Abstract
Objective
ICU acquired muscle weakness (ICUAMW) is an acquired neuromuscular disorder associated with increased duration of mechanical ventilation and weaning suggesting a possible relation between the limb and respiratory neuromuscular involvement. There is no preventive tool and no specific treatment has been proposed for ICU acquired muscle weakness. Aim of this study was to assess the effect of electrical muscle stimulation on prevention of ICUAMW and in facilitating the weaning from mechanical ventilation in critically ill patients.
Design
A prospective, randomized, placebo-controlled trial.
Setting
Critical care department, main Alexandria university hospital.
Patients
80 Critically ill patients on mechanical ventilation for more than 24 h.
Methods
They were randomly categorized into two groups: 40 patients received conventional lines of treatment only (control group) and 40 patients received in addition one daily session of Electrical Muscle Stimulation (EMS) (EMS group). Assessment of occurrence of ICUAMW was done through the MEDICAL RESEARCH COUNCIL SCALE (MRCS) which is a method for clinical assessment of muscle strength.
Results
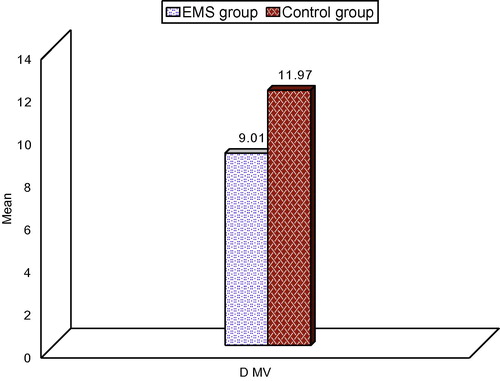
MRCS did not show any significant difference between the two groups in the first 3 days post mechanical ventilation while on day 4, MRCS mean value was 46.86 ± 10.88 in the EMS group versus 43.70 ± 9.32 in the control group (p = 0.041). On day 21, MRCS mean value was 29.67 ± 8.87 in the EMS group versus 19.60 ± 4.34 in the control group (p = 0.037). Significant difference was also noted in the duration of mechanical ventilation as the mean value in the EMS group was 9.01 ± 8.01 days versus 11.97 ± 8.07 in the control group (p = 0.048).
Conclusions
Although the EMS could not prevent the occurrence of ICUAMW in critically ill mechanically ventilated patients it still has a role in minimizing the degree of muscular weakness and could be helpful in facilitating weaning from mechanical ventilation.
1 Introduction
The ICU acquired muscle weakness (ICUAMW) is an acquired neuromuscular disorder which is considered a common complication of critical illness survivors presenting with profound muscle weakness and diminished or absent deep tendon reflexes which are associated also with increased duration of mechanical ventilation – weaning period suggesting a possible relation between the limb and respiratory neuromuscular involvement. In addition, the syndrome is associated with prolonged hospitalization and increased mortality. The diagnosis of ICUAMW requires a reliable bedside muscle strength examination and depends on patient’s cooperation and maximal effort.Citation1,Citation2
There is no preventive tool and no specific treatment has been proposed so far for ICU acquired muscle weakness but there are several risk factors that have been identified and should be adjusted. The risk factors include systemic inflammatory response and sepsis, medications such as corticosteroids and neuromuscular blocking agents, inadequate glycemic control, protracted immobility, hypoalbuminemia, gram-negative bacteraemia and severity of organ dysfunction and also electrolyte disorders.Citation3,Citation4
A number of studies have evaluated the role of early mobilization and/or physiotherapy in critically ill patients. These studies involved passive limb mobilization, limb and respiratory muscle training, and bed cycling. Although favorable results in terms of muscle strength, mobilization, six-minute walking distance and length of hospital stay have been shown, the development of ICUAMW was not evaluated.Citation5,Citation6
It is also noteworthy that limb and respiratory muscle training requires patient cooperation.Citation7
Many studies reported beneficial effects of Electrical Muscle Stimulation (EMS) on ICU acquired muscle weakness. The pathophysiological mechanisms that appear to improve muscle power and facilitate weaning from mechanical ventilator could be that EMS acts as an anabolic stimulus to the muscle reversing the catabolic effects of critical illness and immobilization that is to say EMS has beneficial effects on muscle metabolism and also it improves oxygen uptake (VO2) kinetics and work efficiency.Citation8,Citation9
Also EMS applied to the lower limbs of critically ill patients induced an acute systemic effect on the microcirculation as assessed with the near infrared spectroscopy technique, indicating the presence of factors induced by EMS, that act in a systemic way. It is possible that molecules such as cytokines, produced at the loci of EMS and distributed via the circulation could be responsible for the systemic effect of EMS in preventing ICUAMW. Several cytokine levels, primarily IL-6 have been shown to increase after exercise. IL-6 mRNA has been shown to increase after an EMS session in rat skeletal muscles.Citation10,Citation11
Moreover, it is possible that central command and activation of metabo-reflex and/or ergo-reflex during EMS may increase sympathetic discharge and contribute to changes in heart rate, systolic blood pressure, blood volume and cardiac output, and therefore affect the skeletal muscle metabolism in a systemic way.Citation12 Finally, a bio-energetic pathway may be activated during EMS contributing to an improvement in mitochondrial function of the skeletal muscle.Citation13
2 Aim of the work
The aim of this work was to assess the effect of electrical muscle stimulation in:
| 1. | Prevention of ICUAMW in critically ill patients. | ||||
| 2. | Facilitating the weaning from mechanical ventilation in critically ill patients. | ||||
3 Patients
The present study was carried out on 80 critically ill patients on mechanical ventilation for more than 24 h admitted to the critical care medicine department of Alexandria University Hospital in Egypt.
3.1 Exclusion criteria
| 1. | Age under 18 years. | ||||
| 2. | Pregnancy. | ||||
| 3. | Obesity (body mass index >35 kg/m2). | ||||
| 4. | Pre-existing neuromuscular disease. | ||||
| 5. | Patients receiving muscle relaxant. | ||||
| 6. | Diseases with systemic vascular involvement such as systemic lupus erythematosus. | ||||
| 7. | Technical obstacles that do not allow the implementation of EMS such as bone fractures or skin lesions (e.g. burns). | ||||
| 8. | End-stage malignancy. | ||||
| 9. | Patients with cardiac pacemakers. | ||||
| 10. | Patients with cervical spine fractures, hemiplegia, quadriplegia of neurological origin. | ||||
| 11. | Patients who could not be evaluated with the MRC score due to the impaired cognitive state. | ||||
| · | Patients were randomly categorized into two groups: | ||||
| a. | Group I: Forty patients received conventional lines of treatment only. | ||||
| b. | Group II: Forty patients received conventional lines of treatment in addition to one daily session of electrical muscle stimulation. | ||||
4 Methods
Written informed consents were obtained from all patients’ relatives and the approval of local ethics committee was also obtained.
4.1 Selection of the patients
All patients in the study were subjected to the following:
| 1. | Full history taking. | ||||
| 2. | Complete physical examination. | ||||
| 3. | Body mass index according to the equation: BMI = body weight (in kg) ÷ height (in squared meters) | ||||
| 4. | Radiological examination in the form of chest X-ray. | ||||
| 5. | Laboratory investigations | ||||
| 6. | Identification of the patient’s main diagnosis and reason for mechanical ventilation. | ||||
4.2 Technique
EMS was implemented simultaneously on the quadriceps muscles of both lower extremities starting from the second day after admission using the pointer probe. The stimulator delivered biphasic, symmetric impulses of 50 Hz, 200 μs pulse duration, 15 s on (including 1 s rise time and 1 s fall time) at intensities able to cause visible contractions (mostly 100–150 MA). In case of doubt, contraction was confirmed by palpation of the muscles involved. The session was done once daily for a period of 1 h including 5 min for warm up and 5 min for recovery.Citation14
4.3 Equipment:
| • | Model: Dr. Eldakr Digital Electronic Acupunctoscope. | ||||
| • | Site of production: Hong Kong. | ||||
| • | Name of company: 2D trading company. | ||||
| • | Frequency of muscle stimulation: two frequency ranges setting from 1 to100 Hz and from 10 to 999 Hz. | ||||
| • | Components:
| ||||||||||||||||||||||||||||||||||
Assessment of occurrence of ICUAMW was done through the MEDICAL RESEARCH COUNCIL SCALE (MRCS) which is a method for clinical assessment of muscle strength.Citation15 After interruption of sedation, patients were screened daily for awakening and comprehension for a period of 28 days or until the time of weaning from mechanical ventilation each of which is nearer. MRCS was assessed on the day the patients had a level of consciousness adequate to respond to at least three of the following orders (‘open/close your eyes’, ‘look at me’, ‘put out your tongue’, ‘nod your head’, ‘raise your eyebrows’).Citation16 Three muscle groups in all four limbs were assessed with the MRC scale with values ranging from 0 (quadriplegia) to 60 (normal muscle strength).Citation17 The functions assessed are shown in and grading of muscle strength according to MRCS is shown in .
Table 1 Functions assessed in MRCS.
Table 2 Grading of muscle strength according to MRCS.
Patients with an MRC score of less than 48 of 60 were diagnosed with ICUAMW. The cut-off limit of 48 for the MRC score was selected because it indicates clinically significant weakness and has been used previously for the clinical identification of ICU-acquired paresis.Citation18
4.4 Measurements
Comparison between the two groups of patients regarding the MRCS and duration of weaning from mechanical ventilator.
4.4.1 Statistical analysis of data
Data were analyzed using SPSS software package version 18.0 (SPSS, Chicago, IL, USA). Quantitative data were expressed using minimum, maximum, mean, standard deviation, median, and IQP while qualitative data were expressed in frequency and percent. Qualitative data were analyzed using Fisher exact and Monte Carlo test to compare different groups. Not normally distributed quantitative data were analyzed using the Mann Whitney test for comparing two groups while for more than two groups the Kruskal Wallis test was applied. The level of significance was 5.0%.
5 Results
This study was done over a period of 8 months in the critical care department of Alexandria University in Egypt. Two hundred and fifteen patients admitted to the ICU during this period were mechanically ventilated. Only 80 patients of them were fulfilling the criteria of inclusion in the study and accepted to be involved in the study. Those 80 patients were randomly assigned to receive the EMS. Patients with an odd number were assigned to the EMS group and patients with an even number were assigned to the control group. Patients assigned to the EMS group received daily EMS sessions of both lower extremities starting from the second day after admission until ICU discharge. Patients in the control group did not receive EMS.
Baseline characteristics of continuous variables of the EMS group and the control group for the whole cohort were compared by unpaired Student’s t-test or Mann–Whitney U test (). Qualitative variables at baseline were compared by chi-square test. All continuous variables are presented by mean ± standard deviation (SD). p Values of less than 0.05 were considered statistically significant.
Table 3 Baseline characteristics of patients in the EMS and control groups.
showed the baseline characteristics of the two studied groups which did not show any significant statistical difference.
showed a comparison between the two studied groups regarding MRCS at different periods of follow up. The MRCS at day 2 and day 3 were not significantly different between the two groups while a significant better score was recorded in the EMS group at day 4 and all through till day 21.The MRCS at day 28 did not represent any statistical significant difference (p = 0.091).
Table 4 Comparison between the two studied groups regarding MRCS at different periods of follow up.
showed the duration of mechanical ventilation in the two studied groups. It was 9.010 ± 8.01 days in the EMS versus 11.97 ± 8.07 days in the control group. A significant difference could be recorded between the two groups (p = 0.048).
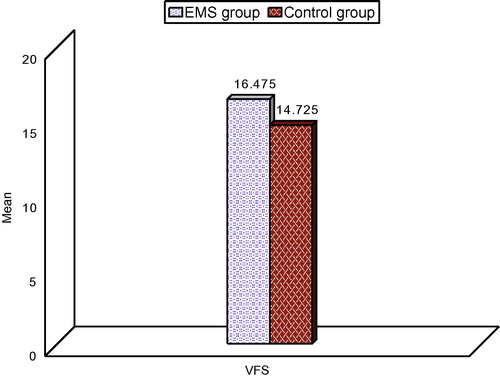
showed the ventilator free survival out of 28 days in both studied groups which did not show any significant difference between the two groups being 15.175 ± 9.65 days in the EMS group versus 14.725 ± 9.70 days in the control group (p = 0.421).
showed the different outcome in the two studied groups. The outcome was significantly better in the EMS group as 31 patients (77.5%) were successfully weaned in the EMS group versus 27 patients (67.5%) in the control group. Regarding the 28 days mortality, 4 patients (10%) died in the EMS group versus 6 patients (15%) in the control group. While the patients who remained ventilated at the end of 28 days due to weaning failure were 5 (12.5%) in the EMS group versus 7 (17.5%) in the control group (p = 0.046).
Table 5 Comparison between the two studied groups regarding outcome.
Regarding the complications related to the application of electrical stimulation (EMS group), there were no major complications as only 6 patients (15%) had a prickling sensation which was not clinically significant.
6 Discussion
Although advances in critical care and mechanical ventilation over the past 2 decades have resulted in the increased survival of patients who are critically ill, some patients develop the need for prolonged mechanical ventilation (PMV). Patients requiring PMV are frequently deconditioned because of respiratory failure precipitated by the underlying disease, the adverse effects of medications, and a period of prolonged immobilization.Citation2,Citation15 Patients requiring PMV often have substantial weakness of the respiratory and limb muscles that further impairs their functional status and health-related quality of life.Citation18 Alternative care settings for patients requiring PMV have been set up in order to wean them off the ventilator. Outcome studies in patients requiring PMV in these care units have focused more on the weaning outcome, disposition, and survival data, whereas only limited information is available on functional status assessed using validated instruments.Citation19–Citation22
The aim of this study was to assess the effect of electrical muscle stimulation on prevention of ICUAMW in critically ill patients and its role in facilitating the weaning from mechanical ventilation.
MRCS assessment for all patients started on the second day of mechanical ventilation which was not significantly different between the two groups (p = 0.497). The striking finding that MRCS values starting from day 3 post mechanical ventilation in both groups were below 48 – which is considered as the cut-off value for diagnosis of ICUAMW – denotes a very fast development of muscle wasting which was shown to be progressive by time as shown by the serial decrease in MRCS values until reaching 20.6 and 21 in the EMS and control groups respectively by the end of the study (day 28).
Our results are matching with MartinCitation23 who reported significant limb muscle weakness in patients who were ventilator dependent, with mean limb strength scores of less than 3 using a 5-point Medical Research Council motor score.
In contrast to our study, is RoutsiCitation14 study which also showed better MRCS in the EMS group compared to control but it was different from our results on showing higher MRCS in both groups. The MRC score was statistically significantly higher in patients assigned to the EMS group as compared with the control group (median = 58, range = 33–60 vs median = 52, range = 2–60) (p= 0.04). This difference between the two studies can be explained based on the different baseline characteristics of the patients involved in the two studies. As it is obviously noticed that our patients are much sicker than the patients in Routsi C Study. Apache II score was around 25 in our study while it was less than 20 in both the EMS and control group in the other study which clarifies the relationship between development of ICUAMW and the severity of illness not only on the term of the degree of affection but also on how fast this can happen in seriously ill patients.
In the same context, another study was done by GerovasiliCitation24 on forty-nine critically ill patients (age: 59 ± 21 years) with an APACHE II admission score ⩾13 who were randomly assigned after stratification upon admission to receive daily EMS sessions of both lower extremities (EMS-group) or to the control group (control group). Muscle mass was evaluated with ultrasound (US), by measuring the cross sectional diameter (CSD) of the vastus intermedius and the rectus femoris of the quadriceps muscle. The right rectus femoris and right vastus intermedius CSD decreased in both groups (EMS group: from 1.42 ± 0.48 to 1.31 ± 0.45 cm, p= 0.001 control group: from 1.59 ± 0.53 to 1.37 ± 0.5 cm, p= 0.002; EMS group: from 0.91 ± 0.39 to 0.81 ± 0.38 cm, p= 0.001 control group: from 1.40 ± 0.64 to 1.11 ± 0.56 cm, p= 0.004, respectively). However, the CSD of the right rectus femoris decreased significantly less in the EMS group (-0.11 ± 0.06 cm, −8 ± 3.9%) as compared to the control group (−0.21 ± 0.10 cm, −13.9 ± 6.4%; p< 0.05) and the CSD of the right vastus intermedius decreased significantly less in the EMS group (−0.10 ± 0.05 cm, −12.5 ± 7.4%) as compared to the control group (−0.29 ± 0.28 cm, −21.5 ± 15.3%; p< 0.05). These results are matching with our results although the method of assessment was different – MRCS as a clinical score in our study versus ultrasound as a radiological assessment in Gerovasili study – but both studies showed evidence of deterioration in the muscle status of both groups by time but this was more pronounced significantly in the group of patients who did not receive the EMS sessions (control group).
A randomized controlled trial was done by BourjeilyCitation25 using trans-cutaneous electrical muscle stimulation (TCEMS) of the lower extremities in 18 medically stable patients of mean (SD) age of 60.0 (1.5) years. Stimulation of the lower extremities was performed three times a week, 20 min each session, for six continuous weeks. Quadriceps and hamstring muscle strength, exercise capacity, and peak oxygen uptake were measured at baseline and after 6 weeks of stimulation. TCEMS improved both the quadriceps strength (by 39.0 (20.4)% v 9.0 (8.1)%, p = 0.046) and hamstring muscle strength (by 33.9 (13.0)% v 2.9 (4.7)%, p = 0.038) in the treated (n = 9) and non-treated (n = 9) groups, respectively. The improvement in muscle strength carried over to better performance in the shuttle walk test in the treated group (36.1% v 1.6% in the treated and non-treated groups respectively, p = 0.007, Mann–Whitney U test). There was no significant change in lung function, peak workload, or peak oxygen consumption in either group. Muscle stimulation was well tolerated by the patients with no dropouts and better than 95% compliance with the protocol. Comparing the previous study with our study, it could be noticed the same concept that EMS improved the functional status of the skeletal muscles in both studies the main difference was in the degree of improvement which was much more significant in the Bourjeily study which can be attributed to the different protocols applied and different periods of follow up as well as the very limited number in the study, only 18 patients—versus 80 patients in our study—which made the absolute values of these results a matter of question although we agreed with the overall conclusion as it is matching with most of the results done in the same context.
Regarding the weaning of patients from mechanical ventilation in our study, it was not clear whether the EMS sessions had a really significant role in facilitating the weaning process or not as the number of days on mechanical ventilation showed a better outcome on the EMS group versus the control group but the level of statistical significance was very weak (p = 0.048) while the ventilator free survival out of 28 days came to be non-significant between the two groups (p = 0.421).
Our results regarding the weaning are more or less comparable to the study done by RoutsiCitation14 where the duration of mechanical ventilation was shorter for patients assigned to the EMS group compared with patients in the control group (median (range), 7 (2–41) vs. 10 (1–62), days, respectively), however, this difference was barely significant (log rank test, p= 0.07). A theoretical explanation for this possible effect of EMS on weaning had been provided by Routsi study as patients assigned to the EMS group had a shorter duration of weaning as compared with patients assigned to the control group, which is a further indication of the presence of a relation between the limb and respiratory muscle weakness. As has been already mentioned an acute systemic effect has been reported after one EMS session.Citation24 It is possible that the reported systemic effect of EMS acts as an anabolic stimulus to the respiratory muscles as well. Generally speaking the pro-catabolic cytokine environment that characterizes disease states associated with inflammation and the critically ill, due to excessive localized elaboration of pro-inflammatory cytokinesCitation26 may be altered by EMS. A possible role is suggested for IL-6, which reduces insulin-like growth factor 1 production, providing a major mechanism by which chronic inflammation inhibits hormonal anabolic action and affects growth.Citation27 Exercise training reduces IL-6 production as well as the magnitude of the acute exercise IL-6 response and a decreased plasma IL-6 concentration, not only in response to exercise but also at rest, appears to characterize a normal exercise adaptation.Citation28 The same mechanism, affecting muscle protein turnover, could hold true for EMS implementation. The shorter duration of weaning in patients assigned to the EMS group implies a beneficial effect of EMS on the respiratory muscle function and reinforces the clinical significance of this study.
In another study conducted by ChiangCitation5 on the effects of Physical Training on Functional Status in Patients with Prolonged Mechanical Ventilation, the respiratory muscle strength (i.e., Pimax and Pemax) was similar in both groups at baseline. At the third and sixth weeks of the study period, Pimax and Pemax increased significantly (p< 0.01) in the treatment group and decreased significantly (p< 0.001) in the control group compared with baseline. Both Pimax and Pemax were significantly greater in the treatment group than in the control group after 6 weeks of physical training. At the end of the 6-week study period, 8 subjects (47%) in the treatment group and 3 subjects (20%) in the control group were able to be removed from the ventilator for at least 12 h per day. The ventilator-free time increased an average of 8.9 h per day (p< 0 .01) in the treatment group and 4.8 h (p< 0.1) in the control group after 6 weeks compared with baseline.
No further studies done on the use of EMS in critically ill patients investigated the mortality as an endpoint for assessment of the benefit of this technique but it seems quiet logical that minimizing the days of mechanical ventilation and facilitation of rapid weaning will decrease the overall complications and might have a beneficial effect through reducing mortality.
No significant complications were encountered during the usage of EMS; only 6 patients suffered from prickling sensation during and after the EMS sessions but this was not clinically significant to be a reason to stop the sessions. All 40 patients in the EMS group completed their sessions till the end of the study.
Our study findings are limited by the relatively small number and heterogeneity of the patients with critical illness who underwent an EMS session. Furthermore, sedation and the use of drugs such as vasopressors might have affected microcirculation in these patients.
Future studies with larger sample sizes may allow subgroup analysis to distinguish potential beneficial effects of EMS for different patient populations.
7 Conclusions
We can conclude from this study that ICUAMW is a very common finding which can occur very early in the course of mechanically ventilated critically ill patients.
The use of EMS sessions as a passive form of physiotherapy is a safe, cheap and easily applicable technique in ICU as it does not need patient cooperation.
Daily application of EMS sessions could not prevent the occurrence of ICUAMW but it can minimize the degree of weakness as shown from MRCS.
There was a tendency for easier weaning in the EMS group versus the control group but the evidence was not statistically significant in such a relatively small population sample.
Notes
Available online 19 April 2013
Peer review under responsibility of Alexandria University Faculty of Medicine.
References
- N.A.AliJ.M.O’BrienJr.S.P.HoffmannAcquired weakness, handgrip strength, and mortality in critically ill patientsAm J Respir Crit Care Med1782008261268
- B.De JongheT.SharsharJ.P.LefaucheurParesis acquired in the intensive care unit: a prospective multicenter studyJAMA288200228592867
- J.Garnacho-MonteroJ.Madrazo-OsunaJ.L.García-GarmendiaCritical illness polyneuropathy: risk factors and clinical consequences. A cohort study in septic patientsIntensive Care Med27200112881296
- M.A.de LetterP.I.SchmitzL.H.VisserRisk factors for the development of polyneuropathy and myopathy in critically ill patientsCrit Care Med29200122812286
- L.L.ChiangL.Y.WangC.P.WuEffects of physical training on functional status in patients with prolonged mechanical ventilationPhys Ther86200612711281
- C.BurtinB.ClerckxC.RobbeetsEarly exercise in critically ill patients enhances short-term functional recoveryCrit Care Med37200924992505
- G.HermansA.WilmerW.MeerssemanImpact of intensive insulin therapy on neuromuscular complications and ventilator dependency in the medical intensive care unitAm J Respir Crit Care Med1752007480489
- P.BouletreauM.C.PatricotF.SaudinEffects of intermittent electrical stimulations on muscle catabolism in intensive care patientsJ Parenter Enteral Nutr111987552555
- M.PérezA.LuciaSantallaAEffects of electrical stimulation on VO2 kinetics and delta efficiency in healthy young menBr J Sports Med372003140143
- K.OstrowskiT.RohdeM.ZachoEvidence that interleukin-6 is produced in human skeletal muscle during prolonged runningJ Physiol5081998949953
- L.HiroseK.NosakaM.NewtonChanges in inflammatory mediators following eccentric exercise of the elbow flexorsExerc Immunol Rev1020047590
- H.TsuchimochiS.G.HayesJ.L.McCordBoth central command and exercise pressor reflex activate cardiac sympathetic nerve activity in decerebrate catsAm J Physiol Heart Circ Physiol296200911571163
- S.Pimenta AdaR.H.LambertucciR.GorjãoEffect of a single session of electrical stimulation on activity and expression of citrate synthase and antioxidant enzymes in rat soleus muscleEur J Appl Physiol1022007119126
- Christina RoutsiVasilikiGerovasiliIoannisVasileiadisElectrical muscle stimulation prevent critical illness poly neuromyopathy, a randomized parallel intervention trialCrit care142010118120
- B.De JongheS.Bastuji-GarinT.SharsharDoes ICU-acquired paresis lengthen weaning from mechanical ventilation?Intensive Care Med30200411171121
- B.De JongheS.Bastuji-GarinM.C.DurandRespiratory weakness is associated with limb weakness and delayed weaning in critical illnessCrit Care Med35200715
- R.P.KleywegF.G.MechéP.I.SchmitzInterobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndromeMuscle Nerve14199111031109
- D.J.ScheinhornD.C.ChaoM.Stearn-HassenpflugLiberation from prolonged mechanical ventilationCrit Care Clin182002569595
- D.J.ScheinhornD.C.ChaoM.S.HassenpflugD.R.GraceyPost-ICU weaning from mechanical ventilation: the role of long-term facilitiesChest1202001482484
- F.IndiharA 10-year report of patients in a prolonged respiratory care unitMinn Med7419912327
- A.ModawalN.P.CandadaiK.M.MandellWeaning success among ventilator-dependent patients in a rehabilitation facilityArch Phys Med Rehabil832002154157
- A.CombesM.A.CostaJ.L.TrouilletMorbidity, mortality, and quality-of-life outcomes of patients requiring 14 days of mechanical ventilationCrit Care Med31200313731381
- U.J.MartinWhole-body rehabilitation in long-term ventilationRespir Care Clin N Am82002593609
- V.GerovasiliK.StefanidisK.VitzilaiosE.KaratzanosP.PolitisA.KoroneosElectrical muscle stimulation preserves the muscle mass of critically ill patients: a randomized studyCrit Care132009161
- G.Bourjeily-HabrC.L.RochesterF.PalermoP.SnyderV.MohseninRandomized controlled trial of transcutaneous electrical muscle stimulation of the lower extremities in patients with chronic obstructive pulmonary diseaseThorax57200210451049
- M.J.RennieAnabolic resistance in critically ill patientsCrit Care Med372009398399
- F.De BenedettiT.AlonziA.MorettaD.LazzaroP.CostaV.PoliInterleukin 6 causes growth factor impairment in transgenic mice through a decrease in insulin like growth factor-I. A model for stunted growth in children with chronic inflammationJ Clin Invest991997643650
- C.P.FischerInterleukin 6 in acute exercise and training: what is the biological relevanceExerc Immunol Rev122006633
