Abstract
Background
Dyspepsia is a common clinical problem. More than half of patients presenting with dyspepsia have no detectable lesion for their symptoms. The common organic causes of dyspepsia include peptic ulcer, esophagitis and cancer. The diagnostic test of choice is endoscopy. Age specific thresholds to trigger endoscopic evaluation may differ by gender, availability of resources and regional disease specific risks.
Aim
The aim of the study was to determine the prevalence of significant endoscopic lesions in Egyptian patients presenting with dyspepsia in relation to age.
Materials and methods
This was a retrospective study. Data on patients presenting with dyspepsia and scheduled for upper gastrointestinal (UGI) endoscopy between January 2000 and January 2013 were collected.
Results
One thousand four hundred patients with dyspepsia (31% of all endoscopies) were assessed by UGI endoscopy. Fifty-one percent were male. The mean age was 43 ± 15 years. Four hundred and fifty patients (32%) had a history of smoking, 388 (32%) were taking aspirin or non-steroidal anti-inflammatory drugs and 22 (2%) were consuming alcohol. Endoscopy revealed normal findings or miscellaneous irrelevant findings in 913 patients (65%). Significant endoscopic findings were diagnosed in 487 (35%). These included peptic ulcers in 245 patients (18%), esophagitis in 191 (14%), erosive gastroduodenitis in 112 (8%) and UGI malignancy in 16 (1%). Significant endoscopic findings were associated with increasing age.
Conclusion
Dyspepsia is a common indication for endoscopy in Egypt. Endoscopy revealed normal findings or miscellaneous irrelevant findings in the majority of patients. The most frequent significant pathologies included peptic ulcer, esophagitis and erosive gastroduodenitis. These were associated with increasing age. UGI malignancy was uncommon and found in older age groups.
Keywords:
1 Introduction
Dyspepsia is defined as pain or discomfort in the upper abdomen.Citation1 It is a common disorder with a prevalence of up to 40% in the general population in Great Britain.Citation2 More than half of these patients presenting with dyspepsia have no detectable cause for their symptoms.Citation1 The common organic causes of dyspepsia are peptic ulcer, esophagitis and cancer.
Options for evaluating dyspeptic patients include therapeutic trials, testing for Helicobacter pylori, upper gastrointestinal (UGI) radiography, and endoscopy.Citation3–Citation5 Once the decision has been made to investigate, the diagnostic test of choice is endoscopy.Citation1 Patients in whom investigations have revealed no organic cause are classified as having functional dyspepsia or “non-ulcer dyspepsia”.Citation6
Cancer of the UGI tract is usually advanced at the time of diagnosis but a low threshold of suspicion for gastric malignancy in dyspeptic patients may result in earlier diagnosis and improved survival. However cancer accounts for only 1–2% of diagnoses at UGI tract and less in patients under the age of 50 years.Citation7 Age specific thresholds to trigger endoscopic evaluation may differ by gender, availability of resources and regional disease specific risks.Citation8
This study was undertaken to determine the prevalence of significant endoscopic lesions in Egyptian patients presenting with dyspepsia in relation to age.
2 Materials and methods
This was a retrospective study carried out at Bolak Eldakror Hospital over a 13-year period from January 2000 to January 2013. Bolak Eldakror Hospital is a secondary-care governmental hospital in Giza, Egypt. The hospital serves an area of nearly one million population. The gastrointestinal endoscopy unit was set up in 1999. The endoscopy unit provides an open-access service and receives patients from outpatient clinics and other hospitals in the area. Patients are from a lower socioeconomic background. All patients presenting with dyspepsia were included in the study. Ten gastroenterologists performed all endoscopies. Two UGI fiberscopes and two videoscopes (Olympus GIF-E and GIF-Q230) were used. Endoscopic biopsy was done at the discretion of the endoscopist. Pathological examination was performed by two expert pathologists.
2.1 Definitions
Dyspepsia was defined as epigastric discomfort, burning sensation or pain persisting for more than three months.Citation9 Heartburn is not included in the diagnostic symptom criteria for dyspepsia. It is thought to arise primarily from the esophagus being caused by gastro-esophageal reflux disease although it may occur concomitantly with dyspeptic symptoms.Citation8
Significant endoscopic findings in the UGI tract were defined as those benefiting from specific treatment or those that are life threatening.Citation10 The presence of any of the following lesions was considered as a significant finding in UGI endoscopy: peptic ulcer, esophagitis (with or without hiatal hernia), erosive gastritis or duodenitis, stricture, Barrett’s esophagus, esophageal candidiasis, neoplasm, mass and polyps.
Reflux esophagitis was graded according to the Savary–Miller grading.Citation11,Citation12 Stage I: Erythematous or erythemato-exudative erosion (alone or multiple, not confluent). Stage II: confluent but not circumferential erosion. Stage III: circumferential erosive and exudative lesions. Stage IV: chronic lesions (ulcer, stenosis). The presence of any of the following lesions was considered as an irrelevant endoscopic finding: erythematous gastritis, atrophic gastritis and incidental miscellaneous abnormalities (varices, portal hypertensive gastropathy, hiatal hernia without esophagitis and vascular ectasia).
2.2 Patients and exclusions
A total of 4477 patients underwent UGI endoscopy between January 2000 and January 2013. Data on patients presenting with dyspepsia and scheduled for UGI endoscopy were collected. Patients who underwent UGI endoscopy for reasons other than dyspepsia such as dysphagia, UGI bleeding, or strong suspicion of cancer were excluded from the study. Patients with prior peptic ulcer were also excluded. Those whose procedures were not completed were excluded subsequently.
2.3 Data recording and statistics
Patients were stratified into three groups according to their age: less than 30 years (group 1), 30–50 years (group 2) and more than 50 years (group 3).Citation1
A standardized data collection form (sheet) was completed for each patient. Recorded information included demographic data (age and gender), smoking history, drugs used (aspirin and non-steroidal anti-inflammatory) alcohol consumption, associated heartburn, endoscopic findings and histopathology. Data were analyzed to assess a statistically significant difference between the age groups for various gastrointestinal lesions. The data from the patients were registered, tabulated and statistically analyzed using the Statistical Package for Social Sciences (SPSS) program version 15 to calculate frequencies and the χ2 test. P value was taken as significant at a level less than 0.05.
3 Results
One thousand four hundred patients presenting with dyspepsia were assessed. Dyspepsia was the commonest indication for UGI endoscopy (). Percentage of patients with dyspepsia who underwent UGI endoscopy among the studied years ranged from 19% to 56% (mean 31 ± 13).
Table 1 Indications for UGI endoscopy among studied years.
3.1 Patients’ characteristics
Seven hundred and seven patients (51%) were male and 693 (49%) female. Ages ranged from 18 to 88 years, mean 43 ± 15 years. Four hundred and fifty patients (32%) had a history of smoking, 388 (32%) were taking aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) and 22 (2%) were consuming alcohol. One hundred and eighty-three patients (13%) had associated heartburn. Patients’ characteristics stratified by age are presented in .
Table 2 Patients’ characteristics stratified by age.Table Footnote⁎
3.2 Endoscopic findings
Endoscopy revealed normal findings or miscellaneous irrelevant findings in 913 patients (65%). Endoscopy revealed significant pathology in 487 patients (35%). Peptic ulcer was diagnosed in 245 patients (18%), duodenal ulcers in 206 (15%) and gastric ulcers in 57 (4%). Esophagitis was diagnosed in 191 patients (14%), stage I in 183 (96%), stage II in six (3%) and stage III in two (1%). Esophagitis was diagnosed in 33 patients (18%) who had dyspepsia with heartburn and in 158 patients (13%) without heartburn (P > 0.05, non-significant). Grading of esophagitis in patients with and without heartburn is shown in . Erosive gastritis and/or duodenitis were diagnosed in 112 patients (8%), gastric erosions in 60 (4%) and duodenal erosions in 67 (5%). Gastric malignancy was diagnosed in 15 patients (1%) and duodenal cancer in one (0.1%). Histopathology revealed adenocarcinoma in seven patients (44%), anaplastic carcinoma in three (19%), undifferentiated carcinoma in three (19%), mucoid carcinoma in one (6%), lymphoma in one (6%) and malt lymphoma in one (6%). Esophageal candidiasis was diagnosed in nine (0.6%) patients, gastric polyps (hyperplastic) in six (0.4%), Barrett’s esophagus (4 confirmed by pathology) in five (0.4%), esophageal stricture in two (0.1%) and submucosal mass (leiomyoma) in one (0.1%). Many patients had more than one lesion. Biopsies were obtained for histopathological examination in 37 patients (3%), mainly in patients with suspicion of malignancy (swelling or gastric ulcer), Barrett’s esophagus and polyps. Testing for Helicobacter pylori infection by rapid urease test was performed in 56 patients with gastric or duodenal ulcer (4%) and the test was positive in 29 (52%).
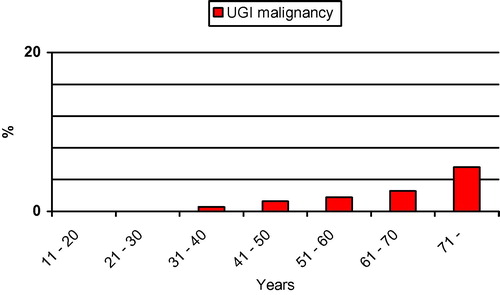
Relative frequency of endoscopic findings in patients presenting with dyspepsia stratified by age is presented in . The prevalence of UGI malignancy among patients with dyspepsia in relation to age is presented in .
Table 3 Endoscopic findings stratified by age.Table Footnote⁎
4 Discussion
Dyspepsia is a common clinical problem seen by both primary care physicians and gastroenterologists. Dyspepsia accounts for about 4–5% of all the general practitioner consultations and 20–40% of all gastroenterological consultations.Citation13 Initial evaluation should focus on the identification and treatment of potential causes of symptoms such as gastro-esophageal reflux disease, peptic ulcer disease, and medication side effects but also on recognizing those at risk for more serious conditions such as gastric cancer. Endoscopy is recommended as the first investigation in the work up of a patient with dyspeptic symptoms and is essential in the classification of the patient’s condition as organic or functional dyspepsia. Approximately 40% of dyspeptic patients have an organic cause, and only 20% of patients have significant gastroduodenal lesions, such as peptic ulcer.Citation10,Citation14,Citation15 The most commonly reported major endoscopic abnormalities are: gastric ulcer (1.6–8.2%), duodenal ulcer (2.3–12.7%), esophagitis (0–23.0%), and gastric malignancy (0–3.4%).Citation16 Only in a few cases are dyspeptic symptoms caused by gastro-esophageal malignancy.Citation17 While gastric or esophageal cancer is an unusual finding in patients with dyspepsia, excluding malignancy is a common reason given for performing endoscopy.Citation8 Once an organic cause for symptoms has been excluded, a diagnosis of functional dyspepsia can be made.Citation8
In the present study 1400 patients presenting with dyspepsia at a community hospital over a 13-year period were assessed. Our goal was to describe patients’ characteristics and endoscopic findings among patients with dyspepsia. We focused on the etiology of dyspepsia in relation to age.
Dyspepsia was the commonest indication for UGI endoscopy in our institution (31% of all endoscopies). The relative frequencies of upper endoscopic finding stratified by age demonstrated that non-ulcer dyspepsia and significant lesions (peptic ulcer, esophagitis and erosive gastroduodenitis) were common in all age groups (). Peptic ulcer, esophagitis and erosive gastroduodenitis were associated with increasing age (). UGI malignancy was an uncommon finding and found in older age groups (). The low prevalence of serious lesions in young patients is consistent with prior published data.Citation18–Citation20 The number of patients with other significant lesions (esophageal candidiasis, gastric polyps (hyperplastic), Barrett’s esophagus, esophageal stricture and leiomyoma) is too small for meaningful comparison.
Endoscopy revealed normal findings or miscellaneous irrelevant findings in 65% of patients presenting with dyspepsia and 82% of patients younger than 30 years. The findings of the present study confirmed that the majority of patients with dyspepsia had no important endoscopic lesions. Many dyspeptic patients continue to be sent for endoscopic evaluation as the initial step in management. The findings of the present study support selective UGI endoscopy in patients with dyspepsia because the prevalence of important lesions was very low in young patients. Further study is warranted to determine whether young patients with dyspepsia benefit from endoscopy. Unmeasured benefits could include improvement in quality of life, if anxiety is reduced, and reduction in subsequent health care utilization.
Significant pathology was diagnosed in 35% of patients presenting with dyspepsia. The commonest included peptic ulcer, esophagitis and erosive gastroduodenitis which were diagnosed in 18%, 14% and 8% of patients, respectively. These findings were more frequent among the older age groups than in the younger age group (P = 0.000, 0.002 and 0.012, respectively). Esophagitis was more common in those with reflux symptoms than in those without (18% vs. 13%) (P > 0.05, non significant). Esophagitis was of mild grade in patients presenting without reflux symptoms ().
We have detected 16 (1%) patients with UGI malignancy among patients with dyspepsia. Ages ranged from 37 to 75 years. UGI malignancy was diagnosed in 1% of patients aged 30–50 years and 2% of patients more than 50 years (P = 0.003). UGI malignancy was not found in dyspeptic patients younger than 30 years old. Studies showed the incidence and risk of gastric malignancy steadily increase with age after 40 years with its highest peak in the seventh decade.Citation21 suggests the same pattern in our sample. No cases of esophageal cancer were reported in this study because most patients with esophageal cancer initially present with dysphagia and these patients were excluded from the study. All cases with UGI malignancy were referred to the National Cancer Institute for further management but unfortunately majority was diagnosed at an advanced stage (unpublished). The factors responsible for delay in detection are underuse of diagnostic tests, late referrals for UGI endoscopy, misdiagnosis and injudicious use of acid suppression therapy. Perhaps the most important reason for performing diagnostic endoscopy is to detect gastric cancer at an early stage. However, in its early stage, gastric cancer presents with symptoms that are often indistinguishable from those of benign gastric ulceration; therefore, all patients who are in the age group at risk of gastric cancer should undergo early endoscopy rather than trials of medical therapy that may delay diagnosis.Citation22
Testing for Helicobacter pylori infection was performed in 56 patients with gastric or duodenal ulcer (4%) and the test was positive in 29 (52%). The number of patients assessed for Helicobacter pylori infection was very small for meaningful comparison. It was reported that the prevalence of Helicobacter pylori infection in Egypt is 90%.Citation23 One study showed that the seroprevalence of Helicobacter pylori infection in Cairo is 60%, Alexandria 88%, Assiut (urban) 87% and Assiut (rural) 40%.Citation24
The findings of the present study confirmed that the majority of patients with dyspepsia had no important endoscopic lesions. The significant endoscopic lesions were more frequent among the older age groups than in the younger age group. There was a statistically significant difference between the age groups for the presence of peptic ulcer, esophagitis, erosive gastroduodenitis and UGI malignancy. Our analysis of daily clinical practice provided valuable information as all consecutive patients of a community hospital in Egypt were included. Also the data provide an interesting profile of this group of patients. Limitation of the study included: the study is retrospective, lack of biopsy sampling in all patients, thereby missing microscopic esophagitis, non-erosive reflux disease, histologic gastritis as well as Helicobacter pylori infection. Also alarm symptoms were not assessed.
In conclusion, dyspepsia is a common indication for endoscopy in Egypt. Endoscopy revealed normal findings or miscellaneous irrelevant findings in the majority of patients. The most frequent significant pathologies included peptic ulcer, esophagitis and erosive gastroduodenitis. These were associated with increasing age. UGI malignancy was uncommon and found in older age groups. Patients with recent onset of dyspepsia who are in the age group at risk of gastric malignancy should undergo early endoscopy. Endoscopy can be avoided in most young patients with chronic dyspepsia because the benefits of endoscopy in these patients are uncertain.
Funding
None.
Conflict of interest
None declared.
Acknowledgments
The authors wish to thank Prof. El-Hindawi A. Cairo University and Prof. Akl M. Theodor Bilharz Research institute for their contribution in the pathological examination.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 5 November 2013
References
- A.AkhtarM.ShaheenDyspepsia in African American and hispanic patientsJ Natl Med Assoc962004635640
- J.G.PenstonR.E.PounderA survey of dyspepsia in Great BritainAliment Pharmacol Ther1019968389
- M.H.EbellL.WarbasseC.BrennerEvaluation of the dyspeptic patient: a cost-utility studyJ Fam Pract441997545555
- M.D.SilversteinT.PettersonN.J.TalleyInitial endoscopy or empirical therapy with or without testing for Helicobacter pylori for dyspepsia: a decision analysisGastroenterology1019967283
- A.SonnenbergCost-benefit analysis of testing for Helicobacter pylori in dyspeptic subjectsAm J Gastroenterol91199617731777
- G.R.LockeNonulcer dyspepsia: what it is and what it is notMayo Clin Proc74199910111015
- E.Bolling-SternevaldR.CarlssonC.AalykkeB.V.WilsonO.JunghardH.GliseSelf-administered symptom questionnaires in patients with dyspepsia and their yield in discriminating between endoscopic diagnosesDig Dis202002191198
- R.HarmonD.PeuraEvaluation and management of dyspepsiaTher Adv Gastroenterol320108798
- J.TackN.J.TalleyM.CamilleriG.HoltmanP.J.HuJ.R.MalageladaFunctional gastroduodenal disordersGastroenterology130200614661479
- P.C.ValleR.K.BreckanA.Amin“Test, score and scope”: a selection strategy for safe reduction of upper gastrointestinal endoscopies in young dyspeptic patients referred from primary careScand J Gastroenterol412006161169
- M.SavaryG.MillerL’oesophage: manuel et atlas d’endoscopie1977Editions GassmannSoleure, Switzerland (English edition 1978). [Internet]. Available from: http://www.gastrosource.com/Scientific-Resources/definitions-classifications/1384415?itemId=1384415
- J.B.OllyoC.FontollierE.BrossardF.LangLa nouvelle classification de Savary des oesophagites de refluxActa Endoscopica221992307320
- N.KhanG.ShabbirM.ZarifM.KhattakUpper gastrointestinal endoscopic assessment of patients presenting with dyspepsiaJPMI212007209216
- R.C.SpillerAnorexia, nausea, vomiting, and painBr Med J323200113541357
- R.S.FisherH.P.ParkmanManagement of nonulcer dyspepsiaN Engl J Med339199813761381
- G.TytgatRole of endoscopy and biopsy in the work up of dyspepsiaGut5020021316
- G.MaconiG.ManesG.PorroRole of symptoms in diagnosis and outcome of gastric cancerWorld J Gastroenterol14200811491155
- D.GillenK.E.L.McCollDoes concern about missing malignancy justify endoscopy in uncomplicated dyspepsia in patients aged less than 55?Am J Gastroenterol9419997579
- B.C.DelaneyS.WilsonA.RoalfeL.RobertsV.RedmanA.WearnCost effectiveness of initial endoscopy for dyspepsia in patients over age 50 years: a randomized controlled trial in primary careLancet356200019651969
- C.CangaN.VakilUpper GI malignancy, uncomplicated dyspepsia, and the age threshold for early endoscopyAm J Gastroenterol972002600603
- N.SalkicM.ZildzicE.ZeremM.SmajicA.GegicE.AlibegovicSimple uninvestigated dyspepsia: age threshold for early endoscopy in Bosnia and HerzegovinaEur J Gastroenterol Hepatol2120093944
- A.AxonChronic dyspepsia: who needs endoscopy?Gastroenterology112199713761380
- World Gastroenterology Organisation Global Guidelines. Helicobacter pylori in developing countries, 2010. [Internet]. Available from: http://www.worldgastroenterology.org/assets/downloads/en/pdf/guidelines/11_helicobacter_pylori_developing_countries_en.pdf.
- S.BassilyR.W.FrenckE.W.MoharebT.WierzbaS.SavarinoE.HallSeroprevalence of Helicobacter pylori among EgyptiansAm J Trop Med Hyg6119993740