Abstract
Introduction
Postoperative radiotherapy of the parotid gland could be achieved with various radiotherapy techniques. However they irradiate differently the surrounding organs at risk (OARs) in particular the cochlea, oral cavity & contralateral parotid causing significant increase in the risk of oral mucositis, xerostomia, and hearing deficits on the irradiated side.
Objectives
The aim of this study was to compare radiation doses received by target volume and different surrounding OARs using three different parotid irradiation techniques aiming to achieve the optimum technique which shows adequate target coverage and sparing of surrounding OARs during postoperative 3DCRT treatment of parotid gland cancer patients.
Methodology
Ten patients diagnosed as having parotid cancer were included in this study. They were subjected to CT simulation and scans were transferred to the treatment planning system. Target volumes and contralateral parotid, oral cavity, cochlea, spinal cord, brain stem, eyes, lenses and optic nerves were contoured. Three plans were done using (a) ipsilateral oblique wedged photon pair, (b) oblique wedged photon pair and direct lateral field, and (c) ipsilateral mixed photon electron beams.
For three plans, the dose volume parameters (DVPs) for target volume and surrounding OARs were compared and analyzed statistically.
Results
Target dose coverage was adequate and comparable for techniques 1 and 2. Technique 2 showed the best dose homogeneity and conformity and lowest max dose to PTV and to the whole body and although the dose to OARs was higher compared to technique 1 it was far lower than OARs tolerance. On the other hand, technique 3 showed unaccepted underdose & dose inhomogeneity within the PTV, the highest doses to OARs and the highest PTV max and body max dose.
Conclusion
The ipsilateral oblique wedged photon pair and direct lateral photon field technique is an optimal treatment technique for parotid cancer patients in comparison to other plans.
Abbreviations:
- 3DCRT
- three dimensional conformal radiotherapy
- OARs
- organs at risk
- DVPs
- dose volume parameters
- PTV
- planning target volume
- RT
- radiation therapy
- ACOD
- Alexandria Clinical Oncology Department
- CT
- computed tomography
- ICRU
- International Commission on Radiation Units
- MLCs
- multi-leave collimators
- DVHs
- dose volume histograms
- TPS
- treatment planning system
- Cont. LC
- contra-lateral cochlea
- ipsi. LC
- ipsilateral cochlea
- C. Parotid
- contralateral parotid
1 Introduction
Parotid gland tumors comprise 3% of all head and neck tumors.Citation1 Radiation therapy (RT) combined with surgery is the main treatment option for patients with adverse pathological risk factors such as high tumor grade, tumor size more than 4 cm, tumor localization within the deep lobe of the parotid, positive surgical margins, lymph node involvement, nerve infiltration, advanced pathological stage, perineural and perivascular invasion, soft tissue extension and recurrent tumor following resection.Citation1,Citation2
Radiation is commonly administered using linear accelerator of 6 MV-energy using three ipsilateral irradiation techniques. The first technique involves a pair of oblique wedged photon beams, the second uses a pair of oblique wedged photon beams and a direct lateral field and the third technique uses mixed photons and electron beams.Citation1
The treatment volume generally includes the ipsilateral parotid bed and the upper neck nodes.Citation1 Presence of regions of different physical and electron densities such as air cavity, dense bone and soft tissue create internal inhomogeneity. Presence of this inhomogeneity with an irregular surface of the volume due to presence of the external ear, both create a heterogeneous treatment volume and so dose distribution; for example tumor might be underdosed due to a decrease in the range of electron beams in the presence of dense bone, and critical structure might be overdosed due to increased penetration of photon beams in the presence of an air cavity.Citation1–Citation3
Although post operative radiotherapy improves locoregional control, different acute and late radiotherapy-related toxicities have been described. These include oral mucositis, xerostomia, dry ear, ear infections, hearing deficits and ipsilateral hearing loss on the irradiated side.Citation1–Citation6 These toxicities could be related to different factors such as radiotherapy technique, size of treatment field, total dose and dose/fraction.Citation6,Citation7
Choice of radiotherapy technique is the most important factor that affects toxicities. Various radiotherapy techniques have been described; the most commonly used one is a pair of oblique wedged photon beams which produce a low radiation dose to the contra-lateral parotid gland, but have a high exit dose through the oral cavity, brain-stem, spinal cord, and the cochlea.Citation3–Citation5 The second most common radiotherapy technique is ipsilateral two oblique wedged and direct lateral photon fields which show the best dose homogeneity and conformity but it shows high dose to OARs which is far lower than OARs tolerance. The third technique is the mixed photon electron beam which uses a high energy electron beam of 12–20 MeV and a low energy photon beam of 6 MV, this technique is usually associated with high dose to the contra-lateral parotid gland, skin and mandible, and a more inhomogeneous tumor dose distribution.Citation4,Citation5
So different radiotherapy techniques should be evaluated and compared according to which of them produces adequate target coverage and at the same time reduces the absorbed dose to surrounding OARs as the cochlea, oral cavity, brain stem, spinal cord, contralateral parotid and other normal tissues below their tolerance to reduce the occurrence of oral mucositis, xerostomia, infections, and sensorineural hearing loss on the irradiated side.Citation8 Based on the published data on OARs tolerance and occurrence of toxicities; to avoid the occurrence of xerostomia, the mean dose to contralateral parotid should not exceed 24–26 Gy and the mean dose to the oral cavity also should be around 35 Gy,Citation9 and to avoid sensorineural hearing loss, the mean cochlear dose should not exceed 40 Gy.Citation10,Citation11
2 Aim of work
The aim of this study was to compare radiation doses received by target volume and different surrounding OARs using three different parotid irradiation techniques aiming to achieve optimum technique which shows adequate target coverage and sparing of surrounding organs at risk (OARs) during postoperative 3DCRT treatment of parotid gland cancer patients.
3 Methods
The material of this study included ten patients diagnosed as having parotid cancer, who underwent superficial parotidectomy and were referred to the Alexandria Clinical Oncology Department (ACOD), Alexandria faculty of Medicine for postoperative radiotherapy to the parotid bed. All the patients had at least one indication for post-operative radiotherapy (high-grade histology, inadequate surgical margin, presence of perineural invasion and nodal disease). All patients were immobilized using individual thermoplastic head masks with thermoplastic shoulder fixation and had computed tomography (CT) simulation (3 mm slice thickness). The CT data were transferred to the treatment planning system (Precise Elekta).
Target volumes and OARs contouring and dose prescription were performed according to the International Commission on Radiation Units (ICRU) 62 guidelines.Citation12 Planning target volume (PTV) and surrounding OARs including contralateral parotid, oral cavity, ipsilateral & contralateral cochlea, spinal cord, brain stem, eyes, lenses and optic nerves were contoured. For each patient, three plans were done;
Plan 1: ipsilateral pair of oblique wedged 6 MV photon beams was used; a wedge angle of 35–60° was used. The beam weight was about 80–100%. No collimation or couch rotation was used. Because of the superficial position of the parotid bed, a bolus of 1–1.5 cm thickness was used in both fields to improve target coverage in the build up region.
Plan 2: ipsilateral pair of oblique wedged 6 MV photon beams and direct lateral photon field were used; a wedge angle of 60° was mostly used for oblique fields. In some patients a wedge was added to the lateral field with a thick end inferior to compensate for the hot spot produced by an air gap at the inferior part of the field (caudal). For the lateral field, beam weight was about 50–70%. No collimation or couch rotation was used. A bolus of 1–1.5 cm thickness was used in all fields. Gantry angle, wedge angle, and beam weighting were adjusted for each patient.
Plan 3: ipsilateral mixed photon electron beams were used. An ipsilateral 6 Mv open photon beam, with 1-1.5cm bolus was used and 15 Mev electron beam was delivered. Both beams were equally weighted. Regarding field size; for oblique fields the smallest field size was 7X9cm and the largest one was 10X16cm (average=8X11cm). For lateral field the smallest field size was 8X9cm and the largest one was 13X16cm (average=11X11cm). Multi-leaf collimators (MLCs) were used to shape the PTV and to shield the close OARs. For electron beam, field size was defined using 10x10 or 14x 14 applicator according to the size of PTV and lead cut out was used to shape the PTV and to shield the close OAR. A dose of 60 Gy was prescribed to the center of the PTV according to ICRU for plan 1 & 2 and in plan 3 it was prescribed at D max for electron beam and at 3-4cm depth for photon beam.
For all plans, isodose distributions and dose volume histograms (DVH) were generated. Plan comparison depends on dose coverage of PTV, its conformity, dose homogeneity within PTV, body maximum dose and the sparing of OARs. The coverage of PTV was evaluated using the minimum and maximum dose. Dose inhomogeneity percentage within PTV was calculated for all patients by subtracting the minimum from the maximum dose of the PTV. Sparing of OARs was assessed using the mean dose for contralateral parotid, cochlea & oral cavity & the maximum point dose of the spinal cord, brain stem, lenses, and optic nerves were also compared.
3.1 Statistical analysis
For all patients, DVPs were recorded. The differences and % of reduction of the DVPs between the plans were calculated and analyzed statistically using excel sheet 2003 and SPSS Wilcoxon signed Rank test (version18).
4 Results
By reviewing the DVPs of the three treatment plans of all patients, the followings are the results as regards the dose distribution of the PTV and OARs including contralateral parotid, spinal cord, brain stem, both cochlea, oral cavity, and body max dose ( & and ):
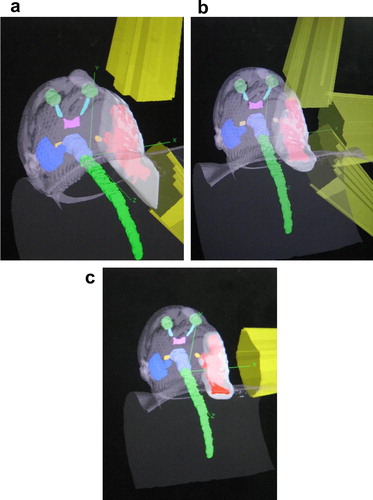
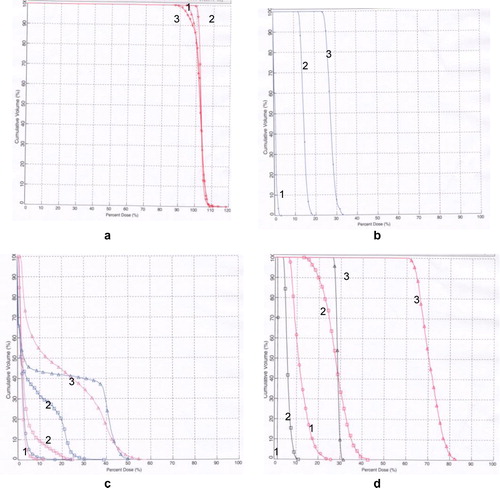
Table 1 Comparison of the average of DVPs of PTV, contralateral parotid, spinal cord, brain stem, contra lateral and ipsi-lateral cochlea, oral cavity DVPs and body max dose irradiated by three different techniques for parotid cancer patients (all are in %). P values for the differences between the plans are also shown.
gives the statistical analysis and DVPs for PTV and OARs comparing the three plans.
4.1 Plan 1 & 2
PTV coverage (PTV min) is adequate and comparable for both plans while the maximum dose and dose inhomogeneity are significantly better with plan 2. Regarding OAR sparing, plan 1 shows a reduction of all DVPs compared with plan 2, however this reduction is insignificant for some of DVPs. Plan 2 also shows a significant reduction of 3% in body max dose.
4.2 Plan 1 & 3
PTV coverage (PTV min), the maximum dose and dose inhomogeneity of plan 1 are significantly better than plan 3. Regarding OAR sparing, plan 1 shows a significant reduction of all DVPs compared with plan 3 except for the oral cavity mean dose which shows insignificant reduction with plan 1. Plan 1 also shows a significant reduction of 3% in body max dose.
4.3 Plan 2 & 3
PTV coverage (PTV min), the maximum dose and dose inhomogeneity of plan 2 are significantly better than plan 3. Regarding OAR sparing, plan 2 shows a significant reduction of all DVPs compared with plan 3 except for the oral cavity mean dose which was comparable for both plans. Plan 2 also shows a significant reduction of 7% in body max dose.
To summarize, the three techniques were compared regarding target coverage, conformity, dose homogeneity within PTV, OARs sparing and body max dose. For techniques 1 & 2 the target coverage was adequate and comparable (). Although the dose to OARs of the technique 1 was lower compared to technique 2, the plan was not conformal and shows unaccepted dose inhomogeneity within the PTV () and higher max dose to PTV and to the body.
Technique 2 showed adequate target coverage with the best dose homogeneity and conformity (95% of the dose completely covers the PTV and closely matches its shape) () compared to the other two techniques and the lowest max dose to PTV and to the whole body. Although the dose to OARs was higher compared to technique 1, it was significant only for contralateral parotid and contralateral cochlea; also their values were far lower than OARs tolerance.
Technique 3 showed unaccepted underdose & dose inhomogeneity within the PTV (), the highest doses to OARs and the highest PTV & body max. dose. DVHs for a typical patient are shown in and show the differences in irradiation of the PTV and different OARs with the different techniques. As the doses to the eyes, lenses and optic nerves are very low and comparable for all patients we did not list them in the table.
5 Discussion
Postoperative radiotherapy using different techniques, radiation sources and beam energies is an effective treatment in patients with parotid tumors especially when 3D treatment planning system (TPS) is used. TPS helps in providing an optimal treatment plan for individual patients with more realistic dose distributions; adequate dose target volume coverage and sparing of the surrounding OARs.Citation1 This could improve local tumor control and reduce the normal organs toxicity thereby preserving maximum quality of life after radiation therapy.Citation1
In the current study, the resulting isodose distributions of the three plans showed different degrees of dose coverage, inhomogeneity, hot spot and the dose to the normal structures; the mixed electron–photon beam techniques contributed to lowest dose coverage, highest dose heterogeneity, highest hot spot and highest OARs doses compared to other photon techniques. The results of the current study are in accordance with Yaparpalvi et al’s.Citation1 work who performed a dosimetric analysis of different techniques, among them were the ipsilateral wedge photon pair, ipsilateral wedge photon pair with a lateral photon field, and the mixed electron–photon beam techniques. They found that the resulting isodose distributions of the three plans exhibited different degrees of dose inhomogeneity, hot spot and the dose to the normal structures; the mixed electron–photon beam technique contributed to highest dose heterogeneity, highest OARs doses compared to other photon techniques. They explained that the beam obliquity, surface irregularity, and tissue heterogeneity all modify the beam penetration and depth dose characteristics for electron beams more than for photon beams.Citation1
In the current study, ipsilateral wedge photon pair with lateral photon field showed adequate target coverage with the best dose homogeneity and conformity compared to the other two techniques and the lowest max dose to PTV and to the whole body, although the dose to OARs was higher compared to the ipsilateral wedge photon pair technique but it was far lower than OARs tolerance. These results are also in agreement with Yaparpalvi et al’s.Citation1 work. However in the current study the hot spot was far lower than they achieved (115%, 111% & 119% against 120%, 115% & 120–140% in their study) for the three plans respectively. These differences might be attributed to the difference of the beam weighting and the difference in the depth of the prescription dose.
Regarding OARs, in both studies, contralateral parotid mean dose, spinal cord and brain stem max dose were the lowest with the ipsilateral wedge photon pair followed by the ipsilateral wedge photon pair and lateral field and were the highest with the mixed electron–photon beam technique.
As the available published data were about radiotherapy of parotid gland use mainly the ipsilateral wedged photon pair we will use it for comparison with our plans. In the current study, for PTV dose coverage; the average of minimum dose to PTV was 57 Gy (94.5%) and the average of maximum dose was 68 Gy (113%). In Nutting et al’s.Citation5 study the min dose to the PTV was 55 Gy (91%) and the maximum dose was 62.8 Gy (105%). Compared to plan 2, the average of minimum dose to PTV was 57 Gy (95%) and the average of maximum dose was 66 Gy (109.5%), for plan 3, the average of minimum dose to PTV was 48 Gy (80%) and the average of maximum dose was 72 Gy (120%). Nutting et al.Citation5 and Yirmibesoglu et al’s.Citation13 studies found the percentage of the dose inhomogeneity was 13% & 30% respectively compared to 18.5%, 14.5% & 40% for the three plans in our work respectively.
In the present work using an oblique wedged pair:
The average of the mean dose to the oral cavity was 33 Gy which is much higher than the mean dose to the oral cavity (23 Gy) in the study done by Nutting et al.Citation5 (using a wedged pair).
The mean dose to the contralateral parotid was 0.4 Gy which is much lower than the mean dose in the study done by Nutting et al.Citation5 (1.6 ± 0.7 Gy) and Yirmibesoglu et al.Citation13 (2.4 Gy) (both used wedged pair technique).
In spite of the higher radiation dose to the oral cavity (37 Gy & 37 Gy) and the contralateral parotid gland (8 Gy & 19 Gy) in the current study using plan 2 & 3, our results were still below the tolerance dose that causes xerostomia, which was determined by Eisbruch et al.Citation14,Citation15 to be 24–26 Gy to the contralateral parotid gland, and given by Studer et al.Citation9 to be 35 Gy to spare the oral mucosa.
The mean doses to ipsilateral & contralateral cochlea in the present study, were (13 Gy & 0.6 Gy,) respectively. These values were far lower than those achieved by Nutting et al.Citation5 for the ipsilateral cochlea (42.3 Gy) & by Yirmibesoglu et al.Citation13 for the contralateral cochlea (4.8 Gy).
Although the values of the mean dose to the ipsilateral cochlea (Gy16 & 32 Gy) & the contralateral cochlea (4 Gy & 13 Gy) in the present study for plan 2 & 3 were higher than for plan 1, these values were still under the threshold that cause sensorineural hearing loss which ranges between 30 Gy and 70 Gy.Citation16,Citation17
In the present work the maximum point dose to the brain stem was far lower than achieved by Nutting et al.Citation5 (20 Gy in the present work compared to 27.4 Gy in his study)
Although the max point dose to the brain stem in the present study for plan 2 & 3 was higher than that for plan 1 (22 Gy & 34 Gy) these values were still below its tolerance (54 Gy)
So this study presented the details of dosimetric analysis among three plans used for postoperative radiotherapy of the parotid gland, however the impact of radiotherapy technique-related DVPs on patient outcome and toxicity should be analyzed in future work.
6 Conclusion
Based on dose distributions, this study concluded that the ipsilateral oblique wedged photon pair and direct lateral photon field technique is better in comparison to other techniques for parotid cancer patients.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 17 June 2013
References
- R.YaparpalviD.P.FontenlaS.K.TyerechL.R.BoselliJ.J.BeitlerParotid gland tumors: a comparison of postoperative radiotherapy techniques using three dimensional (3D) dose distributions and dose-volume histograms (DVHS)Int J Radiat Oncol Biol Phys40119984349
- D.AlterioB.A.Jereczek-FossaM.GriseriA.D’OnofrioG.GiuglianoM.R.FioreThree-dimensional conformal postoperative radiotherapy in patients with parotid tumors: 10 years’ experience at the European Institute of OncologyTumori9732011328334
- R.J.KudchadkerAntolakW.H.MorrisonP.F.WongK.R.HogstromUtilization of custom electron bolus in head and neck radiotherapyJ Appl Clin Med Phys442003321333
- A.M.ChenP.J.GranchiJ.GarciaLoco-regional recurrence after surgery without post-operative irradiation for carcinoma of the major salivary gland: implications for adjuvant therapyInt J Radiat Oncol Biol Phys672007982987
- Christopher M.NuttingCarl G.RowbottomVivian P.CosgroveOptimization of radiotherapy for carcinoma of the parotid gland: a comparison of conventional, three-dimensional conformal and intensity-modulated techniquesRadiother Oncol6022001163172
- A.S.GardenA.K.El NaggerW.H.MorrisonD.L.CallenderK.King AngL.J.PetersPostoperative radiotherapy for malignant tumors of the parotid glandInt J Radiat Oncol Biol Phys3719977985
- C.H.TerhaardH.LubsenC.R.RaschP.C.LevendagH.H.KaandersR.E.Tjho-HeslingaDutch Head and Neck Oncology Cooperative Group: the role of radiotherapy in the treatment of malignant salivary gland tumorsInt J Radiat Oncol Biol Phys612005103111
- I.J.SpiroC.C.WangW.W.MontgomeryCarcinoma of the parotid gland: analysis of treatment results and patterns of failure after combined surgery and radiation therapyCancer71199326992705
- G.StuderP.U.HugueninJ.B.DavisG.KunzU.M.LütolfC.GlanzmannIMRT using simultaneously integrated boost (SIB) in head and neck cancer patientsRadiat Oncol1200617
- R.P.SymondsR.A.EvansK.C.LiuT.AzharLate audio-vestibular consequences of radical radiotherapy to the parotidClin Oncol431992203204
- Y.P.TalmiY.FinkelsteinY.ZoharPost-irradiation hearing lossAudiology281989121126
- International Commission on Radiation Units and Measurements: Prescribing, recording and reporting photon beam therapy. ICRU Report 62. Bethesda, Maryland, USA; 1999.
- EdaYirmibesogluDosimetric evaluation of an ipsilateral intensity modulated radiotherapy beam arrangement for parotid malignanciesInt J Radiat Oncol Biol Phys8122011S527S528
- A.EisbruchR.K.Ten HakenH.M.KimL.H.MarshJ.A.ShipDose, volume, and function relationships in parotid salivary glands following conformal and intensity-modulated irradiation of head and neck cancerInt J Radiat Oncol Biol Phys451999577587
- E.D’HondtA.EisbruchJ.A.ShipThe influence of pre-radiation salivary flow rates and radiation dose on parotid salivary gland dysfunction in patients receiving radiotherapy for head and neck cancersSpec Care Dent181998102108
- B.A.Jereczek-FossaE.RondiA.ZarowskiA.D’OnofrioD.AlterioM.CioccaProspective study on the dose distribution to the acoustic structures during postoperative 3D conformal radiotherapy for parotid tumors: dosimetric and audiometric aspectsStrahlenther Onkol18762011350356
- S.A.BhideK.J.HarringtonC.M.NuttingOtological toxicity after postoperative radiotherapy for parotid tumoursClin Oncol (R Coll Radiol)19120077782