Abstract
Introduction
Lumbo-sacral spinal stenosis (LSS) is a frequent cause for chronic low back pain. The diagnosis is primarily radiological. Neural insult is not frequent in every case. Although the degree and type of LSS can exactly be described with the current imaging studies, the extent of neural impairment cannot be expressed by radiological means. Electrophysiological investigations have an important role in determining the extent of neural compromise. The aim of this study was to evaluate the validity of mixed and dermatomal somatosensory-evoked potentials (SEPs) for the diagnosis of neurological compromise in LSS.
Subjects
Twenty-two patients (11 men and 11 women) with CT and/or MRI-based confirmation of LSS were enrolled. All patients went through thorough neurological and electrophysiological examination. Twenty healthy individuals matching to patients for age and sex were enrolled in the electrophysiologic tests as a control group.
Results
Classic neurogenic claudication was encountered in 86.4% of cases (19 patients). Examination revealed neurologic deficits in six patients (27.3%). MRI evidence of nerve root compression was found in only 12 patients (54.5%). The incidence of electrophysiological abnormality was the highest using dermatomal SEP (90.9%) followed by mixed SEP of the posterior tibial nerve (81.8 %), H-reflex comes next (59.1%), and finally F-wave, which showed the lowest incidence (18.2%). The correlation analysis between different electrophysiologic items and the patient's complaint of neurogenic claudication was best with dermatomal SEP (77.3%), followed by mixed SEP (68.2%) with a significant fair agreement.
Conclusion
Dermatomal and mixed SEPs had added to the clinical and radiological assessment of patients with LSS providing evidence for root dysfunction. Their inclusion in routine evaluation of those patients would help detection of functional integrity of the neural structures.
Abbreviations:
- AP
- anteroposterior
- CMAP
- compound muscle action potential
- CT
- computed tomography
- DSEP
- dermatomal somatosensory-evoked potential
- LSS
- lumbosacral spinal canal stenosis
- MRI
- magnetic resonance imaging
- NC
- neurogenic claudication
- NCV
- nerve conduction velocity
- PTN
- posterior tibial nerve
- SEP-PTN
- somatosensory-evoked potential of posterior tibial nerve
- SEPs
- somatosensory-evoked potentials
1 Introduction
The syndrome of lumbosacral spinal canal stenosis (LSS) was not widely diagnosed until Verbiest's clinical description in 1954.Citation1 The cardinal symptom of LSS is neurogenic claudication (NC), defined as diffuse buttock and leg pain, paresthesias and cramping of one or both lower extremities induced by walking and relieved by sitting or forward bending.Citation2 Walking ability can become substantially limited because of NC. The condition may not be diagnosed until irreversible neurologic damage has occurred.Citation3 In patients with symptoms of stenosis, magnetic resonance imaging (MRI) or computed tomography (CT) with contrast should be used to localize the site of nerve root entrapment.Citation4 In most of the patients, early diagnosis and treatment of spinal stenosis may prevent intractable pain and permanent neurologic sequelae of chronic nerve root entrapment.Citation5
Although the extent and type of the spinal canal stenosis can exactly be described with the current imaging studies, the extent of neural impairment and its functional defects cannot be expressed by radiological means.Citation3 In cases with typical NC symptoms and unequivocal imaging findings the diagnosis is straightforward. However, not all patients are present with typical symptoms and there is obviously no correlation between the severity of stenosis detected by imaging and clinical complaint. Recent MRI studies have shown that mild to moderate stenosis can also be found in asymptomatic individuals.Citation6
Electrophysiological techniques are useful in evaluating compressive lumbosacral radiculopathies, providing information complementary to that obtained by imaging procedures. It is hypothesized that electrophysiological recordings, especially somatosensory-evoked potentials (SEPs), indicate a nerve root involvement complementary to the neurological examination. They provide confirmatory information in less obvious clinical conditions and help in exclusion of other abnormalities.Citation7
The aim of this study was to evaluate the role of mixed and dermatomal somatosensory-evoked potentials as an add-on diagnostic procedure to imaging studies in patients with LSS.
2 Subjects
Twenty-two patients with clinically suspected and radiologically confirmed LSS were randomly collected among those attending at the Outpatient Clinic of Physical Medicine, Rheumatology and Rehabilitation Department, Faculty of Medicine, University of Alexandria. Clinical diagnosis was based on chronic back and/or leg pain for more than three months with or without NC. Lumbar canal stenosis was diagnosed radiologically by CT and/or MRI according to one or more of the following findingsCitation8:
| • | Trefoil appearance of the spinal canal at axial images. | ||||
| • | Anteroposterior (AP) diameter of the midsagittal spinal canal at the most stenotic level ⩽12 mm at sagittal images describing central spinal stenosis. | ||||
| • | The lateral recess measurements with a diameter ⩽5 mm describing lateral recess stenosis. | ||||
Patients were excluded if clinical, radiological and/or electrophysiological evaluations revealed signs of: lumbosacral plexopathy, peripheral neuropathy associated with any systemic disease, neuromuscular disorder, spinal tumors, post traumatic or surgical stenosis or spondylolithesis.
A control group of 20 healthy subjects free from any musculoskeletal or neurological deficits were also included for the determination of the normal electrophysiological values.
2.1 Methods
All patients were subjected to: (1) thorough history taking focusing on the presence or absence of NC, (2) full neurological examination of both lower limbs, (3) electrophysiological studies including sural sensory conduction study, posterior tibial nerve (PTN) motor conduction study, peroneal motor conduction study, PTN F-response, gastrocnemius-soleus H-reflex,Citation9 mixed SEP-PTN and dermatomal SEP (DSEP) of L3, L4, L5 and S1.Citation10 For the mixed SEP-PTN examination, right and left PTN were stimulated just behind the medial malleolus, with an intensity to create a slight twitch in the toes. Recordings were made from Cź and referred to Fz according to the international 10–20 system. P37/N45 response was statistically evaluated. For DSEP examinations, stimulating electrodes were placed on the inner side of the femur 4 cm above the knee for the L3 dermatome; in the medial leg in the region where the saphenous nerve ranges superficially for the L4 dermatome; in the foot between the first and second toes for the L5 dermatome; and lateral malleolus for the S1 dermatome. Evocation intensity was set at a level where the individual would easily perceive the evocation, but would not sense pain or would not twitch. Cortical responses were obtained from Cź and referred to Fz according to the international 10–20 system. SEP responses were recorded at 1.25–2.5 μV sensitivity, 100 ms sweep speed, and 10 Hz–2 kHz filtration range. The average of 200 cortical responses was taken twice. The responses were statistically evaluated. In SEP-PTN and DSEP examinations, a latency value above the cut-off point obtained from the control group and/or an amplitude value below the cut-off point obtained from the control group were evaluated as pathological.
CT and/or MRI imaging of the lumbosacral spine were performed for all patients. MRI was performed in 14 patients (64%), CT scans were performed in four patients (18%), and both were done in four patients (18%). All the axial and sagittal T2 weighted images in MRI and the axial images in CT scans were used to determine the AP diameter of the spinal canal at the most stenotic level at the midline describing central spinal stenosis and at the lateral recess describing lateral recess stenosis.Citation11 Mild central LSS is diagnosed if the AP diameter of the most stenotic level ⩽12 mm and >11 mm, moderate if ⩽11 mm and >8 mm and severe if ⩽8 mm. Also the cause and levels of stenosis were determined.
Data were analyzed using the Statistical Package for Social Sciences (SPSS ver. 17, Chicago, IL, USA).
3 Results
Twenty-two patients (50% men and 50% women) were enrolled in this study. Their mean age was 49.5 years (ranged from 23 to 73 years). The control group consisted of 20 individuals, eight men (40%) and 12 women (60%). Their mean age was 45.7 years (ranged from 24 to 70 years). There were no statistically significant differences between patients and control group as regards the sex (χ2 = 0.305, p = 0.581) and age (t = 1.904, p = 0.066).
Nineteen patients (86.5%) suffered from back/buttock and leg pain, while only one patient (4.5%) had only back pain and two patients (9%) had only leg pain. Sixty-four percent of patients experienced chronic pain for more than 6 months. Pain was typically aggravated by lumbar extension and relieved by lumbar flexion. Nineteen patients (86.5%) presented with typical NC manifested as intermittent crampy diffuse radiating thigh or leg pain with associated paresthesia during walking relieved by sitting, squatting and lumbar flexion. None of the patients experienced motor weakness or sphincteric disturbance.
3.1 Examination
Ninety-one percent of the patients walked with forward flexed attitude. Clinical examination revealed decreased lumbar lordosis in 19 patients (86.5%). Straight leg raising test was positive on one side in three patients (13.5%) and bilaterally in one patient. Motor deficit was present in two patients (9%) with weak left tibialis anterior and extensor hallucis longus muscles (G3). Muscle tone and coordination were normal in all patients.
Only three patients (13.5%) had sensory deficit manifested as hypoesthesia along the left L5 dermatome in one patient, along the left L5 and S1 dermatomes in another patient and along the right L3, L4, L5 and left S1 dermatomes in the third. Deep sensations were normal in all patients.
As regards the deep and superficial reflexes; ankle reflex was depressed on one side in four patients (18%) and bilateral in two patients (9%). Knee reflex was depressed on one side in one patient (4.5%). Plantar reflex was normal in all patients. Thus at the clinical level six patients were suspected to have radiculopathy.
3.2 Radiological findings
Severe central LSS was diagnosed in one patient (4.5%), moderate stenosis in 18 patients (82%) and mild stenosis in three patients (13.5%). Lateral recess stenosis was found in seven patients (32%). Its measurement ranged from 3 to 5 mm. The most frequently stenotic level was L4/5 in 15 patients (68.5%) followed by L3/4 in four patients (18%). The mean mid-AP diameter at its most stenotic level was 10.3 mm (ranged from 8 to 12 mm). Nineteen patients (86.5%) had more than one stenotic segment.
Primary LSS was diagnosed in three patients due to short pedicles in one patient and congenitally small canal in two patients, whereas secondary LSS was diagnosed in 19 patients due to combination of hypertrophied ligamentum flavum (five patients), apophyseal arthrosis (seven patients), disk bulge or herniation (12 patients), and spondylodegenerative changes (13 patients).
In 54.5% of patients (12 patients) a significant nerve root compression at its exit foramina was found in 1, 2 or 3 segments. S1 root was most frequently affected by compression (six patients). Unilateral compression was found in 10 patients and bilateral in two patients (L5 root in one patient and S1 root in the other).
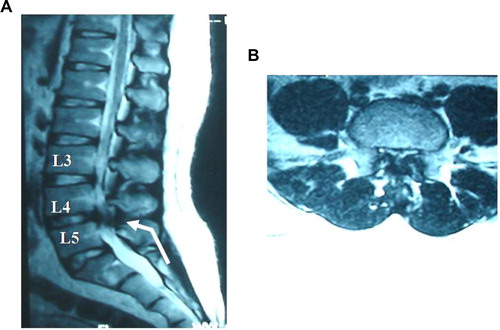
shows sagittal T2 weighted MRI of the lumbosacral spine in one of the studied patients with LSS with the evidence of nerve root compromise.
Figure 1 (A) Sagittal T2 weighted MRI of lumbosacral spine showing decreased normal lumbar lordosis, stenotic bony canal (AP diameter = 8.5 mm at L3/4 and L4/5 levels), diffuse posterior disk bulge at L4/5 together with thickened ligamentum flavum posteriorly (arrow). (B) Axial T2 weighted image at L4/5 level showing diffuse posterior disk bulge slightly inclined to the right side encroaching upon the ipsilateral exiting and traversing nerve roots, exaggerated by bony canal stenosis.
3.3 Electrophysiological recordings
The evaluation of the electrophysiological recordings is based on reference values obtained from the control group. Values exceeding the cut-off points (Youden Index) were considered abnormal.
3.3.1 Nerve conduction studies
| • | Sensory conduction study of the sural nerve: None of the patients demonstrated any abnormalities regarding sensory conduction study of the sural nerve which excludes the presence of polyneuropathy. | ||||
| • | Motor conduction study of the PTN and peroneal nerve: Reduced compound muscle action potential (CMAP) amplitude of PTN was found in 40.5% of patients. Eighteen percent of patients had mild slowing of motor nerve conduction velocity (NCV) (unilateral in three patients, bilateral in one patient) indicating axonal degeneration. Reduced CMAP amplitude of the peroneal nerve was found in 31.5% of patients. Thirteen percent of patients had mild slowing of motor NCV (unilateral in two patients, bilateral in one) indicating axonal degeneration. | ||||
3.3.2 Late responses
| • | F-response: Eighteen percent of patients (four patients) had bilaterally delayed response as compared to age and height matched control values. There was a statistically significant difference between both groups as regards the F-wave minimal latency. | ||||
| • | H-reflex: Prolonged H-reflex latency was found in 59% of patients (13 patients) as compared to age and height matched control values. In 50% of these patients, the H-reflex was bilaterally delayed. There was a statistically significant difference between both groups as regards the H-reflex latency. | ||||
3.3.3 Somatosensory-evoked potentials
There was a statistically significant difference between patients and controls as regards the latency and amplitude of SEP-PTN and DSEP ( and ). Mixed SEP-PTN abnormalities were detected in 18 patients, whereas DSEP abnormalities at one or more levels were detected in 20 patients (). Abnormal DSEPs were found in four out of six patients with clinically suspected radiculopathy and in 16 patients without clinical evidence of radiculopathy. shows mixed SEP-PTN and DSEP of L3, L4, L5 and S1 recordings in a patient with LSS with evidence of MRD consistent with LSS.
Figure 2 Mixed SEP-PTN and DSEP of L3, L4, L5 and S1 traces of a patient with LSS. Mixed SEP showing normal latency and amplitude on right side stimulation but prolonged latency and low amplitude on left side. At the L3 level, wave forms are absent on the right side but of normal P1 latency and low amplitude on the left side. At the L4 level, normal P1 latency on the right side and prolonged on the left side with low amplitude bilaterally. At the L5 level, the wave forms are absent bilaterally. At the S1 level, also markedly prolonged and attenuated response bilaterally. (R.) right side recording, (L.): left side recording.
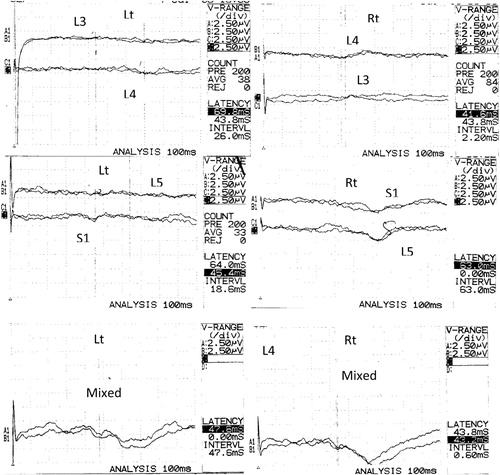
Table 1 The P37 latency of mixed SEP-PTN and DSEPs of L3, L4, L5 and S1 in patient and control groups.
Table 2 The amplitude of mixed SEP-PTN and DSEPs of L3, L4, L5 and S1 in patient and control groups.
Table 3 Frequency of electrophysiological abnormalities in the studied patients.
3.3.4 Frequency of different electrophysiological abnormalities in the studied patients
The frequency of electrophysiological abnormalities is shown in . It was found that the incidence of abnormality among the patients was highest using the DSEPs study (20 patients; 91%) followed by the mixed SEP-PTN (18 patients; 82%). H-reflex came next (13 patients; 59%) and finally F-wave which showed the lowest incidence (four patients or 18%).
3.3.5 Correlation analysis between NC and SEPs
Fifteen out of the 19 patients with NC had mixed SEP-PTN abnormality with a significant fair concordance (κ = 0.26, p = 0.034) and 68% agreement. Whereas, 17 out of the 19 patients with NC had DSEPs abnormalities with a significant fair concordance (κ = 0.31, p = 0.031) and 77.2% agreement.
3.3.6 Correlation analysis between SEP and the radiological findings
Mixed SEP-PTN was fairly correlated with imaging with an agreement of 72.7%. DSEPs also showed an agreement of 50%, 68.2%, 63.6% and 63.6% at L3, L4, L5 and S1, respectively, but all were not statistically significant.
3.3.7 Sensitivity and specificity of DSEP and mixed SEP-PTN
Considering NC as a comparative standard, the sensitivity and specificity were estimated for DSEP and mixed SEP-PTN. The sensitivity and specificity of DSEP were 91% and 66.7%, respectively, and was higher than that of the mixed SEP of PTN which were 84.2% and 33.3%, respectively.
4 Discussion
This study included 22 patients with LSS. The role of mixed and dermatomal somatosensory-evoked potentials as an add-on diagnostic procedure to imaging studies was evaluated in those patients.
Clinical examination revealed decreased lumbar lordosis in 19 patients (86.5%). Other studies suggested that diminished lumbar extension constitutes the most significant finding in LSS. Patients with LSS tend to walk with a stooped forward gait and even maintain this posture while standing.Citation12 Their pain is exacerbated with lumbar extension as the cross-sectional area of the spinal canal is reduced as the lumbar spine moves from flexion to extension.Citation13 Straight leg raising test was negative in most of the patients (82%). It is reported that this test is generally negative in LSS patients, differentiating it from acute disk herniation.Citation14
Neurological examination revealed abnormalities in only 27% of patients. Depressed ankle reflex was the commonest (27%). Hyposthesia of the legs came next (13.5%), lastly motor weakness was found in 9% of patients. Similar findings were reported by Vranken et al.,Citation12 who found sensory-motor deficits in less than 20% of patients. The paucity of clinical signs seen in this group of patients was consistent with what has been reported by others.Citation15,Citation16 As the neurological findings, even in severe LSS, are mainly non-specific (no characteristic pattern of sensory-motor deficit) the diagnosis of LSS based on the neurological examination is challenging. Also since the nervous system adapts over time and the development of stenosis is slow and gradual, it takes time for sufficient axonal damage to occur and cause signs and symptoms.Citation17
In the current study central LSS was diagnosed in the CT and/or MRI scans of all the patients. There was an accompanying lateral recess stenosis in seven of them. Nineteen patients (86.5%) had more than one stenotic level. The most frequent stenotic level was L4/L5 in 15 patients (68.5%) followed by L3/4 in four patients (18%). Egli et al.Citation7 found multilevel stenosis in 88% of patients and the most frequent stenotic level was also L4/L5 in 72%. Imaging can distinguish mono- and multisegmental stenosis, as well as the severity of the stenosis that, however, is not related to the pain symptoms or clinical signs. Therefore, imaging is of restricted value for diagnosing the clinical relevance of LSS.Citation7
Whereas all cases presented with CT/MRI evidence of stenosis, radiological evidence of neural compromise (root insult) was diagnosed in 54.5% of patients of this study. S1 nerve root was the most frequently affected level shown by imaging studies. Assessment of functional rather than structural neural lesion was achieved by electrophysiological studies.
Reductions of the CMAP amplitude of PTN in 41% of patients and of peroneal nerve in 32% indicate axonal damage. The nerve compression leads to an axonal damage and eventually a Wallerian degeneration of the peripheral nerve. CMAP abnormalities in assessment of radiculopathies are limited by the overlapping root innervation.Citation15
Eighteen percent of patients showed mild slowing of motor NCV of the PTN and 13.5% showed mild slowing of motor NCV of the peroneal nerve. Slowing of motor conduction velocities between proximal and distal stimulation sites is uncommon and, if present, limited in degree due to the overlapping root innervation. Decrease in motor conduction would be restricted to the mild slowing seen with the loss of the largest, fastest conducting motor fibers.Citation15
F-wave showed the lowest incidence of abnormality among the studied electrophysiological parameters (18%). H-reflex showed abnormality in 59%. Egli et al. [Citation7] obtained similar results. They found F-wave abnormalities in 15% of 54 patients scheduled for surgery for LSS and H-reflex abnormalities in 52%. F-wave study may be normal in root disease, as this test evaluates the integrity of only the ventral roots.Citation15 But in demyelinating polyneuropathic disorders F-wave study is of high sensitivity.Citation18 H-reflex evaluates the integrity of both the dorsal and ventral roots but it detects only S1 root dysfunction. Also H-reflex in normal individuals decreases with age so it must be interpreted cautiously in old age groups.Citation19
In this study abnormal mixed SEP-PTN recordings were found in 18 patients (82%). Similar findings were detected by Egli et al.,Citation7 who found mixed SEP-PTN abnormalities in 78% of the studied 54 patients.
Dermatomal SEP abnormalities were found in 91% of the patients at more than two levels so multiple lumbosacral root disease (MRD) criteria were fulfilled. SEPs have to demonstrate an abnormality at more than one level to be considered abnormal; otherwise, it would represent single root disease not MRD, the signature of LSS.Citation20 Similar findings were reported by other studies. In a study by Slimp et al.,Citation21 25 out of 26 patients (96%) with LSS had abnormal DSEPs. In another study by Tokuhashi et al.,Citation22 90% of 34 patients with LSS had abnormal DSEPs. Snowden et al.Citation23 found DSEPs study to be a useful diagnostic test of CT/MRI documented LSS. The insidious, low grade compression of the cauda equina roots occurring in LSS causes impaired proximal nerve conduction best detected by DSEPs study.Citation20 Hall et al.Citation24 utilized mixed SEPs and DSEPs in evaluating 66 patients with LSS. Abnormal recordings were obtained from stimulation of L5 and S1 dermatomes in 62 of them. The P37 latency remained unchanged but the amplitude of the waveform diminished to 50% or less of control. The presence of these abnormal responses was correlated with the surgical result.
It was found in this work that the incidence of electrophysiological abnormalities among the patients is highest using the DSEPs study (91%) followed by the mixed SEPs from the PTN (82%). Moreover, the sensitivity and specificity of DSEPs were 91% and 66.7%, respectively, and were higher than that of the mixed SEP-PTN which were 84.2% and 33.3%, respectively. Similar results were obtained by Snowden et al., Citation25 who evaluated DESPs in 155 patients with spinal stenosis and reported a sensitivity of 93%. Also Dumitru and DreyfussCitation26 attained a sensitivity of 93% for DSEPs in LSS patients. Specificities may be more important than sensitivities since false positive studies could lead to harmful patient management.Citation27 Mixed SEP-PTN showed fewer abnormalities than DSEP as it is dependent on conduction through L4, L5 and S1 nerve roots.Citation24 So it may be normal even if DSEPs are abnormal.
In the current study six patients had radiculopathy at the clinical level. Of them, four were found to have DSEP abnormalities at one or more levels. In 16 patients with no clinical evidence of radiculopathy, SEP abnormalities were evident (subclinical radiculopathy). Those results indicate that SEP abnormalities may be encountered even in the absence of demonstrable sensory deficit and therefore support the idea that SEP studies are more sensitive indicator of spinal nerve root dysfunction than the clinical sensory examination.Citation28
Mixed SEP-PTN and DSEP recordings in a previous study indicated that SEP recordings can confirm NC due to cauda equina involvement.Citation29 In the current study 15 out of the 19 patients with NC had mixed SEP-PTN abnormality and 17 out of the 19 had DSEP abnormalities. Failure to detect abnormalities in some patients may be explained by doing the test in resting condition. These results may be changed if the same tests were done following walking till the symptoms appear as provocative tests. These changes may be reversible as the pathogenesis of NC is thought to be due to relative ischemia of the cauda equina roots during exercise.Citation30,Citation31
Correlation analyses between the different electrophysiologic items and NC revealed that the observed agreement was best with DSEP studies (77.2%) followed by mixed SEP-PTN (68%) with a significant fair agreement.
Mixed SEP-PTN was fairly correlated by imaging with an agreement of 72.7%. DSEPs also showed an agreement of 50%, 68.2%, 63.6% and 63.6% at L3, L4, L5 and S1 levels, respectively, but all were not significant. Fisher et al.Citation32 mentioned that SEP studies correlated well with MRI in the diagnosis of lumbosacral radiculopathy. The contradiction between Fisher's results and our results can be explained by the fact that DSEPs in the current study revealed several bilateral affections whereas imaging revealed bilateral nerve root compression in only two patients. This is in agreement with other authors who found that in large series of patients referred for lumbosacral root assessment, electrophysiologic changes are often bilateral. This is because the lumbosacral roots can be compromised not only at their exit foramina as appears in CT or MRI but also anywhere in the cauda equina within the spinal canal, where the roots are quite compact.
In accordance with other studies there is not always a direct relationship between an abnormal DSEP level and the stenotic levels found on imaging because the rootlets in the lumbar and sacral regions pass through multiple spinal segments as they course through the spinal canal. Thus, the term multiple lumbosacral root disease (MRD) is a more accurate label than LSS for the results of a DSEP studies. Neurophysiologically, single root disease could occur in LSS, but its presence could also indicate a herniated nucleus pulposus.Citation20
Out of the 10 patients with radiological evidence of unilateral compression of one or more roots, nine patients showed bilateral DSEP abnormalities. Moreover, in eight patients with no radiological evidence of root compression, DSEPs revealed abnormalities in one or more levels. These findings indicate that DSEPs are more superior to imaging studies in the ability to detect neurological compromise in patients with radiological evidence of LSS. In a controlled blind study of electrodiagnosis and MRI for older subjects it was found that imaging did not differentiate symptomatic from asymptomatic persons with LSS, whereas electrodiagnosis did. So, it is believed that radiographic findings alone are insufficient to justify surgery for spinal stenosis.Citation33
5 Conclusion
In conclusion, mixed and dermatomal SEP studies can reflect the extent of neurological deficits in LSS patients even earlier before the patients develop the classic symptoms (subclinical cases). SEP techniques have the ability to detect abnormalities in patients with LSS more than late responses. DSEP studies have a role in the diagnosis of LSS by demonstrating multiple root abnormalities. They are more sensitive than mixed SEP in the diagnosis of neurological deficits in LSS patients. They can be used as an add-on diagnostic procedure to imaging studies in patients with LSS.
It can be recommended that a combination of clinical, radiological and electrodiagnostic tests, especially DSEPs, should be included in the evaluation of patients with suspected LSS. Data on CT and MRI findings of the lumbar spine of asymptomatic subjects should be interpreted cautiously as radiologic findings may not represent physiologically important LSS. Further studies correlating imaging and electrophysiological procedures with operative findings need to be done to document the role of these diagnostic studies in accurate evaluation of LSS patients.
Conflict of interest
The authors have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine
Available online 19 July 2012
References
- H.VerbiestA radicular syndrome from developmental narrowing of the lumbar vertebral canalJ Bone Joint Surg36-B1954230237
- R.W.PorterSpinal stenosis and neurogenic claudicationSpine21199620462052
- T.AmundsenH.WeberF.LilleasH.J.NordalM.AbdelnoorB.MagnaesLumbar spinal stenosis: clinical and radiologic featuresSpine20199511781186
- D.K.BinderM.H.SchmidtPh.R.WeinsteinLumbar spinal stenosisSemin Neurol2222002157166
- F.PostacchiniManagement of lumbar spinal stenosis. Instructional course lectureJ Bone Joint Surg78-B1996154164
- S.D.BodenD.O.DavisT.S.DinaT.S.PatronasS.W.WieselAbnormal magnetic resonance scans of the lumbar spine in asymptomatic subjectsJ Bone Joint Surg72-A1990403408
- D.EgliO.HausmannM.SchmidN.BoosV.DietzA.CurtLumbar spinal stenosis: assessment of cauda equina involvement by electrophysiological recordingsJ Neurol2542007741750
- M.K.AlfieriJ.R.HesselinkMR imaging of spinal stenosisAppl Radiol26819971827
- D.C.PrestonB.E.ShapiroElectromyography and neuromuscular disorders1998Butterworth-HeinemannBoston, Oxford, Johannesburg, New Delhi, Singapore2358
- Bingöl S, Soysal A, Yüksel B, Mutluay B, Arpacı B. Dermatomal somatosensory evoked potentials in the diagnosis of patients with lumbosacral radiculopathies. Düşünen Adam Psikiyatri ve Nörolojik Bilimler Dergisi 2010;23:185–94.
- L.Saint-LouisLumbar spinal stenosis assessment with computed tomography, magnetic resonance imaging, and myelographyClin Orthop3882001122136
- R.VrankenP.StormD.ChouLumbar spinal stenosis, cauda equina syndrome, and multiple lumbosacral radiculopathiesPhys Med Rehabil Clin N Am132002713733
- S.ChungC.LeeS.KimM.ChungJ.AhnEffect of low back posture on the morphology of the spinal canalSkeletal Radiol292000217223
- M.ModicJ.RossLumbar degenerative disc diseaseRadiology24520074361
- J.FritzA.DelittoW.WelchR.ErhardLumbar spinal stenosis: a review of current concepts in evaluation, management, and outcome measurementsArch Phys Med Rehabil7961998700708
- J.N.WeinsteinT.D.TostesonJ.D.LurieSPORT investigators surgical versus nonsurgical therapy for lumbar spinal stenosisN Engl J Med3582008794810
- H.KatifiE.SedgwickEvaluation of the dermatomal somatosensory evoked potential in the diagnosis of lumbosacral root compressionJ Neurol Neurosurg Psychiatry50198712041210
- N.KoharaJ.KimuraR.KajiF-wave latency serves as the most reproducible measure in nerve conduction studies of diabetic polyneuropathy: multicentre analysis in healthy subjects and patients with diabetic polyneuropathyDiabetologia432000915921
- G.EhniSurgical treatment of spondylitic caudal radiculopathyP.WeinsteinG.EhniC.WilsonLumbar Spondylosis: diagnosis, management and surgical treatment1977Year Book Medical PublishersChicago146183
- G.KraftDermatomal somatosensory-evoked potentials in the evaluation of lumbosacral spinal stenosisPhys Med Rehabil Clin N Am1420037175
- J.C.SlimpD.E.RubnerM.L.SnowdenDermatomal somatosensory-evoked potentials: cervical, thoracic, and lumbosacral levelsElectroencephalogr Clin Neurophysiol70199255
- Y.TokuhashiK.SantohS.FunamiA quantitative evaluation of sensory dysfunction in lumbosacral radiculopathySpine16199113211328
- M.SnowdenJ.HaselkornG.KraftDermatomal somatosensory evoked potentials, electromyography and radiologic imaging in lumbosacral spinal stenosisArch Phys Med Rehabil73199289
- S.HallJ.BartlesonB.OnofrioLumbar spinal stenosis: clinical features, diagnostic procedures, and results of surgical treatment in 66 patientsAnn Intern Med10321985271275
- M.SnowdenJ.HaselkornG.KraftSomatosensory evoked potentials in the diagnosis of lumbosacral spinal stenosis: comparison with imaging studiesMuscle Nerve159199210361044
- D.DumitruP.DreyfussDermatomal/segmental somatosensory-evoked potentials evaluation of L5/S1 unilateral/unilevel radiculopathiesMuscle Nerve1941996442449
- A.J.HaigH.C.TongK.J.YamakawaThe sensitivity and specificity of electrodiagnostic testing for the clinical syndrome of lumbar spinal stenosisSpine30200526672676
- A.WilbournM.AminoffAAEM minimonograph 32: the electrodiagnostic examination in patients with radiculopathiesMuscle Nerve2112199816121631
- J.M.SpivakDegenerative lumbar spinal stenosisJ Bone Joint Surg80199810531066
- C.GettyLumbar spinal stenosis: the clinical spectrum and the results of operationJ Bone Joint Surg62-B41980481485
- L.MorelandA.Lopez-MendezG.AlarconSpinal stenosis: a comprehensive review of the literatureArthritis Rheum1921989127149
- M.FisherS.PerlikD.PatelOn the usefulness of somatosensory-evoked responses for the evaluation of lower back painArch Neurol431986907913
- M.GeisserA.J.HaigH.C.TongSpinal canal size and clinical symptoms among persons diagnosed with lumbar spinal stenosisClin J Pain2392007780785