Abstract
Objective
This study was conducted to compare and evaluate the therapeutic effects of ultrasound guided local steroid injection versus medium frequency shock wave therapy in plantar fasciitis treatment among Egyptian population.
Patients and methods
Between May 2009 and May 2010, 60 patients (27 males, 33 females), otherwise healthy individuals with the diagnosis of unilateral plantar fasciitis were included in this study. All patients underwent subjective assessment following The Mayo clinical scoring system and objective assessment through measuring plantar fascia thickness by US imaging. Patients were randomly classified into two equal groups; group A had ultrasound guided local steroid injection, and group B received high dose of extracorporeal shock wave therapy.
Results
There was a statistically significant reduction in plantar fascia thickness after treatment in both groups, while no statistically significant difference between the study groups. According to assessment with Mayo clinic scoring system, despite the fact that both groups showed statistically significant improvement at the end of follow up period, there was no statistically significant difference between the study groups.
Conclusion
Both treatment groups showed significant clinical and radiological improvement of plantar fasciitis after therapy with statistically non-significant superior results of the extracorporeal shock wave therapy group. However, we do recommend local steroid injection as our preferred method of treatment as it attains clinical improvement at a much better cost effective value.
1 Introduction
Plantar fasciitis (PF) is the most commonly reported cause of chronic pain beneath the heel.Citation1,Citation2 About 10% of the population complains of heel pain at some point in life, and the condition accounts for about 2.5 million people each year in the United States.Citation3 The condition is associated with significant morbidity placing activity limitations on the affected patients.Citation4–Citation6
PF is characterized by microscopic tearing of the plantar fascia, which is a long ligament on the bottom of the foot. This ligament (the plantar fascia) is responsible for maintaining the arch of the foot. When the plantar fascia pulls away from the bone, the heel becomes painful. As a result of continuous pulling, tissue may react by filling this space with new bone – a heel spur. Most people think that heel spurs are the cause of their foot pain, but the pain is actually caused by the inflammation or irritation of the plantar fascia and muscle.Citation5
PF is characterised by pain at the calcaneal origin of the plantar fascia that is usually worse with their first steps in the morning or after a period of inactivity, and made worse by increased duration of weight-bearing.Citation1,Citation2 The most common pathological features are deterioration of collagen fibres, increased secretion of ground substance proteins, focal areas of fibroblast proliferation and vascular congestion.Citation6
The diagnosis of plantar fasciitis can be made with reasonable certainty on the basis of clinical assessment alone.Citation4
Ultrasonography has been well recognized as an effective imaging diagnostic tool for plantar fasciitis,Citation7,Citation8 with advantages of being non-invasive, well tolerated by patients, cost effective, free of radiation, and able to provide perfect spatial resolution for superficial structures.Citation9,Citation10 Given the thickening of the plantar fascia as a commonly observed finding with ultrasound in patients with PF, it is postulated that there should be a decrease in the plantar fascia thickness as the patients improve in their symptoms with treatment.Citation11
The goals of treatment are to alleviate pain and restore function. Treatment of plantar fasciitis is mainly conservative, with more than 80–90% of patients responding positively.Citation12 Surgical treatment with either open or an endoscopic release of the plantar fascia has been recommended in patients who failed to respond to conservative treatment.Citation13,Citation14
Conservative treatment modalities for the treatment of plantar fasciitis includes, among others: non-steroidal anti-inflammatory drugs, heel cushions, stretch exercise, physiotherapy, local injections, and extracorporeal shock wave therapy.Citation14,Citation15 The response of plantar fasciitis to any treatment is unpredictable.Citation14,Citation16
Local injection is a commonly used treatment modality for PF. Most authors recommend steroid injection,Citation16–Citation19 although there are some trials for other injectables like botulinum toxin,Citation20 hyperosmolar dextrose/lidocaineCitation21 and autologous platelet concentrate.Citation22,Citation23
Corticosteroids have been shown to inhibit fibroblast proliferation and expression of ground substance proteins. It is possible that these known effects may be of benefit in the treatment of plantar fasciitis, as increased fibroblast proliferation and excessive secretion of proteoglycans are commonly reported features of the condition.Citation16,Citation24
Shock waves (SWs), defined as a sequence of single sonic pulses characterised by high peak pressure, a fast rise in pressure and a short lifecycle, are conveyed by an appropriate generator to a specific target area. Extracorporeal SW therapy was first used on patients in 1980 to break up kidney stones. This technique has been successfully employed in orthopaedic diseases such as pseudoarthosis, tendinitis, calcification of the shoulder, epicondylitis, plantar fasciitis and several inflammatory tendon diseases. In particular, treatment of the tendon and muscle tissues was found to induce a long-time tissue regeneration effect in addition to having a more immediate analgesic and anti-inflammatory outcome.Citation25–Citation27
The FDA approved extracorporeal shockwave therapy (ESWT) for the treatment for plantar fasciitis was in 2000. Since that time, numerous studies have investigated the use of shock wave treatments for recalcitrant cases of plantar fasciitis.Citation24
The ESWT are sound waves that create vibrations and cause controlled injury to the plantar fascia and the surrounding structures at the heel. The body responds by increasing its healing ability at that area, stimulating a repair process. The mechanism of this type of therapy is unknown, however, it has been suggested that ESWT induce micro-destruction of avascular or minimally vascular tissues, which encourage revascularization, the release of local growth factors and the recruitment of appropriate stem cells; leading to an enhancement of the intrinsic wound healing process.Citation5,Citation19,Citation28,Citation33
Several previous studies evaluate the effects of either local injection therapy or shock wave therapy versus sham therapy in plantar fasciitis treatment,Citation5,Citation26,Citation30,Citation32 but comparison between the therapeutic effects of local steroid injection therapy versus ESWT in PF treatment is lacking in the literature.
The aim of this study was to evaluate and compare the therapeutic effectiveness of ultrasound guided local steroid injection versus ESWT in plantar fascia thickness through both clinical and radiological assessment. And to investigate whether the body mass index (BMI) is a risk factor in each group .The choice of ultrasound guided technique of steroid injection was related to the accuracy of application and superior results among available literatures.
2 Patients and methods
Between May 2009 and May 2010, 60 patients (27 males, 33 females), otherwise healthy individuals with the diagnosis of unilateral plantar fasciitis were selected from the out-patient clinic of orthopaedic and Physical therapy Departments of Ain Shams University. The diagnosis of PF was made upon the finding of tenderness to pressure at the origin of the plantar fascia on the medial tubercle of the calcaneus, as well as complaint of sharp shooting inferior foot pain, made worse with activity and/or upon arising in the morning.
Inclusion criteria were: (1) symptomatic heel pain of greater than 6 months duration and (2) unsuccessful response to conservative treatment with NSAIDS and stretch exercises. Patients with systemic inflammatory disease, connective tissue disease, herniated intervertebral disc of the lumbar spine, or previous local trauma and those with bilateral plantar fasciitis were excluded from the study. Patients with overt tarsal tunnel syndrome and those who gave history of recent administration of local steroid injection within last 3 months were excluded from the study.
2.1 Study design
All patients underwent functional assessment of pain and its impact on functional status, footwear requirement and effect on the gait by The Mayo clinical scoring system (total 100 points) which comprises six parameters; (degree of Pain, activity limitations, footwear or orthotic requirement, plantar heel tenderness, neuropathy, and antalgic gait).Citation35 Scoring is classified as excellent results (90–100 points), good results (80–89), fair (70–79), poor < 70. Weight and height measurements were recorded to calculate body mass index (BMI).
2.2 Radiographic evaluation
All patients were evaluated by plain heel radiographs to diagnose a calcaneal spur or any pre-existing foot anomaly.
2.2.1 Ultrasound protocol
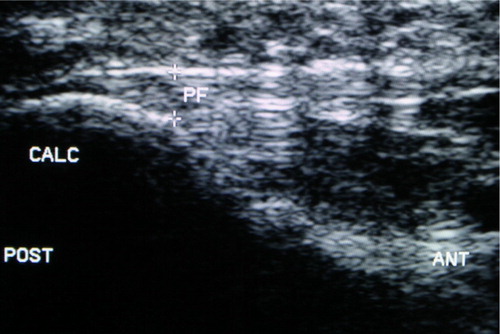
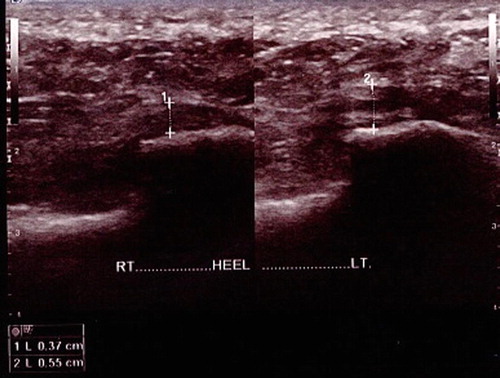
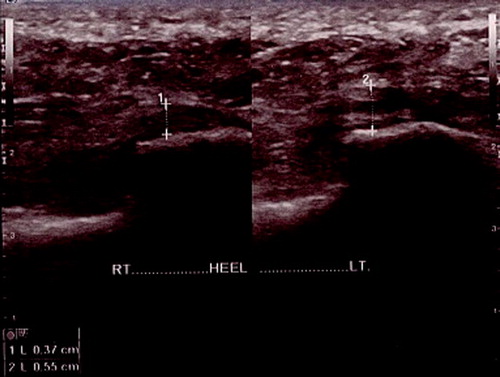
All patients were evaluated through high resolution Ultrasound imaging, to measure the thickness of plantar fascia in the affected and the sound sides. The thickness of the plantar fascia was measured at the thickest portion from the base of the medial calcaneal tubercle where a bright echogenic line was easily visible.
2.2.2 Patient consent
All the selected patients were motivated to the treatment, and they agreed to co-operate and follow the recommendations and instructions of the clinician.
Patients were randomly assigned to two equal treatment groups:
| Group A: | Treated with palpation guided injection for two sessions with 2 weeks interval. | ||||
| Group B: | Treated with medium energy density (0.28 mJ/mm2); shock wave therapy in the area of maximal tenderness and positive finding by U/S for two sessions with 2 weeks interval. | ||||
Local injection for group A was done through aseptic technique, including twice injection of 2 mL of 4 mg/mL (betamethasone diproprionate and betamethasone sodium phosphate), combined with local anaesthetic; 0.5% zylocaine hydrochloride). Injection procedures were separated by 2 weeks.
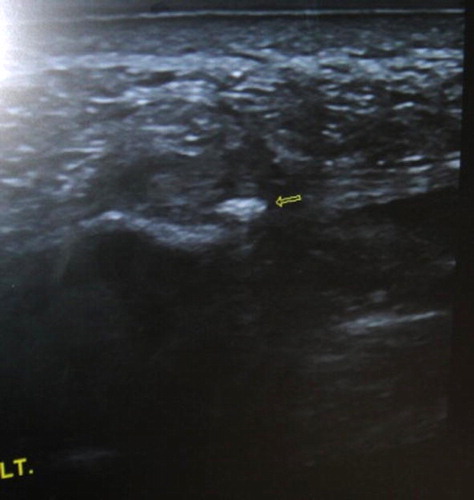
The patient is placed in the lateral recumbent position with the affected side down. The soft tissue just distal to the calcaneus is palpated, locating the point of maximal tenderness or swelling. At the defined soft tissue area, confirmed by ultrasound, the needle is inserted through the medial heel, perpendicular to the skin and to the long axis of the ultrasound transducer (–). The needle will be advanced under continuous guidance into the proximal plantar fascia, past the midline of the width of the foot. Injection into the fat pad at the base of the foot was totally avoided.
2.3 Shock wave therapy for group B
The patient was lying in prone position over the treating table, the foot was positioned over pillow to be sure that the foot position remains constant throughout therapy. All the procedures were performed under local transcutaneous ultrasound mediated infiltration of lidocaine hydrochloride gel 2% and was explained to the subject prior to the test. Shockwaves were applied using an electro hydraulic shock wave generator. They were bundled into a focal area guided by LASER locating aid which helps to adjust the focal point for the treatment. The head of the shock wave device was coupled to the most tender point of proximal heel using ultrasonic gel as a coupling medium, and then two series of shocks were applied. The energy intensity applied ranged from 14 to 17 kV, 2 Hz, 1000–1500 pulses and were divided into two distinct directional applications, which were applied at 45° to the target area (). Same technique is repeated after two weeks.
Following treatment, participants will be advised to avoid all running and other high impact activities for at least 2 weeks. Patients were followed-up for a mean of 20 weeks (range 12–24 weeks). At twelve weeks visit, Mayo clinical scoring is recalculated and thickness of plantar fascia is re-examined with ultrasound imaging.
2.4 Statistical analysis
The data was collected and tabulated. Statistics was done using SPSS programme V10. The following tests were done:
| – | Mean and standard deviation were calculated for numerical variables. | ||||
| – | Paired sample Student's t-test was done to compare between two numerical variables (pre and post). | ||||
| – | Independent sample Student's t-test was done to compare between two groups regarding numerical variables. | ||||
| – | Pearson correlation coefficient was done to test linear relation between two numerical variables. | ||||
| – | P value was calculated for all tests and interpreted as following: <0.05, significant; <0.001, highly significant; >0.05, non-significant. | ||||
3 Results
The demographic data of the patients are listed in (). There was no significant difference in age, sex, or body mass index between the two treatment groups.
Table 1 Demographic data of the two treatment groups.
Twenty patients had calcaneal spurs in their heel on X-ray films. All of the spurs discovered incidentally on X-ray.
At 12 weeks follow up, subjective assessment with Mayo clinic scoring system and objective assessment through measuring the thickness of planter fascia. The recorded data are analysed and statistical analysis was conducted with preoperative values.
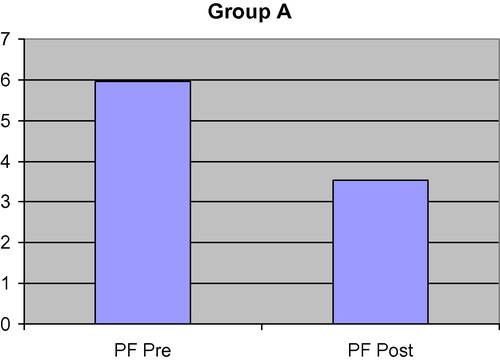
Objective analysis through measurement of the thickness of plantar fascia in the ultrasound guided injection group (group A) showed statistically significant improvement from a mean of 5.9567 ± 0.4591 before treatment to a mean of 3.5433 ± .3148 after treatment (t = 39.33, P < 0.00) ().
Table 2 Comparison between PF thickness pre and post treatment in group A. Comparison between Mayo CSS pre and post treatment in group A.
showed significant decrease in PF thickness post treatment as well as significant increase in Mayo CSS post treatment in group A.
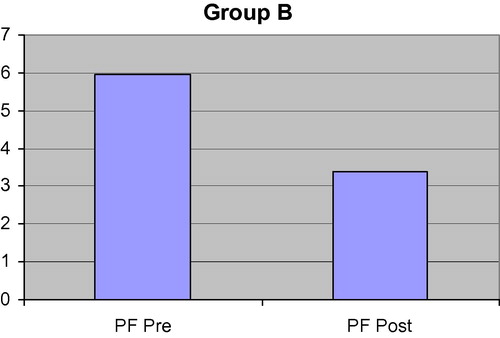
The group of ESWT (group B) had also showed significant decrease in plantar fascia thickness from 5.9367 ± .5353 before treatment to a mean of 3.3733 ± .4152 after treatment (t = 35.7, P < 0.001) ((A and B) and (A and B)).
Subjective analysis according to Mayo clinic scoring system, patients within ultrasound guided injection group (group A) showed statistically highly significant improvement from a mean of 46.66 ± 10.44 pre injection to a mean of 84.00 ± 6.6176 post injection (t = −23.549, P < 0.001)with 8 (13%) patients had excellent score. . The ESWT group (group B) had also showed highly significant improvement from 46.8333 ± 9.60 pre ESWT to a mean of 85.83 ± 6.83 post ESWT (t = −24.984, P < .001), with 17 (28%) patients had excellent score.
On comparing the change in Plantar fascia thickness between group A & B pre treatment and post treatment it showed non-statistically significant difference between 2 groups (t = 0.155, P = 0.877 and t = 1.78, P = 0.079, respectively).
Moreover, there was no statistically significant difference in Mayo CSS score between the two treatment groups before and after treatment (t = −0.064, P = 0.949 and t = −1.056, P = 0.296, respectively) ().
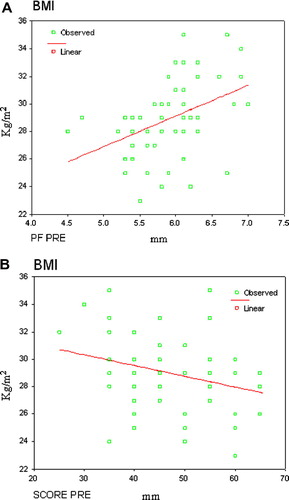
Groups A and B were further analysed by way of the Pearson correlation analysis to reveal a significant positive correlation between the plantar fascia thickness before treatment and BMI (rA = .420, PA < .05 and rB = 0.392, PB < 0.05, respectively) (A and B), and a significant negative correlation between plantar fascia thickness before treatment and the Mayo CSS pre treatment (rA = 0.681, rB = 0671, respectively, and PA = 0.001, PB = 0.001, respectively).
At a mean follow-up of 4.3 months (range 3–6 months), 90% of patients in both treatment groups showed good to excellent results according to Mayo clinic scoring system. Two patients in each group (7%) showed poor response to treatment.
A total of six patients (20%) showed recurrent symptoms of plantar fasciitis. The time before recurrence ranged from 5 months to 7 months (mean 6.1 months). The recurrent patients included three patients from each treatment group. There were no haematoma, bruising or swelling over the treated area in both groups.
4 Discussion
Although the most common cause of heel pain is plantar fasciitis, the aetiology and treatment are still not fully understood.Citation14,Citation36,Citation37 The diagnosis of plantar fasciitis is based on the patient's history and physical findings for at least 6 months.Citation4 This is in accordance with most studies which included only patients who had symptoms for 6 months or longer, and who had failed conservative treatment.Citation35 The population shared in this study comprised of 35 females (58%) and 25 males (42%) with average age 34.23 ± 6.67 and BMI 28.8000 ± 2.61 randomly divided into two equal groups with no statistically significant difference between them.
The accuracy of radiological studies in diagnosing plantar heel pain is unknown. In the current study, measurement of PF thickness by high resolution US technique was chosen based on confirmed published data that (US) has been well recognized as an effective imaging diagnostic tool for PF, and able to provide perfect spatial resolution for superficial structures and correlated with Patient Self Reported Improvement.Citation8,Citation13,Citation39 Moreover, Ultrasound is superior to MRI for diagnosis of plantar fibroma as small low signal lesions on MRI are similar to the normal plantar fascia signal. Ultrasound demonstrates low echogenicity compared with the echogenic plantar fascia.Citation8
Thickening of the plantar fascia insertion more than 4 mm would be abnormal and more than 5 mm is suggestive of plantar fasciopathy. This was confirmed by Hammer et al. and Karabay et al.Citation13,Citation39 In the current study, mean PF thickness of group A pre-treatment is 5.9567 ± 0.4591 and 5.9367 ± .5353 for group B. As the efficacy of intralesional steroid injection has been proven in multiple literatures.Citation41,Citation42 In current study, group A, the US guided local steroid injection technique was performed and preferred on palpation guided local injection, to ensure accuracy of application and the objective evaluation of prognosis .This was previously confirmed in the literature, by many authorsCitation43 who did document in their study that ultrasound guided injection is superior to palpation guided technique in both the reduction of thickness and recurrence rate of plantar fasciitis. However, others considered there were no statistically significant differences in the plantar fascia thickness and visual analogue scale of pain among groups treated by those two techniques. Accordingly, some authors recommended both techniques as more efficacious and cost effective than other modalities including ESWT.Citation44 Selection of a particular CS agent for local injection varies across disciplines, with limited evidence available to assist in decision-making.Citation45,Citation46 In relation to treatment outcomes, systematic reviews of randomised trial data have revealed no difference in clinical efficacy between various CS types. Additionally, high solubility preparations (e.g. Betamethasone sodium phosphate) are thought to reduce the risk of post-injection flare and soft-tissue atrophy.Citation31
Accordingly, Betamethasone sodium phosphate was considered the most appropriate corticosteroid for use in this trial. This is comparable to Andrew et al. and Tsai et al.,Citation34,Citation47 they use Betamethasone and lidocaine in their design,they reported that the thickness had decreased significantly 3 months after injection.
In current study, 3 months later, Reassessment by Ultrasound imaging and subjective assessment by Mayo CSS was performed for both groups. Group A, showed significant improvement in the subjective (Mayo CSS) and in the objective (Plantar fascia thickness) assessment methods. This is in accordance to Tsai et al. and Yucel et al.,Citation34,Citation48 they mentioned significant improvements in plantar fascia thickness, fat pad thickness, and VAS without significant deterioration of the mechanical properties of the heel pads, in all patients receiving US guided local steroid injection.
Extracorporeal shockwave therapy (ESWT) for the treatment of musculoskeletal (MSK) disorders evolved in Europe in the early 1990s.Citation24,Citation29,Citation30 The efficacy of ESWT may be based on an enhancement of the wound healing cascade; a conversion of a chronic wound to an acute wound; which can then go a normal physiological wound healing process.Citation42 Furthermore, clinical observations indicate an immediate increase in blood flow around the treated area. Nevertheless, the biochemical mechanisms comprise neovascularization at the tendon junction by inducing of early release of angiogenesis-mediated growth and proliferating factor.Citation33,Citation35,Citation42
Based on these data, ESWT is applied in two sessions under local transcutaneous ultrasound mediated infiltration of local anaesthetic to group B as a comparative non-invasive treatment to local steroid injection. Therapy is of an energy density 0.28 mJ/mm2, 2 Hz, 1000–1500 pulses for two sessions. This is quiet similar to ESWT parameters used by Wen et al.,Citation35 their patients received 1000 impulses at 16 kV, medium-energy (0.55 mJ/mm2) in a single session. In current study, plantar fascia thickness reduction was statistically significant from (5.93 ± 0.53) pre ESWT to a mean of (3.37 ± 0.41), 12 weeks post ESWT. This is in agreement with Khan et al., Speed and Theodre et al., all of them reported significant reduction in plantar fascia thickness.Citation14,Citation28,Citation38
The results of this study were in agreement with the hypothesis of a significant decrease in plantar fascia thickness associated with symptomatic improvement in the patient group with PF subjective assessment by Mayo CSS was performed 3 months later and group B showed significant improvement in Mayo CSS score (t = −24.984, P < 0.001) with 52 (86.6%) patients showed good to excellent results. These findings were in common with Wang et al.,Citation33 they compared the effect of ESWT vs. conservative treatment for plantar fasciitis, the patients experienced significant improvement in pain and function by Mayo CSS. Additionally, Wen et al. reported that Mayo CSS score increased post ESWT with good to excellent result rate 86.9 + 18.2.Citation38 A recent Study in 2006 compared ESWT versus a sham procedure in 172 patients. The researchers found a statistically significant improvement of function and reduction of pain of group treated by ESWT over the sham treatment after 12 weeks and the patients experienced no significant complications or side effects.Citation20 A meta-analysis identified eight acceptable studies of sufficient duration of follow up (one year after treatment); the report concluded that the therapeutic application of ESWT is clinically effective for the treatment of chronic proximal plantar fasciitis.Citation26,Citation49
It was found that BMI of both groups (28.8 ± 2.61 and 29.523 ± 2.896) respectively, falls in the overweight category and there was a significant positive correlation between BMI and PF thickness pre treatment in both groups. This is in accordance with Ozdemir et al. and Heurta et al. they reported a significant positive correlation between BMI and Plantar fasciitis.Citation9,Citation40 This could be referred to possible association between plantar fasciitis formation and overloading, as overweight lead to chronic stretch and focal pressure on plantar fascia lead to PF.Citation11
In the current study, the reduction of plantar fascia thickness measured by U/S in both groups was statistically significant post treatment after 12 weeks. Although, the reduction in the thickness was more in ESWT group than local injection group, yet did not reach significant value. Those results are similar to those reported by Porter and Shaadbolt, found that ESWT and CS injection proved significant improvements in visual analogue scale and heel tenderness index scores, but between the two groups there was no significant difference in the VAS score change 3 months after treatment.Citation18
Recently, Yucel et al.Citation44 compared high-Dose ESWT and intralesional CS injection in the treatment of PF. In their study, they reported that the two treated groups showed significant improvements in visual analogue scale and heel tenderness index scores, but between the two groups there was no significant difference 3 months after treatment. Pribut, found out that CS injection and ESWT are successful treatment modalities for plantar fasciitis. However, local corticosteroid injection treatment is cost effective compared with ESWT, and CS injection may be the first treatment choice according to their results.Citation17
Others studies for PF have had conflicting results; undoubtedly that many issues surrounding ESWT like shockwave dosage, high versus low-energy ESWT, and the n umber of sessions required for a therapeutic effect.Citation34 while, It was previously ascertained that efficacy of ESWT may be highly dependent upon machine types and treatment protocols.Citation28,Citation36 However, much more work needs to be done in order to determine the best protocols and patient selection for the use of shock wave therapy.Citation27
5 Conclusion
Both local steroid injection and ESWT are proved effective in treatment of plantar fasciitis. Both groups showed significant clinical and ultrasound documented improvement of their disease after therapy with a slightly superior results of the ESWT group, yet we do recommend local steroid injection as our preferred method of treatment being more cost effective and has more reproducible results regardless of the machine or the operator. However, ESWT should be considered prior to any surgical treatment for recalcitrant PF.
Acknowledgement
We are appreciating the effort and cooperation by Dr. Mohammed ElTohamy for adding to this worthy work by accomplishing the statistics package of results.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 17 December 2011
References
- T.AldridgeDiagnosing heel pain in adultsAm Fam Physician702004332338
- L.AlmekindersJ.TempleEtiology, diagnosis and treatment of tendonitis: an analysis of the literatureMed Sci Sports Exerc30199811831190
- APMA News Release: http://www.apma.org/ [April 11, 2001].
- C.ColeC.Craig SetoJ.JohnPlantar fasciitis: evidence-based review of diagnosis and therapyAm Fam Physician7211200522372242
- J.RompeA.CacchioL.WeilJ.FuriaJ.HaistV.ReinersLow energy extracorporeal shockwave therapy for painful heelArch Orthop Trauma surg11519967579
- R.BuchbinderPlantar fasciitisN Eng J Med350200421592166
- N.KarabayT.TorosC.HurelUltrasonographic evaluation in plantar fasciitisJ Foot Ankle Surg4662007442446
- E.G.McNallyS.ShettyPlantar fascia: imaging diagnosis and guided treatmentSemin Musculoskelet Radiol1432010334343
- H.OzdemirE.YilmazA.MuratL.KarakurtA.PoyrazE.OgurSonographic evaluation of plantar fasciitis and relation to body mass indexEur Radiol542005443447
- N.SabirS.DemirlenkB.YageiN.KarabulutS.CubukeuClinical utility of sonography in diagnosing plantar fasciitisJ Ultrasound Med24200510411048
- J.FabrikantT.S.Tae Soon ParkbPlantar fasciitis; treatment outcome study: plantar fascia thickness measured by ultrasound and correlated with patient self reported improvement2009119
- W.TsaiC.HsuC.ChenM.ChenT.YuY.Ying-JenPlantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidanceJournal of Clinical Ultrasound34120061216
- D.S.HammerF.AdamA.KreutzS.RuppD.KohnR.SeilUltrasonographic evaluation at 6-month follow-up of plantar fasciitis after extracorporeal shock wave therapyArch Orthop Trauma Surg1251200569
- R.KulkarniConservative treatment of plantar fasciitisIndian J Orthop382004121123
- S.MalayExtracorporeal Shockwave Therapy versus placebo for the treatment of chronic proximal plantar fasciitis: randomised controlled, double blinded, Multicenter intervention TrialJFAS4542006196209
- C.KeatingS.BurkeA.WalshS.KearnsInjection of local anaesthetic and steroids for the treatment of plantar fasciitis under general anaestheticJ Bone Joint Surg92-BI201048
- S.PributCurrent approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroidsJ Am Podiatr Med Assoc97120076768
- M.PorterB.ShaadboltIntralesional corticosteroid injection versus extra- corporeal shockwave therapy for plantar fasciopathyClin J Sport Med152005119
- W.TsaiC.WangF.TangT.HsuK.HsuM.WongTreatment of proximal plantar fasciitis with ultrasound-guided steroid injectionArch Phys Med Rehabil8110200014161421
- Y.HuangS.H.WeiH.WangF.LieuUltrasonographic guided botulinum toxin type A treatment for plantar fasciitis: an outcome-based investigation for treating pain and gait changesJ Rehabil Med4222010136140
- M.B.RyanA.D.WongJ.H.GilliesJ.WongJ.E.TauntonSonographically guided intratendinous injections of hyperosmolar dextrose/lidocaine: a pilot study for the treatment of chronic plantar fasciitisBr J Sports Med432009303306
- Barrett S, Erredge S. Growth factors for chronic plantar fasciitis? 2004; 17(11). http://poditryinsitute.com/info [Medline].
- S.CorottiR.VaqueroB.BeltranLarraMiranda deTreatment of chronic plantar fasciitis with autologus platelet concentrateJ Bone Joint Surg91-BI2009162
- R.AlvarezPreliminary results on the safety and efficacy of the Ossatron for treatment of plantr fasciitisFoot Ankle Int2332002197203
- F.KhanJ.HartyC.HealyR.StackP.HessionL.D'souzaExtra corporeal shockwave therapy for the treatment of plantar fasciitisJ Bone Joint Surg88-BII2010286
- B.MorettiR.GarafaloV.PatellaG.SistiM.CornadoExtracorporeal shock wave therapy in runners with a symptomatic heel spurKnee Surg Sports Traumatol Arthrosc1410200610291032
- M.SofiaD.AlessandraC.ElisabettaA.ErnestoM.ErnstH.HisanoriExtracorporeal shock wave therapy in inflammatory diseases: molecular mechanism that triggers anti-inflammatory actionCurr Med Chem1619200923662372
- M.TheilApplication of shock waves in medicineClin Orthop38720011821
- C.WangAn overview of shockwave therapy in musculoskeletal disordersRev Chan Gung Med J262003220232
- J.A.OgdenR.G.AlvarezExtracorporeal shockwave therapy for chronic proximal plantar fasciitisClin Orthop Relat Res38720014759
- J.G.SkedrosK.J.HuntT.C.PittsVariations in corticosteroid/anesthetic injections for painful shoulder conditions: comparisons among orthopaedic surgeons, rheumatologists, and physical medicine and primary-care physiciansBMC Musculoskelet Disord6;8200763
- C.WangH.ChenT.HuangShockwave Therapy for Patients with Planter Fasciitis: A One-Year Follow-up StudyFoot Ankle Int2332002204207
- C.Wangk.YangShockwave therapy enhanced neovascularization at tendon-bone junction. A study in rabbitsJ Orthop Res212003984989
- J.A.OgdenR.G.AlvarezM.MarlowShock wave therapy for chronic proximal plantar fasciitis: a meta analysisFoot Ankle Int2342002301308
- L.Wen-hongH.Chin-JungH.Horng-ChaungT.Kuo-FungClinical application of extracorporeal shock wave therapy in treatment of plantar fasciitisMid Taiwan J Med112006230235
- F.CrawfordC.Thomson|Interventions for treating plantar heel painCochrane Database Syst Rev32003CD000416
- J.PearlJAMA28811200213371364
- G.TheodoreM.BuchA.AmendolaC.BachmannL.FlemingC.ZingasExtracorporeal shock wave therapy for the treatment of plantar fasciitisFoot Ankle Int2552004290297
- N.KarabayT.TorosC.HurelUltrasonographic evaluation in plantar fasciitisJ Foot Ankle Surg4662007442446
- J.HuertaJ.GarciaE.MatamorosJ.MatamorosT.MartinezRelationship of body mass index, ankle dorsiflexion, and foot pronation on plantar fascia thickness in healthy, asymptomatic subjectsJ Am Podiatr Med Assoc982008379385
- D.RiddleM.PulisicP.PidcoeR.JohnsonRisk factors for plantar fasciitis: a matched case-control studyJ Bone Joint Surg Am85-A2003872877
- C.SpeedExtracorporeal shockwave therapy in the management of chronic soft tissue conditionsJ Bone Joint Surg Br8622004165171
- C.WangAn overview of shockwave therapy in musculoskeletal disordersRev Chan Gung Med J262003220232
- I.YucelK.E.OzturaY.DemiraraE.DegirmenciG.KaynakComparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitisJ Am Podiatr Med Assoc10022010105110
- A.KalaciH.ÇakiciO.HapaA.NedimY.DogramaciT.Teoman ToniTreatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trialJ Am Podiatr Med Assoc9922009108113
- F.SorrentinoA.IovaneA.VetroA.VaccariR.MantiaM.MidiriRole of high resolution ultrasound in guiding treatment of idiopathic plantar fasciitis with minimally invasive techniquesRadiol Med1132008486495
- A.AndrewB.KarlF.MarkR.AdamD.AdamB.HyltonUltrasound guided injection of dexamethasone versus placebo for treatment of plantar fasciitis: protocol for a randomised controlled trialJ Foot Ankle Res3201015
- I.YucelB.YaziciE.DegirmenciB.ErdogmusS.DoganComparison of ultrasound-, palpation-, and scintigraphy-guided steroid injections in the treatment of plantar fasciitisArch Orthop Trauma Surg12952009695701
- C.SpeedD.NicholsJ.WiesH.HumphreysC.RichardsS.BurnetExtracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trialJ Orthop Res2152003937940