stump, which was coagulated with bipolar forceps to prevent re-growth of fibers. When there were several nerve branches for one muscle, one or more branches could easily be sectioned completely until the global amount needed for the considered muscle was attained.
The evaluation of treatment outcome was done by measuring some of the clinical consequence of spasticity like pain, abnormal posture and reduced functional ability. Mean postoperative follow up examination period was 21 months (range from 1 to 3, 5 years).
2 Results
SPN was performed on both ulnar and median nerves in all cases at the same setting using the same incision. All patients were followed up after surgery, at the discharge from the hospital then at 3 months postoperatively. The last postoperative follow-up examination period was from 1 to 3, 5 years.
Postoperative mortality and morbidity: There was no perioperative mortality. As regard the morbidity, one patient had wound infection that responded well to antibiotics after culture and sensitivity. Paresis of flexors of the wrist and fingers because of excessive nerves sectioning occurred in one patient that was transient, and responded well to physical therapy. Recurrence of spasticity due to insufficient amount of sectioning could be observed in one case (10%) that was shifted to other modalities of treatment (Botulinum toxin injection). Recurrence occurred 6 months postoperatively after initial improvement of the spasticity.
Assessment of outcome after surgery was done by comparing modified Ashworth scale preoperatively and postoperatively. The patients were classified into four groups according to their results. Group 1: Reduction of three or more grades was considered excellent, group 2: reduction of two grades was considered good, group 3: reduction of one grade was considered faire and group 4: no grade reduction was considered poor. All patients had immediate initial improvement of their spasticity.
At the last follow up examination period, excellent results were obtained in 40% of patients, good results in 40% of patients, fair results in 10% of patients, and poor results in 10% of cases.
In excellent and good results, the reduction of spasticity was accompanied by complete withdrawal of medications.
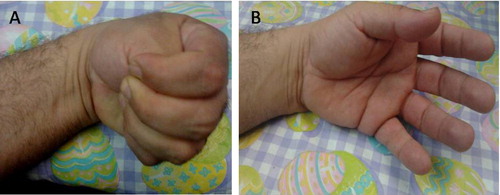
Abnormal hand posture that was present in all cases improved in 9 patients (90%) postoperatively, while pain that was present in 50% of cases improved in all these cases as measured by visual analogue scale ( and ). Summary data and outcome of these 10 patients are listed in .
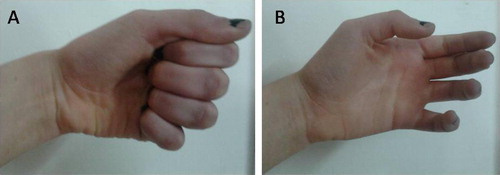
Table 3 Summary data and outcome of 10 patients who underwent SPN of median and ulnar nerves.
Also, performance and functional outcome of these 10 patients was assessed by comparing both preoperative and postoperative Oswestry scaleCitation6 as shown in .
3 Discussion
Hypertonia of the upper limb due to spasticity causes pronation of the forearm and flexion of wrist and fingers resulting in reduction, or even loss of neuro-functional capacities.Citation10 Treatments of hypertonia of spastic origin are various and thus necessitate multidisciplinary management. Along with medication and reeducation, injections of botulinum toxin and selective neurotomies are two therapeutic options frequently chosen.Citation11 Selective fascicular neurotomy is appropriate in cases of localized spasticity, with absence of associated muscle-tendon retraction, and when a motor block using anesthetic or first test using botulinum toxin has given good functional results.Citation12 In the literature, fascicular neurotomy has essentially been used for the treatment of spastic drop foot.Citation13,Citation14 Few precise studies have been undertaken to propose these techniques for the ventral compartment of the forearm.Citation15,Citation16
Generally patients do not complain about spasticity; they are more likely to be aware of stiffness, deformity and limitations in functional abilities. After a period of time, the patients will have a mixture of spasticity and muscle shortening or contracture. There are two types of hand deformities, dynamic caused by spasticity and fixed described as contracture that remains present under local blocks or anesthesia. The differentiation between dynamic from fixed deformities is of prime importance before deciding any surgical treatment. The dynamic range of motion measures are useful starting points, supplemented with instrumental measures of spasticity and its effects on function, such as motion. Spasticity should only be treated when excess muscular tone leads to further functional losses, impairs locomotion, or induces deformities, or chronic pain.Citation17 This should be explained carefully to patients what can be gained and what will not be obtained by surgery.Citation18 The strategy of using pre-operative injection tests for motor block, allows the patient to appreciate the benefit that can follow a selective neurotomy. Objectives may be cosmetic.Citation19
In this study, the most common cause of spastic hand was cerebrovascular stroke that was found in 5 patients (50%). Also, cerebral palsy was the cause in two cases, cervical cord injury in two cases and traumatic brain injury in one case. In this study, the male to female ratio was 1 to 1 (5 males and 5 females) and their ages ranged from 15 to 58 years with mean age of 34 years. Cerebral palsy occurred in young age while cerebrovascular stoke in old age and both of them had equal sex distribution.
Assessment of the degree of spasticity in each muscle (or group of muscles) of the upper limb is essential to plan the surgical procedure. Spasticity of the pronators and flexors of the wrist and fingers mediated by the median and ulnar nerves. Thus, a variable combination of SPN can be performed, depending on the pattern and distribution of spasticity. The operative program includes designation of the spastic muscles to be targeted and the amount of denervation of the respective muscles needed.Citation1,Citation5 For measuring the spasticity, Ashworth developed a standardized scale to document resistance to passive movements ().Citation20 It is a simple, easy to use test. The scale has been shown to correlate with other more reliable measures such as electromyography measurements. The disadvantage of this scale is the fact that it measured the combined effect of both biochemical and neural components of tone also the lake of standardization technique in performing the tone measurements. Repetitive movement of the limb may modify stretch reflex and influence more dynamic biochemical properties of the muscle. The force applied in moving the limb should also be standardized.Citation21 Also, preoperative assessment of the patients by measuring functional disability related to their spasticity was done using Oswestry scale of Spasticity (). This scale is based on the common assumption that spasticity interferes with the quality of movement. Although other positive features of UMN syndrome may interfere with function, it is the negative features which are the most disabling. Thus, functional impairment in the UMN syndrome is multifactorial and so functional measures should not be portrayed as measurement of spasticity. In practice the scale is sensitive to change in the acute setting but has not been subjected to formal validity or reliability studies.Citation6,Citation21
Surgery should be performed so that excessive hypertonia is reduced without the suppression of useful muscular tone or impairment of residual motor and sensory functions.Citation1 SPN aims at re-equilibrating the tonic balance between agonist and antagonist muscles by reducing excess spasticity. Decreased spasticity is obtained by sectioning both afferents and efferent fibres of the stretch–reflex at the level of a motor nerve.Citation5
The microsurgical selective neurotomies concerning the motor branches originating from the median nerve and ulnar nerve can be performed by one surgical approach alone since all of them originate in a short interval located between 0,5 to 13,5 cm from the horizontal line drawn through the top of the medial epicondyle. This surgical approach must be S-shaped, with a transversal incision in the cubital fossa to avoid scar adhesion here, with a short proximal curve at the bicipital medial groove and a longer distal curve following the medial edge of the brachioradialis.Citation22
The median nerve and its collateral branches can be isolated above the PT. It then enters distally between the humeral head and the ulnar head of this muscle. This usual arrangement was found in all cases in this study, thus making it easy to dissociate the two muscle heads to expose the median nerve. The dividing level between the humeral head of the PT and the FCR is determined. After spreading open the muscle bundles, the median nerve can be seen vertically descending through this space before running under the FDS arcade. Variations are rare.Citation23
According to Von Lanz and WachsmuthCitation24 the median perforates the humeral head in 2% of cases and in 3%, it runs behind the two heads. It is important to keep these particular arrangements in mind, as surgical dissection could need to be modified.Citation23
Many authors reported their results concerning extra-muscular nerve supply in the front of forearm.Citation24,Citation25 The PT is classically described as having extra-muscular nerve supply made by 2 branches from the median nerve. This is also what was found in 90% of the cases of this study.
Likewise, extra-muscular nerve supply of the FDS made by two or three branches at regular intervals is just as Brash described.Citation26 This organization of the nerves at regular intervals as well as the existence of two muscle heads probably explains the often unpredictable therapeutic results of injections of botulinum toxin into this muscle.Citation27,Citation28
For the ulnar nerve, it is possible to follow its course starting behind the medial epicondyle and continuing vertically, under the FCU arcade which can, at this level, be opened.
From the ulnar nerve, two branches, one proximal and one distal, are usually described for the FCU and one branch for the FDP. This is also what was found in all operated cases. The two branches for FCU originate in this study at 2.o cm and at 2.5 cm on average respectively from the horizontal line drawn through the medial epicondyle.Citation29 The branch supplying the FDP is located at 4.3 cm on average from the horizontal line drawn through the top of the medial epicondyle and it divides into two.Citation22 This is also what was found in all the cases of this study.
This precise knowledge of the distribution of the median and ulnar nerves below the elbow makes selective fascicular neurotomies possible beyond the nerve trunk, by selecting collateral motor branches.Citation15 After identifying them by electrical stimulation, the neurotomy is performed under microscope. Each motor branch is partially sectioned (between 50% and 80%). The percentage of fibers to be sectioned depends on the degree of spasticity, and on the response to intraoperative electrical stimulation after sectioning 50% of the fibers.Citation26
In the literature, few studies describe these selective neurotomies below the elbow. Decq et al.Citation30 have described selective neurotomy microsurgical techniques for the upper limb, but they only concern the pectoralis major and teres major. More recently, Bouttens and DelecourtCitation31 refer to neurotomy surgical techniques for the upper limb but give no practical details. BrunelliCitation32 perfectly describes this surgical approach at the cubital fossa, but extends it to the PQ or to the palm of the hand to denervate the intrinsic muscles. In this study denervation of the ulnar nerve was extended to the palm to denervate adductor pollicis in one case with thumb in palm deformity. Canovas et al.Citation33 have done a precise biometrical study of the collateral branches of the median nerve of the elbow. Segal et al.Citation34 have done partial morphological studies of some muscles in the ventral compartment of the forearm.
In this study the spasticity and abnormal hand posture had improved in 90% of cases, as measured by Ashworth scale and also by improvement in the functional score. Most patients in this study (90%) had more comfort, less pain and ability to resume physical therapy with more functional gain. The same results were reported by Sindou et al.Citation2 who performed SPN of median and ulnar nerves in 25 patients with spastic hand. The muscular tone was diminished after SPN due to interruption of the afferent component of the both afferents and efferent fibres of the stretch–reflex at the level of a motor nerve. Recurrence of spasticity occurred in one patient after initial improvement because of insufficient amount of sectioning and was treated by botulinum toxin injections and physiotherapy. The recurrence could be explained by the fact that the nerve endings of intact α motor neurons sprout in an attempt to compensate for the partial denervation as regrowth has been prevented by the resection performed during neurotomy. New motor endplates appear, and the size of motor units increases in proportion to the degree of denervation.Citation3 On average, motor units increase by about five times their original size, allowing them to compensate for a loss of as much as 80% of the motoneuron pool.Citation8
The outcome of SPN also intimately depends on the postoperative care after a successful surgery. The hand can be raised to avoid edema and mobilized as soon a possible, physical therapy beginning on the second post-operative day. An anti-thrombotic therapy is administered for 5 days after surgery, and the patient is discharged on the seventh postoperative day. Immediately thereafter, a programme of physical and occupational therapy is undertaken for at least 6 weeks.Citation15
4 Conclusion
In well-selected patients, SPN can yield good effects on refractory spasticity of the hand and its consequences. SPN can unmask residual motor function of muscles, make easier passive movements, increase comfort in daily activity, decrease pain because of spasticity and improve cosmetic appearance of the hand. Operative planning with a detailed clinical assessment of each spastic muscle is essential to determine the degree of nerve section, thus avoiding insufficient surgery or the loss of motor strength in the concerned muscles. Neurotomy performed distally on the muscular branches warrants selectivity of the procedure, to avoid sensitive and painful complications.
Notes
Available online 20 August 2011
Peer review under responsibility of Alexandria University Faculty of Medicine
References
- A.StoffelThe treatment of spastic contracturesAm J Orthop Surg101912611644
- M.SindouF.SimonP.MertensSelective peripheral neurotomy (SPN) for spasticity in childhoodChilds Nerv Syst232007957970
- P.MertensM.SindouSelective peripheral neurotomies for the treatment of spasticityM.SindouR.AbbottY.KeravelNeurosurgery for Spasticity: A Multidisciplinary Approach1991SpringerNew York pp. 119-132.
- G.LagallaM.DanniF.ReiterPost stroke spasticity managementAm J Phys Med Rehab792000377384
- I.HodgkinsonM.SindouDecision making for treatment of disabling spasticity in children in “Neurosurgical Management of Disabling Spasticity” (Sindou ed.)Oper Tech Neurosurg72004120123
- P.MertensM.SindouSurgical management of spasticityM.P.BarnesG.R.JohnsonClinical Management of Spasticity2001Cambridge University PressCambridge UK pp. 239-65.
- P.DecqE.CunyP.FilipettiPeripheral neurotomy in the treatment of spasticity Indications, techniques and results in the lower limbsNeurochirurgie441998175182
- R.DenglerA.KonstanzerS.HesseCollateral nerve sprouting and twitch forces of single motor units in conditions with partial denervation in manNeurosci Lett971989118122
- P.DecqP.FilipettiA.CubillosSoleus neurotomy for treatment of the spastic equinus foot Groupe d’Evaluation et de Traitement de la Spasticite et de la DystonieNeurosurgery47200011541160
- N.J.O’ DwyerL.AdaP.D.NeilsonSpasticity and muscle contracture following strokeBrain1195199617371749
- G.TardieuSpasticity: an ill-defined condition abstract retrospective neurology in the central and peripheral nervousVenice World Federation Neurol119832426
- T.TairaT.HoriSelective peripheral neurotomy for spasticity in cerebral palsyNo Shinkei Geka2912200111371150
- C.BerardM.SindouJ.BerardSelective neurotomy of the tibial nerve in the spastic hemiplegic child: an explanation of the recurrenceJ Pediatr Orthop B719986670
- T.DeltombeT.GustinP.LalouxSelective fasicular neurotomy for spastic equinovarus foot deformity in cerebral palsy childrenActa Orthop Belg67200115
- J.MaarrawiP.MertensM.SindouSurgery in the Peripheral Nerves for Upper Limb SpasticityOper Tech Neurosurg72005147152
- A.K.MsaddiA.R.MazroueS.ShahwanMicrosurgical selective peripheral neurotomy in the treatment of spasticity in cerebral palsy childrenStereotact Funct Neurosurg691997251258
- P.DecqP.FilipettiA.FevePeripheral selective neurotomy of the brachial plexus collateral branches for treatment of the spastic shoulder: anatomical study and clinical results in five patientsJ Neurosurg861997648653
- D.E.GarlandR.ThompsonR.L.WatersMusculocutaneous neurotomy for spastic elbow in flexion in non-functional upper extremities in adultsJ Bone Joint Surg (Am)621981108112
- A.K.PurohitB.S.V.RajuK.Shiv KumarSelective musculocutaneous fasciculotomy for spastic elbow in cerebral palsy: a preliminary studyActa Neurochir (Wien)1401998473478
- F.PisanoG.MiscioC.C.DelQuantitative measures of spasticity in post stroke patientsClin Neurophysiol1116200010151022
- A.D.PandyanG.R.JohnsonC.L.PriceA review of the properties and limitations of the Ashworth and modified Ashworth scales as a measure of spasticityClinc Rehab1351999373383
- D.LepageB.ParratteL.TatuExtra- and intramuscular nerve supply of the muscles of the anterior antebrachial compartment: applications for selective neurotomy and for botulinum toxin injectionSurg Radiol Anat272005420430
- S.F.GuntherD.DiPasqualeR.MartinThe internal anatomy of the median nerve in the region of the elbowJ Hand Surg (Am)171992648656
- Lanz T V, Wachsmuth W P. Anatomie. Arm. Springer; Berlin-Gottingen-Heidelberg 1959; 144.
- C.GrosP.FrerebeauL.BenezechSelective radicular neurotomyL.SimonActualities in functional physical therapy1977MassonParis pp. 230-235
- Brash JC. Neuro-vascular hila of limb muscles. E&S Livingstone, Edinburgh 1955; 100.
- C.F.O’BrienInjection techniques for botulinum toxin using electromyography and electrical stimulationMuscle Nerve61997176180
- M.RousseauxO.KozlowskiJ.FrogerEfficacy of botulinum toxin A in upper limb function of hemiplegic patientsJ Neurol24920027684
- A.Y.LimV.P.KumarJ.HuaThe neuromuscular of the flexor carpi ulnarisPlast Reconstr Surg103199910461051
- P.DecqPeripheral neurotomies for the treatment of focal spasticity of the limbsNeurochirurgie492003293305
- D.BouttensC.DelecourtLes traitements orthope‘diques des conse´quences de la spasticite´ au membre supe´ rieurNeurochirurgie492003353357
- G.BrunelliF.BrunelliPartial selective denervation in spastic palsies (hyponeurotization)Microsurgery41983221224
- F.CanovasP.MouilleronF.BonnelBiometry of the muscular branches of the median nerve to the forearmClin Anat111998239245
- R.L.SegalP.A.CatlinE.W.KraussAnatomical partitioning of three human forearm musclesCells Tissues Organs1702002183197