Abstract
Background: Anemia in pregnancy is common and linked to postpartum hemorrhage in terms of uterine atony. The more severe the anemia, the more likely the greater blood loss and adverse outcome. The aim of this study was to examine the association between anemic women at labor and postpartum hemorrhage (PPH) during emergency cesarean delivery and to assess the hemoglobin (Hb) values at which the emergency hysterectomy is needed. Methods and patients: A cross-sectional study was carried out between (Aug. 1st 2012 and Jul. 30th 2013) at Al Thawra General hospital. Fifty-three cases were included in the study. Results: Postpartum hemorrhage was developed in 53 women (29.1%). Out of 53 women, 21 cases (39.6%) had severe uterine atony and required emergency hysterectomy and the remaining 32 cases (60.37%) responded to the conservative measures (p 0.03). Most of the hysterectomized women 80.75% (17/21) had Hb levels ⩽ 7 versus 12.5% of the nonhysterectomized patients [OR 29.75; 95% CI 6.564–134.53; p < 0.01]. There was a strong correlation between low Hb levels and blood loss [r = −.619; p < 0.00]. Conclusion: Our study supports the association between anemia (Hb < 10) and the risk of PPH. We also provide evidence of the association between severe anemia and emergency hysterectomy.
1 Introduction
Anemia in pregnancy is defined as hemoglobin level below 11 g/dl (WHO).Citation1 It is one of the public health problems mostly in developing countries.Citation2 World Health Organization (WHO) reported that the prevalence of anemia during pregnancy in developing countries exceeds 50%.Citation1 In pregnancy, anemia is mainly nutritional due to dietary deficiency of iron and folatesCitation3 but impaired absorption, chronic blood loss, increased requirement, concurrent medical disorders and malaria are other contributing factors for anemia.Citation4 It has long been considered that anemia increases the risk of postpartum hemorrhage (PPH)Citation5 and the two conditions together contribute to 40–43% of maternal deaths in Africa and Asia.Citation6
Few studies exist that have linked the risk of PPH by level of anemia and indicate a weak association.Citation7 Recently small studies demonstrated causal – relationship between severe anemia and uterine atony which is the main cause of PPH accounting for about 90% in most studies.Citation8
Similar to other less developing countries, anemia is prevalent in our area particularly in remote setting where the accessibility to antenatal care services is difficult. It is not uncommon to see women at time of labor with uncorrected moderate to severe anemia. They are often unbooked and seeking hospital only when severe obstetric complications have already developed. The aim of this study was to find out the rate of PPH among women with low hemoglobin concentration (Hb < 10) during emergency cesarean delivery and to assess the Hb level at which cesarean hysterectomy is needed.
2 Patients and methods
This study was a cross-sectional observational trial conducted over a year (from August 1st 2012 to July 30th 2013) in Al Thawra General Hospital. The study included all singleton pregnant women, 38 weeks gestational age or more (based on early first trimester ultrasonography and/or LMP), who delivered by cesarean section and having moderate to severe anemia (Hb < 10 g/dl) at admission. Anemia is defined according to WHO criteria: mild (Hb 10–10.9 g/dl), moderate (Hb 7–9.9) and severe (Hb < 7).
We excluded from the study any women with risk factors for uterine atony [i.e. over distended uterus, parity ⩾ 5, history of previous PPH, bleeding tendency, etc.]. Fifty-three women met our criteria were included in this study. An informed consent was taken from each participant and the ethical approval was obtained from the hospital ethics committee. The study was conducted in accordance with the Helsinki declaration. Maternal characteristics such as age, parity, gestational age, booking status, previous scar and pregnancy complications were noted. Clinical evaluation and routine investigation including initial hemoglobin levels, urine analysis and other tests were performed as indicated.
The hospital protocol for prevention of PPH was followed which relies on the administration of 600 μg misoprostol (3 tablets) rectally at the time of scrubbing, in addition to oxytocin infusion (20 units in 500 ml normal saline solution infused over 30 min). Circumstances in which additional uterotonic agents are required, injection of methyl ergometrine (if no contraindication), increasing the oxytocin infusion doses, local injection of either or both drugs are used as appropriate. Cesarean section was performed as standard by the senior-in charge and one resident doctor, under spinal anesthesia with Pfannenstiel skin and lower uterine segment transverse incisions. The intraoperative blood loss was estimated by using the calibrated Steri-Drape TM Loban TM 2 (3M Health Care, St. Paul, Minnesota, USA) for all cases. Collected blood within the drape was added to the content of suction bottle and counted. The surgical swabs were weighed and the differences in weight between soaked and dry [1 g = 1 m] were added. All patients received prophylactic antibiotics and blood transfusion. Hysterectomy was performed by senior in charge and on-call consultant after discussion when conservative measures failed to restore uterine tonus namely bimanual uterine massage, use of additional uterotonic agents, compression sutures and uterine artery ligation.
The outcome measures were the rate of PPH in these anemic patients, the level of Hb among those women who needed hysterectomy, estimation of blood loss, amount of blood transfused the interval from delivery till completing the hysterectomy and the type of hysterectomy.
2.1 Statistical analysis
Analysis of the data was carried out using SPSS version 21. Values given are mean ± SD or percentages as appropriate. Independent sample t-test was used to evaluate the association between continuous variables and Chi-square test for categorical variables.
Odds ratio and 95% confidence interval (CI) were calculated. A p value of ⩽0.05 was considered statistically significant.
3 Results
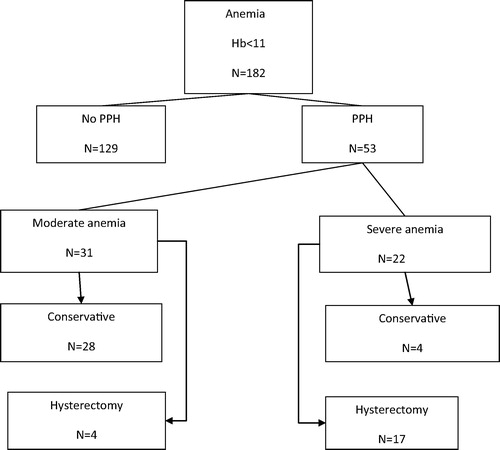
A total of 11,680 deliveries were recorded. One hundred eighty-two women had Hb ⩽ 11 g/dl at the time of admission. Of these, 53 women (29.1%) were developed PPH due to uterine atony during cesarean section (). Maternal obstetrics and demographic data are shown in . Of the 53 women who developed uterine atony, 32 cases (60.37) were successfully managed by conservative measures: additional uterotonic drugs 49% (26/53), 4 cases (7.5%) by B-Lynch compressive sutures with success rate of 50%, 4 cases (7.5%) by uterine artery ligation with success rate of 75%, and internal iliac artery ligation in only one case (1.8%). Severe bleeding that required emergency hysterectomy was developed in 39.6% (21/53) of cases. The difference was statistically significant (p < 0.03) (). We further analyzed hysterectomized and nonhysterectomized patients as regards Hb, blood loss, and parity. We found that the majority of hysterectomized women 80.95% (17/21) had Hb ⩽ 7 and 87.5% (28/32) of nonhysterectomized patients had Hb > 7. The difference was significant {OR 29.75; 95% CI 6.564–134.53; p .00}.
Table 1 Maternal characteristics.
Table 2 Outcome results of the two groups.
The mean blood loss among hysterectomized patients was 1688 ± 238.7 ml versus 1517.18 ± 353.23 ml in the nonhysterectomized patients. The difference was significant (P = 0.05). The amount of bleeding (>1500 ml) was significantly higher in the hysterectomized than that in the nonhysterectomized women [OR 6.5; 95% CI 1.28–32.8; P = 0.01] ().
Table 3 Comparison between hysterectomized and nonhysterectomized patients.
Nineteen women (91.47%) had cesarean hysterectomy while the remaining 2 cases (9.5%), the hysterectomy was performed after abdominal closure due to persistent vaginal bleeding.
Subtotal hysterectomy was the commonest type of operation performed (80.95%). Disseminated intravascular coagulopathy (DIC) was developed in 7 cases (33.3%) of hysterectomized group versus one case (3.1%) of conservative group. Eight cases of the two groups were admitted to intensive care unit (ICU). There was no maternal mortality recorded in our study.
4 Discussion
The present study shows that 29.1% of anemic women were developed PPH during cesarean delivery due to uterine atony. Prior studies have demonstrated that severe anemia may impair myometrial contractility resulting from impaired transport of hemoglobin and oxygen to uterus causing tissue enzymes and cellular dysfunction.Citation9,Citation10 In this study severe uterine atony required emergency hysterectomy was occurred in 39.6% (32/53) of women who had severe anemia (Hb ⩽ 7 g/dl).
This finding indicates that for the patients with Hb of 7 or less the odds (or likelihood) of having PPH due to uterine atony increases greatly compared to patients with Hb 7.1–10 (p = .00). Although nulliparous women were associated with 11.6% increased risk for developing PPH in our patients, this tendency was not significantly different from women with parity > 1 (p = 0.86). This result is consistent with other study.Citation11
The results of the present study showed lower mean blood loss 1584.9 ± 321.8) than 4700 ± 1949 that reported by Zamzami Yamani who analyzed 17 cases of peripartum hysterectomy at king Abdulaziz University Hospital. Only 9 cases had uterine atony while the remaining 8 cases were presented with placenta previa and morbid adherent placenta with previa.Citation12 The differences in the population contributing factors could partly explain such expected variation. Additionally all women in our study received rectal misoprostol and oxytocin intraoperatively. The combination of these agents may be responsible for reduction of hemorrhage and thus better outcome. This suggests the importance of the active management of the third stage of labor in reducing blood loss. Elbourrne et al.Citation13 reported significant reduction of the amount of blood loss when prophylactic administration of uterotonic agents during the third stage of labor. Similarly Badejoko et al.Citation14 reported dramatic effect of rectal misoprostol (600 μg) in prevention of PPH comparable with oxytocin infusion.
The correlation between Hb values and blood loss was inversely significant (Pearson R = −.619 at P < 0.00) indicating the more severe the anemia, the more likely of greater blood loss.
This result highlights the need to increase the population awareness to utilize the available maternity care services along with the promotion of iron and folates supplementation for all pregnant women. The screening and therefore treatment of anemia must be essential part of antenatal care components particularly in setting where malaria and other infectious diseases are prevalent. Of note, the specific cause of anemia was not considered in this study.
We found that cesarean – hysterectomy was done in (39.6%) of cases with uterine atony, similar to other studies.Citation15,Citation16 Recently, the reported success rate for uterine compression sutures is 92% and for uterine artery ligation up to 85%.Citation17 It is noticed in this study that additional measures such as balloon tamponade and systemic pelvic devascularization were underutilized in our hospital. This could possibly be related to the probability that in these anemic women in particular other surgical conservative techniques may further increase blood loss with possible risk of failure or might be due to lack of experience. The mean time from delivery to completing hysterectomy in this study was (155.71 ± 52.4 min). This finding is in contrast to the Forna et al.Citation18 who analyzed 38 cases of cesarean-hysterectomy from 1990 to 2002 and found the mean time as (303.1 ± 219.9) min.
The variation may likely be explained by the type of hysterectomy. In the current study total abdominal hysterectomy was performed in only 4 cases (7.5%) compared to (50.9%) in their study. Although there is no consensus as the appropriate timing for resorting to hysterectomy in atonic uterus,Citation17 the patient’s general condition, the severity of blood loss, and the effectiveness of the conservative measures should direct the decision-making process. However, because anemic women have poor tolerance to even mild bleeding,Citation19 rapid deterioration in the hemodynamic stability should be considered.
According to our results, we proposed that severe anemia (Hb ⩽ 7 g/dl) combined with ongoing bleeding despite other conservative measures is predictors of persistent myometrial contractility failure, and warrant early hysterectomy.
Few studies have addressed the causal-relationship between severe anemia and PPH, but there is no data as what is the exact value of Hb at which the potential uterine atony could be imminent. Such investigation will provide the obstetricians a new sophisticated tool to recognize pregnant women at risk and therefore providing them with the standards of care. Our work can be of particular relevance that may enhance researchers to address the issue.
The present study has certain limitations. We used the available sample size that could be small and may not be representative for whole population. Also the study considered only women who underwent cesarean section while vaginal delivery was not included because this subgroup of anemic women are poor, mostly from remote settings, unbooked, often deliver at home and seeking hospital only when severe complications have already developed. We also did not consider the prevalence of anemia because this study was designed to assess women with Hb < 10 g/dl. Mild anemia is common and tends to have less significant impact on labor and delivery complications.
5 Conclusion
The finding of this study support the link between low hemoglobin levels at delivery and the potential risk of PPH which remains currently debated. Also we provide evidence of the association between severe anemia and severe uterine atony requiring emergency hysterectomy.
Further studies with larger sample size to confirm these findings are required. In this subgroup of anemic women who develop severe PPH due to uterine atony, early decision of hysterectomy to save their lives is potential and should be considered when other measures are ineffective.
6 Disclosure
The author declared that there is no conflict of interest.
Acknowledgments
We thank Dr. BoranAltincicek in Bonn University, Germany for his assistant in statistical analysis and for all colleagues for their kindly helping in the data collection and support.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 6 January 2015
References
- Candio F, Hofmeyr GJ. Treatments for iron-deficiency anaemia in pregnancy: RHL commentary. The WHO Reproductive Health Library; Geneva: World Health Organization [last revised: 23.11.07].
- WHO. Micronutrient deficiency: battling iron deficiency anaemia: the challenge; 2004. http://www.who.int%20nut/ida.htm [accessed 13.06.13].
- T.G.SanghviP.W.HarveyE.WainwrightMaternal iron-folic acid supplementation programs: evidence of impact and implementationFood Nut Bull312010100107
- K.KalaivaniPrevalence and consequences of anemia in pregnancyInd J Med Res1302009627633
- G.RamanathanS.ArulkumaranPostpartum hemorrhageJ Obstet Gynecol Can28112006967973
- Christian P. Nutrition and maternal survival in developing countries. In: Lammi-keefe CJ, Couch SC, Philipson EH. Handbook of nutrition and pregnancy (USA), 1st ed.; 2008. p. 319–36 [chapter 21].
- N.L.SloanE.JordanB.WinikoffEffects of iron supplementation on maternal hematologic status in pregnancyAm J Public Health922002288293
- G.CaroliC.CuestaE.AbalosAM.GulmezogluEpidemiology of postpartum hemorrhage: a systematic reviewBest Pract Res Clin Obstet Gynecol22620089991012
- J.A.KavleR.J.StoltzfusF.WitterJ.M.TielschS.S.KhalfanAssociation between anemia during pregnancy and blood loss at and after delivery among women with vaginal births in Pemba lsland, Zanzibar, TanzaniaHealth Popul Nutr2522008232240
- R.JaleelA.KhanSevere anemia and adverse pregnancy out comeJ Surg Pak1342008147150
- H.M.Al-KadriS.TariqH.M.TamimRisk factors for postpartum hemorrhage among Saudi womenSaud Med J3010200913051310
- T.Y.Yamani ZamzamiIndication of emergency peripartum hysterectomy: review of 17 casesArch Gynecol Obstet2682003131135
- Elboune DR, Prendiville WJ, Carroli G, Wood J, McDonald S. Prophylactic use of oxytocin in the third stage of labor. Cochrane database of systematic reviews, 2001;4:CD001808.
- O.O.BadejokoA.O.ljarotimiI.O.AwowoleO.M.LotoB.O.BadejokoD.S.OlaiyaAdjunctive rectal misoprostol versus oxytocin infusion for prevention of postpartum hemorrhage in women at risk: a randomized control trialJ Obstet Gynecol Res3811201212941301
- P.ChristopoulosD.HassiakosA.TsitouraK.PanoulisK.PapadiasN.VitoratosObstetric hysterectomy. A review of cases over 16 yearsJ Obstet Gynecol3122011139141
- M.F.El JalladF.ZayedH.S.Al-RimawiEmergency peripartum hysterectomy in Northern Jordon: indications and obstetric outcome (an 8 year review)Arch Gynecol Obstet27042004271273
- J.AhonenV.StefanovicR.LasslaManagement of postpartum hemorrhageActa Anaesthesiol Scand54201011641178
- F.FornaA.M.MilesD.J.JamiesonEmergency peripartum hysterectomy: a comparison of cesarean and postpartum hysterectomyAm J Obstet Gynecol190200414401444
- K.KalaivaniPrevalence and consequences of anemia in pregnancyInd J Med Res1302009627633