Abstract
Introduction
The knowledge of the anatomy of greater occipital nerve and its relation to occipital artery is important for the surgeon. Blockage or surgical release of greater occipital nerve is clinically effective in reducing or eliminating chronic migraine symptoms.
Aim
The aim of this research was to study the anatomy of greater occipital nerve (GON) and its relation to occipital artery. Also the use of these anatomical measures in local injection of the greater occipital nerve for treatment of migraine.
Materials and methods
The study was carried out at the Faculty of Medicine, Alexandria University.
The posterior neck and scalp of 25 cadaveric heads were dissected. GON was identified and measured relative to bony landmarks. Delineation of GON and occipital artery relationship was done.
Twenty patients suffering from migraine diagnosed according to International Headache Society (IHS) criteria (HIS 2004) were treated using GON blockade. The landmark for GON injection was based on the anatomical study. Treatment was assessed using the visual analogue scale for migraine pain.
Results
In the anatomical study, the GON was found in all specimens. The diameter of GON was measured at the lower border of inferior oblique, where it pierced SSC, and after its exit from trapezius muscle. The distance between the point where the GON pierced SSC inferior to the external occipital protuberance (EOP) and lateral to the midline was also measured. The GON was parallel to the occipital artery. The distance between GON and occipital artery was measured.
In the clinical study, 20 patients suffering from migraine were treated with 1.5 ml of 0.5% bupivacaine using GON blockade. The landmark for GON injection was based on the anatomical study. For the right GON: the vertical location inferior to EOP ranged from 19.85 mm to 26.9 mm with a mean of 23.1 mm. The lateral location from EOP ranged from 11.03 mm to 14.65 mm with a mean of 13.4 mm.
For the left GON: the vertical location inferior to EOP ranged from 16.89 mm to 29.5 mm with a mean of 22.1 mm. The lateral location from EOP ranged from 10.89 mm to 15.31 mm with a mean of 14.1 mm.
Pain was improved in 70% of patients within the first hour after the first injection. After 1 month, 60% of patients still showed improvement.
Conclusion
The knowledge of the anatomy of greater occipital nerve and its relation to occipital artery is important for the surgeon. Blockage or surgical release of greater occipital nerve is clinically effective in eliminating chronic migraine headache.
1 Introduction
The greater occipital nerve represents the posterior primary ramus of the second cervical spinal nerve. It comes from the larger medial branch of the dorsal ramus of the second cervical nerve. It ascends between inferior oblique and semispinalis capitis, pierces the latter and trapezius near their occipital and is joined by a filament from the medial branch of the third dorsal ramus.Citation1 It supplies sensory innervations to the posterior regions of the scalp.Citation2
The occipital artery arises from the back of the external carotid on a level with the facial artery. The occipital artery emerges from the apex of the posterior triangle and runs with the GON to supply the back of the scalp up to the vertex.Citation3
The greater occipital nerve becomes superficial just inferior to the superior nuchal line and lateral to the occipital protuberance of the skull; at this point, the nerve is positioned medial to the pulse of the occipital artery, approximately one third of the distance from occipital protuberance to the mastoid.Citation4
There is wide variability of headache syndromes treated by (GON) blockade using local injections of steroids, local anaesthetics or a mixture of both.Citation5
Migraine (with its complex cerebral and brainstem mechanisms), cluster headache, occipital neuralgia, cervicogenic headache, whiplash syndrome, and various tension type headaches have shown variable degree of improvement following (GON) blockade.Citation6,Citation7
So the aim of this research was to study the anatomy of greater occipital nerve and its relation to occipital artery. These anatomical measures will be useful in local injection of the greater occipital nerve for treatment of migraine.
2 Materials and methods
2.1 Anatomical study
Twenty five specimens of head and neck were obtained from anatomy department, faculty of medicine, Alexandria University. All specimens were dissected to show the GON and occipital artery.
Measurements were done for GON diameter below the inferior oblique muscle, and where it pierces semispinalis capitis and trapezius muscles. Also the distances between the point where the GON pierces the semispinalis capitis and the external occipital protuberance and between the GON and occipital artery were measured.
The relationships between the GON, semispinalis capitis, aponeurosis of trapezius and the occipital artery were determined.
The points where the GON pierces the semispinalis capitis and trapezius were determined, measured and photographed on the cadavers. All measurements were done on both sides of the specimens using Vernier Swiss caliper. Statistical analyses were performed.
2.2 Clinical study: patients and methods
In this prospective study, 20 patients suffering from migraine diagnosed according to International Headache Society (IHS) criteria (HIS 2004) were treated using GON blockade.
3 Results
3.1 Anatomical results
In all specimens, the GON was found (, –). The GON appeared at suboccipital region at the lower border of inferior oblique muscle (). The diameter of GON at the lower border of inferior oblique was measured (, ).
Figure 1 A photograph of right half of head and neck specimen (posterior view) showing the greater occipital nerve (GON) emerging on the lower border of inferior oblique(IO) muscle in suboccipital triangle before piercing semispinalis capitis(SSC). (RC: rectus capitis minor and major –TR: trapezius).
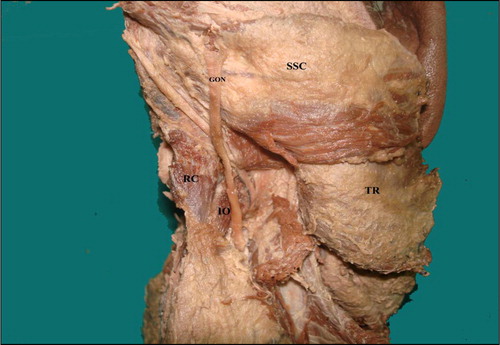
Figure 2 showing the mean diameter of GON at the lower border of inferior oblique muscle and when it pierces semispinalis capitis and trapezius aponeurosis.
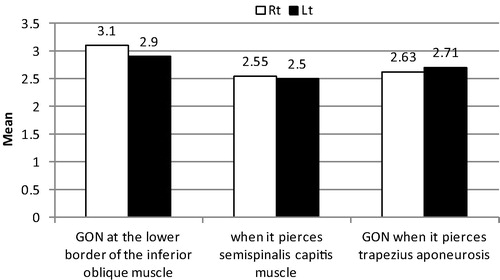
Figure 3 A photograph of right half of head and neck specimen showing the greater occipital nerve (GON) piercing semispinalis capitis (SSC). (TR: trapezius reflected).
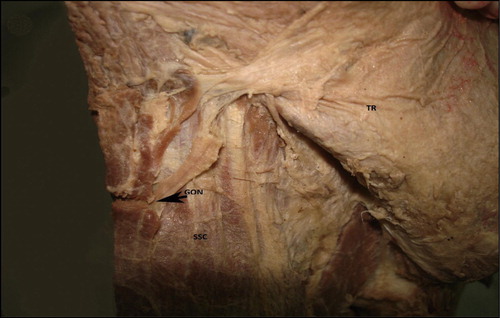
Figure 7 Posterior view of right half of head and neck specimen showing the greater occipital nerve (GON) parallel to the occipital artery (OA). (SSC: semispinalis capitis – TR: trapezius).
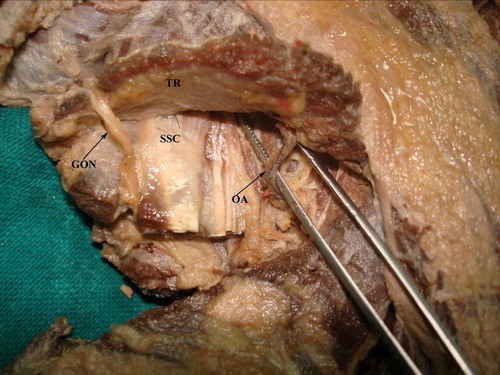
Table 1 showing the anatomical measurements of GON in mm. (RT: right-LT: left-GON: greater occipital nerve).
After traversing the inferior oblique muscle, GON runs between inferior oblique and the deep surface of semispinalis capitis (SSC) (). Then the GON pierces SSC muscle (). The diameter of GON where it pierces SSC was shown in , .
The distance between the point where the GON pierced SSC inferior to the external occipital protuberance (EOP) and lateral to the midline was measured (, ). After the GON pierced SSC, it pierces the trapezius aponeurosis to reach the scalp ( and ). The diameter of GON after its exit from trapezius muscle was shown in , . Then it travels to supply the integument of the scalp through multiple branches ().
Figure 4 Lateral view of right half of head and neck specimen showing the greater occipital nerve (GON) piercing semispinalis capitis (SSC) then piercing trapezius aponeurosis (TR). (IOP: internal occipital protuberance-EOP: external occipital protuberance).
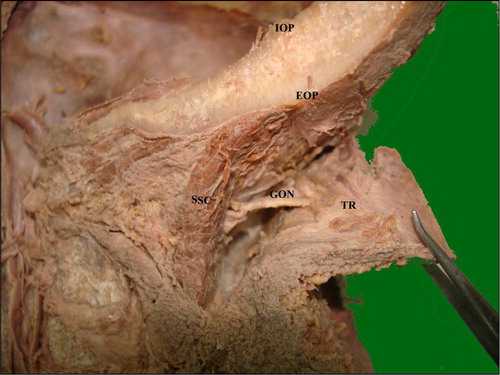
Figure 5 Lateral view of right half of head and neck specimen showing greater occipital nerve (GON) piercing semispinalis capitis (SSC) then trapezius aponeurosis (TR). This view shows the relation of GON to external occipital protuberance (EOP). (IOP: internal occipital protuberance).

Figure 6 Posterior view of right half of head and neck specimen showing the greater occipital nerve (GON) traversing the semispinalis capitis (SSC) and trapezius aponeurosis (TR) then dividing into 3 branches (arrow) to supply the scalp.

Figure 8 representing the mean distance of GON inferior to external occipital protuberance, lateral to the midline and from occipital artery.
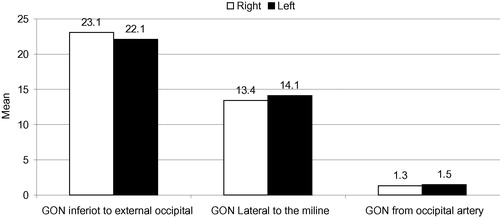
Table 2 showing the distance of GON inferior to external occipital protuberance, lateral to the midline and from occipital artery in mm.
During the course of GON through the SSC to reach the scalp, the GON travels parallel to the occipital artery (). The distance between GON and occipital artery was measured and recorded in , .
3.2 Clinical results
In this prospective study, 20 patients (15 females and 5 males) suffering from migraine diagnosed according to International Headache Society (IHS) criteria (HIS 2004) were treated using GON blockade.
The landmark for GON injection was based on the anatomical study which revealed the followings;
For the right GON: the vertical location inferior to EOP ranged from 19.85 mm to 26.9 mm with a mean of 23.1 mm. The lateral location from EOP ranged from 11.03 mm to 14.65 mm with a mean of 13.4 mm.
For the left GON: the vertical location inferior to EOP ranged from 16.89 mm to 29.5 mm with a mean of 22.1 mm. The lateral location from EOP ranged from 10.89 mm to 15.31 mm with a mean of 14.1 mm.
The blocks were performed with 1.5 ml of 0.5% bupivacaine from 13.4 mm lateral and 23.1 mm inferior to the external occipital protuberance for the right GON and 14.1 mm lateral and 22.1 mm inferior to the external occipital protuberance for the left GON.
Patients were given GON blocks with 0.5% bupivacaine and repeated depending on the clinical response. Patients were evaluated immediately after injection and were followed after 1 month. During the treatment and entire follow-up period, the patients avoided prophylactic therapy.
Treatment was assessed using the visual analogue scale for migraine pain.
Pain was improved in 70% of patients within the first hour after the first injection. After 1 month, 60% of patients still showed improvement.
No undesirable effect related to GON block was observed in the present study.
4 Discussion
Anatomical variants of GON may be the cause of individual treatment failures of blind nerve blocks. The blind nerve blocks are used for the treatment of occipital headaches.
The greater occipital nerve GON appeared at the lower border of inferior oblique muscle. After traversing the inferior oblique muscle, GON run between it and the deep surface of semispinalis capitis SSC. Then the GON pierces SSC muscle. After the GON pierced SSC, it pierces the trapezius aponeurosis to reach the scalp to supply the integument of the scalp through multiple branches.
Anatomy textbooksCitation8,Citation9 describe the course of the greater occipital nerve as curving medially around the semispinalis muscle and only piercing a fascial plane in the region of the superior nuchal line. This does not agree with the findings of the present study.
Ducic et al.Citation10 reported that the GON proceeds between the inferior oblique and the semispinalis capitis muscle and then pierces medially to the semispinalis capitis muscle. It courses obliquely, in a superolateral fashion and is considerably more lateral at the level of the occipital prominence. It then penetrates through the trapezius muscle to join the occipital artery. Mosser et al.Citation11 found the greater occipital nerve piercing the semispinalis capitis on both sides of 20 cadavers. This agrees with the findings in the present study.
In the present work, it was found that the mean diameter of GON at the lower border of inferior oblique muscle was 3.1 ± 0.2 mm on the right side and 2.9 ± 0.4 mm on the left side. The mean diameter of GON when it pierces semispinalis capitis muscle was 2.55 ± 0.214 mm on the right side and 2.50 ± 0.195 mm on the left side. Mosser et al.Citation11 found the average diameter of GON 2.7 mm to 2.4 mm on the right and 3.0 mm to 2.9 mm on the left as the GON passes through the SSC muscle. ShimCitation12 found the average diameter of the GON between EOP and mastoid process measured by ultrasound, was 2.9 ± 0.4 mm on the right and 3.1 ± 0.3 mm on the left.
The mean diameter of GON when it pierces trapezius muscle was 2.63 ± 0.073 mm on the right side and 2.71 ± 0.065 mm on the left side in the present study. Mosser et al.Citation11 found the average diameter of GON distal to the site of emergence from semispinalis muscle was 2.4 mm on the right side and 2.9 mm on the left side.
The mean distance of GON inferior to external occipital protuberance on the right side was 23.1 ± 3.4 mm and 22.1 ± 5.0 mm on the left side in the present study. While the mean distance of GON lateral to midline on the right side was 13.4 ± 1.65 mm and 14.1 ± 2.07 mm on the left side. Greher et al.Citation13 reported that the distance from the EOP to the GON was 17.4 mm (11.1–22.8 mm) in their cadaveric study. ShimCitation12 found the distance to be 23.1 ± 3.4 mm on the right and 20.5 ± 2.8 mm on the left from the EOP to the GON.
In the present work, the GON travels parallel to the occipital artery in all specimens, while Janis et al.Citation14 found the greater occipital nerve and occipital artery crossing each other in 54% of specimens. The relationship between these structures when they crossed varied from a single intersection to a helical intertwining. Becser et al.Citation15 stated that the GON surrounded the occipital artery while Guvencer et al.Citation16 found the GON’s route is nearly parallel to the OA and the GON’s branches surround the OA.
In the present work, it was found that the mean distance between the GON and the occipital artery was 1.3 ± 0.4 mm on the right and 1.5 ± 0.3 mm on the left.
JaeCitation12 found the distance between the GON and the occipital artery was 1.5 ± 0.6 mm on the right and 1.2 ± 0.6 mm on the left, representing no significant difference. These values were similar to the values of the present study.
Greater occipital nerve block has been part of headache medicine for more than half a century, with injection techniques and solutions varying greatly. The rationale of performing a GONB for the treatment of chronic headache states is on the anatomical connections between trigeminal and upper cervical sensory fibres at the level of the trigeminal nucleus caudalis. However, the reason for the improvement after GONB in primary headache is unknown.Citation7
There are considerable differences in the proposed landmarks for the GON blockade in the literature ().Citation7
Table 3 Variation of anatomical sites for greater occipital nerve.Citation17
In the present study, the proposed landmark for GON blockade was 13.4 mm lateral and 23.1 mm inferior to the external occipital protuberance for the right GON and 14.1 mm lateral and 22.1 mm inferior to the external occipital protuberance for the left GON. These measurements were based on an anatomical study in which twenty five specimens of head and neck were dissected to show the location of greater occipital nerve.
Pain was improved in 70% of patients after 5 min of first injection. After 1 month, 60% of patients still had improvement. This was in agreement with Young et al.Citation18 who performed greater occipital nerve blocks on 24 migraineurs and revealed 64%, reduction in pain after 5 min.
Similarly Takmaz et al.Citation19 in their series of 10 patients treated for migraine using GON injection had shown a good response in the majority of the patients.
5 Conclusion
GON block with 0.5% bupivacaine 13.4 mm lateral and 23.1 mm inferior to the EOP for the right GON and 14.1 mm lateral and 22.1 mm inferior to the EOP for the left GON is effective in reducing pain severity in migraine patients and with no adverse effect.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 19 August 2014
References
- A.WilliamsR.L.M.NewellM.S.DaviesThe legS.StandringGray’s anatomy39th ed2005Elsevier Churchill Livingstone515
- Ernest W, April. Clinical anatomy. 3rd ed.; 1997. P. 495.
- Chummy S. Sinnatamby Last’s anatomy Regional and Applied. 10th ed.;1999:424.
- Mehmet.BaykalGreater occipital nerve block in migraine headacheAGRI212200983
- C.A.WarfieldZ.H.BajwaPrinciples and practice of pain medicine2nd ed.2004McGraw HillNew York 268–9
- J.M.S.PearceHeadaches in the whiplash syndromeSpinal Cord392001228233
- M.G.SaraccoW.ValfrèM.CavalliniM.AguggiaGreater occipital nerve block in chronic migraineNeurol Sci31Suppl 12010 JunS179S18010.1007/s10072-010-0320-7
- F.H.NetterAtlas of human anatomy1989Ciba-Geigy CorporationSummit, N.J
- K.L.MooreClinically Oriented Anatomy3rd ed.1992Williams & WilkinsBaltimore
- I.DucicM.MoriartyA.Al-AttarAnatomical variations of the occipital nerves: implications for the treatment of chronic headachesPlast Reconstr Surg1232009859863
- S.W.MosserB.GuyuronJ.E.JanisR.J.RohrichThe anatomy of the greater occipital nerve: implications for the etiology of migraine headachesPlast Reconstr Surg11322004 Feb693697
- Jae HangShimSo YoungKoMi RangBangWoo JaeJeonSang YunChoJong HoonYeomUltrasound-guided greater occipital nerve block for patients with occipital headache and short term follow upKorean J Anesthesiol61120115054 July
- M.GreherB.MorigglM.CuratoloL.KirchmairU.EichenbergerSonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissectionBr J Anaesth1042010637642
- J.E.JanisD.A.HatefE.M.ReeceP.D.McCluskeyT.A.SchaubB.GuyuronNeurovascular compression of the greater occipital nerve: implications for migraine headachesPlast Reconstr Surg1266201019962001
- N.BecserG.BovimO.SjaastadExtracranial nerves in the posterior part of the head: anatomic variations and their possible clinical significanceSpine2313199814351441
- M.GuvenceraP.AkyeraS.SayhanS.TetikaThe importance of the greater occipital nerve in the occipital and the suboccipital region for nerve blockade and surgical approaches – An anatomic study on cadaversClin Neurol Neurosurg1132011289294
- ACNR • volume 8 number 3 • July/August; 2008.
- Young W, Cook B, Malik S, Shaw J, Oshinsky M. Headache 2008;48(7):1126–8, 2008 [Jun 28]. 10.1111/j.1526-4610.2008.01146.x. Epub.
- S.A.TakmazN.InanS.UçlerM.A.YazarL.InanH.BaşarGreater occipital nerve block in migraine headache: preliminary results of 10 patientsAgriculture20120084750
