Abstract
Elderly people constitute an increasing proportion of those presenting with acute upper gastrointestinal bleeding. Not only in upper gastrointestinal bleeding is advanced age a risk of death, but also exceeding 60 years of age results in an increased risk of cerebrovascular and cardiovascular events. Factors likely to influence the morbidity and mortality associated with endoscopy in an elderly cohort with acute gastrointestinal bleeding include the acuity and severity of bleeding and the presence of comorbid conditions. Audits have shown a surprisingly high incidence of both morbidity and mortality following upper gastrointestinal endoscopy. The following incident is a case report of a cerebrovascular accident following diagnostic upper gastrointestinal endoscopy for an elderly patient with acute upper gastrointestinal bleeding.
1 Case report
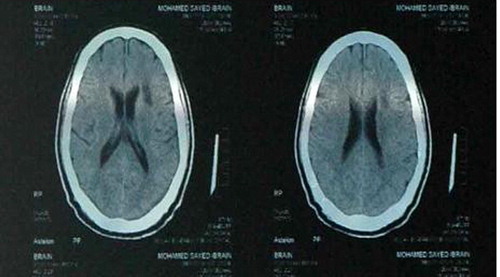
A 67-year-old man presented to the hospital on July 2009 complaining of hematemesis of large amount of coffee ground blood. His medical history consisted of hypertension and diabetes mellitus. He was a smoker and using baby aspirin. His pulse rate was 114 beats per minute and blood pressure 140/90 mmHg. The physical examination was unremarkable. Relevant laboratory values included hemoglobin of 9 g/dl. Liver and kidney function tests were normal. ECG was normal. Four hours later he developed a second attack of hematemesis. His blood pressure was 130/90 mmHg and pulse rate 130 beats per minute. He received normal saline and one unit blood. Early upper endoscopy was performed five hours after admission. The patient was American Society of Anesthesiologists (ASA) score 2 and initial Rockall score 2. Endoscopy was performed by a staff with attendance of a senior staff. A first degree relative signed the consent. Pre-procedure basic vital signs monitoring using pulse oximetry revealed pulse rate 98 beats per minute and blood pressure 93/47 mmHg. The patient had been sedated with IV midazolam (1 mg) but he was agitated during the procedure which necessitated adding 1 mg midazolam. Supplemental oxygen was administered during endoscopy. The patient was awake during and after the procedure. Pulse oximetry showed persistent oxygen saturation >90% and transient drop of pulse rate to 54 beats per minute during the procedure. Endoscopy revealed normal esophagus and duodenum but the stomach was full of blood and could not be examined. The source of bleeding was not identified so the endoscopist decided to repeat the endoscopy after 24–48 h. Postprocedure vital signs monitoring revealed pulse rate 110 beats per minute and oxygen saturation 100%. During follow up, blood pressure was 130/90 mmHg and pulse rate 120 beats per minute. Twenty-four hours after endoscopy, the patient suffered an ischemic-cerebrovascular stroke leaving him with right sided hemiplegia, aphasia and bedridden. Urgent CT scan of the brain without contract revealed left fronto-parietal infarction (). ECG was normal. CPK-MB and troponin levels were normal. Hemoglobin level was 5 g/dl. The patient received five units of blood and his pulse rate dropped to 95 beats per minute and hemoglobin recovered to 10 g/dl. For this reason, it was decided to refrain from second endoscopy. The patient received pantoprazole 40 mg per day for the possibility of ulcer, was advised to stop smoking and started physiotherapy. Few days later he received baby aspirin 75 mg per day. The patient was retained in the hospital for two weeks and discharged without diagnosing the cause of bleeding. He was followed up in the outpatient clinic.
A staff meeting was called to analyze why and how this complication had occurred and to consider strategies to minimize the risk of further complications. An elderly hypertensive diabetic patient presented with hematemesis underwent emergency diagnostic endoscopy five hours after admission and developed a cerebrovascular stroke 24 h after endoscopy. The possible cause for the cerebrovascular accident was severe prolonged postbleeding hypovolemia in an elderly patient. The patient had persistent tachycardia (>100 beats per minute) from admission till the occurrence of the stroke. Hemoglobin level was checked only twice on admission and after the stroke (9 g/dl and 5 g/dl, respectively). Hemoglobin level was not checked before the procedure. Hypotension (93/47 mmHg), documented immediately before the procedure, was ignored. Transient bradycardia (54 beats per minute) occurred during the procedure which may be accompanied with hypotension. Blood pressure was not assessed during the procedure. In spite of evidence of active bleeding (blood in stomach and tachycardia), close observation (pulse rate, blood pressure and hemoglobin level) was not performed for 24 h until the patient had the stroke. After the stroke, assessment of hemoglobin level revealed a low hemoglobin level (5 g/dl). Consequently the patient received massive blood transfusion (five units) which corrected the hemodynamic instability and anemia. Corrective actions were undertaken. In elderly or at risk patients with acute upper gastrointestinal bleeding, intense monitoring and early rapid resuscitation should be performed. Hemoglobin level should be checked every four to six hours. Blood pressure and pulse rate should be monitored before, during and after any endoscopic procedure. An endoscopic procedure may need to be deferred if the patient’s blood pressure is too low. The hypotensive patient may require resuscitation with blood and/or IV fluids before it is safe to proceed. Good communication is necessary to improve staff performance.
Four years later the patient presented with an attack of hematemesis and melena. His pulse rate was 130 beats per minute, blood pressure 80/50 mmHg and hemoglobin 7 g/dl. He received four units of blood transfusion. Bleeding stopped spontaneously. Endoscopy was postponed until stabilization of hemodynamic state and hemoglobin level recovered to 11 g/dl. Endoscopy was performed 48 h after admission. The patient had been sedated with IV midazolam (2.5 mg). Supplemental oxygen was administered during endoscopy. Blood pressure, pulse rate and oxygen saturation were monitored before, during and after the procedure without any significant change. The patient was ASA score 3, initial Rockall score 4 and final Rockall score 5. Endoscopy revealed a pre-pyloric gastric ulcer with flat pigmented spot. Biopsy for Helicobacter pylori was positive. The patient received a course of 500 mg Clarithromycin, 20 mg Omeprazole and 500 mg Tinidazole; all given twice daily for two weeks. He was discharged few days later without complications. Follow up endoscopy performed after two months revealed normal endoscopic findings and biopsy for Helicobacter pylori was negative. The patient was followed in the outpatient clinic until the time of writing this report.
2 Discussion
Elderly people (aged over 60 years) constitute an increasing proportion of those presenting with acute upper gastrointestinal bleeding.Citation1 Advanced age has been consistently identified as a risk factor for mortality among patients presenting with upper gastrointestinal bleeding.Citation2,Citation3 Not only in upper gastrointestinal bleeding is advanced age a risk of death, but also exceeding 60 years of age results in an increased risk of cerebrovascular and cardiovascular events.Citation4 Thus, these patients need particular attention. Factors likely to influence the morbidity and mortality associated with endoscopy in an elderly cohort with acute gastrointestinal bleeding include the acuity and severity of bleeding and the presence of comorbid conditions. Hypotension at presentation is associated with high mortality among elderly people who present with acute upper gastrointestinal bleeding and early aggressive volume resuscitation decreases mortality.Citation5 Urgent endoscopic evaluation can be undertaken, provided a risk–benefit assessment has been performed and informed consent has been obtained.Citation6 Tolerance of sedation is an important consideration in elderly patients, who require lower doses of benzodiazepines than non-elderly patients.Citation6 Elderly patients prescribed benzodiazepines for sedation can be prone to oxygen desaturation during endoscopy.Citation6
Audits of endoscopic practice have shown a surprisingly high incidence of both morbidity and mortality following gastrointestinal endoscopy.Citation7,Citation8 Complications of gastrointestinal endoscopy include sedation-related complications (cardio-pulmonary and cerebrovascular) and complications specific to diagnostic and therapeutic gastrointestinal endoscopy.Citation9 It was reported that both transient ischemic attacks and fully completed strokes can and do occur both during and following endoscopic procedures.Citation7,Citation8,Citation10,Citation11 Possible mechanisms include periods of hypo or hypertension, cardiac arrhythmias or as a consequence of a myocardial infarction. Hypotension can occur due to sedation.Citation9 Benzodiazepines (midazolam, diazepam) have a mild vasodilatory effect and usually produce only a slight fall in blood pressure in normal sedative doses. Sedation may cause more profound falls in blood pressure in a hypovolemic patient e.g. due to blood loss or dehydration. Hypotension can also occur due to bradycardia – of any cause.Citation9 A fall in heart rate (e.g. as a result of vagal stimulation) and/or cardiac stroke volume will also lower blood pressure.
We report a cerebrovascular stroke that occurred in an elderly male patient following diagnostic endoscopy. The patient is smoker and has been suffering from hypertension. He presented to internal medicine department suffering from acute upper gastrointestinal bleeding. Exposure of a high risk patient to acute severe hypovolemia, anemia, sedation and minor invasive procedure was responsible for the occurrence of this complication. Suboptimal performance included inadequate monitoring, negligence of pre-procedure assessment data, poor communication and delay in resuscitation. Measures were instituted to improve patient care and ensure safety of endoscopy in elderly patients with acute upper gastrointestinal bleeding. This case report illustrates the need for close observation, aggressive fluid resuscitation, risk stratification in assessment of comorbidities before, continuous hemodynamic monitoring, proper evaluation before any interference regardless of age, a culture of team working and safety first throughout the unit in the management of elderly patients with acute upper gastrointestinal bleeds.Citation9
Complications will always still occur despite the highest standards of practice. Risk is inherent in the procedures that we undertake.Citation9 Our professional responsibility is therefore to completely prevent avoidable risks and to reduce unavoidable risks to an absolute minimum.Citation9 Audit of complications with regular review meetings involving all physicians to give feedback on errors and, ideally, near misses should be performed.Citation9 When a complication or error occurs, a careful investigation of clinical practice should be undertaken and continuous quality improvement should be implemented. Performance assessment, monitoring and continuous quality improvement have been recommended by professional societies as a part of clinical practice.
Conflict of Interest
None declared.
Case report
All authors approved manuscript submission.
Funding
None.
Ethical approval
Not needed.
The manuscript is not being submitted concurrently elsewhere and was not presented at any place.
Consent
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 2 February 2015
References
- K.C.ThomopoulosK.A.VagenasC.E.VagianosChanges in aetiology and clinical outcome of acute upper gastrointestinal bleeding during the last 15 yearsEur J Gastroenterol Hepatol162004177182
- T.A.RockallR.F.LoganH.B.DevlinT.C.NorthfieldIncidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal HemorrhageBMJ3111995222226
- B.KatschinskiR.LoganJ.DaviesG.FaulknerJ.PearsonM.LangmanPrognostic factors in upper gastrointestinal bleedingDig Dis Sci391994706712
- P.WierzchowskiS.DąbrowieckiW.SzczęsnyUrgent endoscopy in elderly patients with non-variceal upper gastrointestinal bleedingVideosurgery Miniinv72012246250
- R.BaradarianS.RamdhaneyR.ChapalamaduguL.SkoczylasK.WangS.RivilisEarly intensive resuscitation of patients with upper gastrointestinal bleeding decreases mortalityAm J Gastroenterol992004619622
- P.YachimskiL.FriedmanGastrointestinal bleeding in the elderlyNat Clin Practice520088093
- M.A.QuineG.D.BellR.F.McCloyJ.E.CharltonH.B.DevlinA.HopkinsProspective audit of upper gastrointestinal endoscopy in two regions of England: safety, staffing and sedation, methodsGut361995462467
- C.J.A.BowlesR.LeicesterC.RomayaE.SwarbrickC.B.WilliamsO.EpsteinA prospective study of colonoscopy practice in the United Kingdom today – are we adequately prepared for national colorectal cancer screening tomorrow?Gut532004277283
- Green J. Complications of gastrointestinal endoscopy. BSG Guidelines in gastroenterology. <http://www.bsg.org.uk/pdf_word_docs/complications.pdf>; 2006.
- T.K.DaneshmendG.D.BellR.F.A.LoganSedation for upper gastrointestinal endoscopy: results of a nationwide surveyGut3219911215
- G.D.BellReview – premedication, preparation, and surveillance in “state of the art in gastroenterologic endoscopy – a review of last year’s most significant publications“Endoscopy3620042331