Abstract
Rhabdomyosarcoma is the commonest soft tissue sarcoma in both children and adolescents representing 40% of such tumours in North America and more than 50% in Africa. The involvement of the paratesticular tissue, testis and the kidney are generally rare and more so when it is occurring synchronously. We present a case of 22 year old male with inguinoscrotal swelling, fever and abdominal distention who was diagnosed as having obstructed left inguinoscrotal hernia and a right renal mass. The patient had surgery, and a diagnosis of synchronous rhabdomyosarcoma of the left testis, paratesticular tissue and right kidney was made by histology and immunohistochemistry.
1 Introduction
Rhabdomyosarcoma (RMS) is the commonest soft tissue sarcoma in both children and adolescents representing 40% of such tumours in North America and more than 50% in Africa.Citation1–Citation5 Most reviews document a male preponderance and a bimodal peak age pattern in the first and 5th decades of lifeCitation3,Citation4,Citation7,Citation8,Citation6.
RMS could affect almost all the organs of the body because of its embryological origin. The following main histological types have been recognised; embryonal, alveolar and pleomorphic. The involvement of the paratesticular connective tissue has been reported but kidney involvement is very rare.
Diagnosis is made by histology and some cases supported by immunohistochemistry and electron microscopy.
We present this rare case of a young adult male with synchronous rhabdomyosarcoma of the left testis and right kidney which was thought to be an obstructed inguinoscrotal hernia.
2 Case report
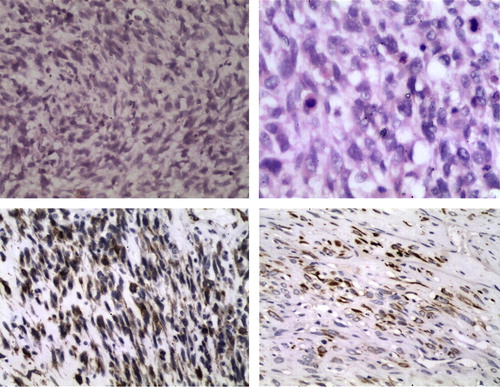
This is a case of a 22 year old male who presented with 3 week history of left inguinoscrotal swelling which suddenly became painful 2 days before presentation, fever, vomiting and abdominal distension with associated urinary symptoms. Examination revealed an acutely ill-looking young male, febrile (temperature 37.8 °C), moderately pale, anicteric and no significant peripheral lymphadenopathy. The abdomen was uniformly distended, tender and dull to percussion with hypoactive bowel sounds. The inguinoscrotal swelling was irreducible and a left testicular mass was palpated. Urgent abdominopelvic ultrasound showed massive ascites and a mass at the right lumbar area. An impression of obstructed inguinoscrotal hernia with peritonitis and associated renal mass was made. Patient was prepared for emergency laparotomy and herniorrhaphy. He subsequently had right nephrectomy and left orchidectomy as both the right kidney and the left testis were found to be tumorous. Grossly, we received a renal mass measuring 16 cm × 10 cm × 4 cm and weighing 230 g; testicular mass measuring 10 cm × 6 cm × 4 cm and weighing 55 g. Cut sections of both showed grey-white fleshy appearance with focal areas of haemorrhage and necrosis. Microscopically, the testis and kidney tissues had features suggestive of rhabdomyosarcoma with a differential of sarcomatous renal cell carcinoma. The slides were reviewed by 5 pathologists and rhabdomyosarcoma was favoured. The tissues were subjected to the following immunohistochemical stains: actin, desmin, S100, pancytokeratin, OCT3/4 and AFP. Actin and desmin were strongly positive while the others were negative. The actin and desmin positivity confirms the diagnosis of RMS ( and ). During the post operative period, there was wound infection which was adequately treated with antibiotics and daily dressing. He was discharged 14th day after surgery and counselled on further treatment. Patient did not come back for follow up and attempt at reaching him was unsuccessful.
Figure 1 Sections of the testis showing malignant neoplasm composed of spindle cells with hyperchromatic and pleomorphic nuclei and abundant eosinophilic cytoplasm. Some of the cells have cytoplasmic extension (tadpole cells) while some are small and round with scanty cytoplasm. There are abnormal mitoses. ((A) H&E ×200; (B) H&E ×200; (C) IHC × 200 desmin positive; (D) IHC × 200 actin positive).
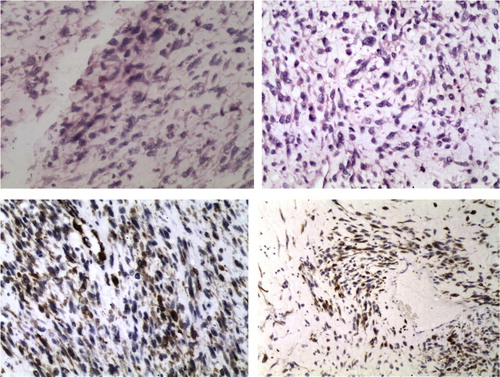
Figure 2 (A) Section of the kidney showing malignant neoplasm composed of spindle cells with hyperchromatic and pleomorphic nuclei and abundant and eosinophilic cytoplasm. Some of the cells have elongated cytoplasmic extension (tadpole cells). There are numerous abnormal mitoses (H&E ×200); (B) Section shows tumour with abnormal mitosis (H&E ×400); (C) IHC × 200 section with strong actin positivity; (D) IHC × 200 section with strong desmin positivity.
3 Discussion
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma in both children and adolescents representing 40% of such tumours in North America and more than 50% in Africa.Citation1,Citation2,Citation4,Citation5 Most reviews document a male preponderance and a bimodal peak age pattern.Citation3,Citation4,Citation6–Citation8 Although more than half of the cases occur within the first decade of life, the second smaller frequency peak is seen mainly in males.Citation1–Citation3,Citation6
RMS can occur in any part of the body due to its embryonal mesenchymal origin and mimics the characteristics of striated muscles.Citation1,Citation9 Histologically, the embryonal and alveolar subtypes are the commonest.Citation1,Citation3,Citation6 Head and neck and genitourinary regions were most frequently affected in most series.Citation3,Citation4,Citation10 Involvement of the extremities is however a phenomenon associated with alveolar RMS.Citation1,Citation10 About 6–7% of RMS arise in the paratesticular region arising from the mesenchymal tissues of the envelope of the testis, epididymis and spermatic cord.Citation2,Citation7,Citation11 It usually presents as a hard painless scrotal, inguinal or inguinoscrotal mass.Citation7 Metastasis to the retroperitoneal lymph nodes is more likely in those older than 10 years, occurring in as much as 26–40% of patients.Citation2
Primary renal RMS is a very rarely reported condition in adults and true renal sarcomas are uncommon in any age group.Citation13,Citation14 Patients within the first two decades of life with renal RMS enrolled in the Intergroup Rhabdomyosarcoma Study Group accounted for less than 0.2% out of a total of 5746 patients.Citation12 All these patients reported with renal masses. One must however ensure, from gross examination of the surgical specimen, that there was no spread from the adjacent retroperitoneal structures.Citation12
Radiological evaluation of choice is computerised tomography.Citation2 Ultrasonography is sufficient for purely scrotal lesions.Citation7 Magnetic Resonance Imaging is also an excellent option for soft tissue evaluation.Citation7 Our patient was evaluated with ultrasonography as he could not afford CT or MRI for financial and logistic considerations.
Treatment of RMS consists of complete surgical excision and adjuvant chemotherapy with or without radiotherapy and is dependent on the stage and group of the tumour.Citation2,Citation7,Citation13 Excision was incomplete as the margins were positive for tumour. Surprisingly no lymph node was submitted for pathology analysis and none was found clinically.
Staging of RMS is not very straight forward as it involves assigning the patient to a stage, a local tumour group and a risk group. Stage assignment is dependent on tumour site, tumour size, state of regional lymph nodes and distant metastases. Tumour group assignment warrants evaluation of the post surgical resection status with pathological determination of margins and lymph node status. Assigning a risk group takes into consideration the stage, the tumour group and the histology.Citation15,Citation16
Radical inguinal orchidectomy with high resection of the spermatic cord and radical nephrectomy are the surgical options for paratesticular and renal RMS respectively.Citation2,Citation7,Citation13 Retroperitoneal lymph node dissection is included when there is clinical or radiological evidence of lymphatic spread in the former.Citation2 Traditional chemotherapeutic agents are vincristine, actinomycin-D and cyclophosphamide. Radiation therapy is reserved for high risk group categories.Citation2,Citation11 Unfortunately, we could not re-operate for lymph dissection or give chemotherapy as our patient was lost to follow up most probably due to financial challenges. The alveolar subtype has been shown to have 2 genetic reciprocal translocations PAX3–FOXO1 and PAX7–FOXO1 which is more common in older patients (as in our case) and confers poor prognosis due to high rate of recurrence. We could not do genetic studies in our patient.Citation17 There is a possibility of the renal tumour being metastatic to the testis from retroperitoneal lymphatics retrograde flow as synchronous primary is very rare but the absence of lymph node in the specimens submitted made it unlikely in this case.
Prognosis is dictated by age, tumour site and size, histology, lymph node status and presence or absence of distant metastases.Citation1,Citation2
We considered our patient as a high risk group because of synchronous involvement of left testis and right kidney coupled with his inability to afford health care costs. A survival trend has remained the same in the past decade especially for those considered as high risk group patients.Citation1
Conflict of interest
The authors have no conflict of interest.
Acknowledgements
We wish to acknowledge all staff of Pathology Department of Asokoro District Hospital Abuja, Nigeria; Prof. Ian Roberts and Dr. Godman Greywoode of Oxford University Hospital, Oxford UK for their assistance with the immunohistochemistry and review of the slides.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 15 April 2015
References
- S.OgnjanovicA.M.LinaberyB.CharbonneauJ.A.RossTrends in childhood rhabdomyosarcoma incidence and survivalCancer11518200942184226
- A.FerrariG.BisognoM.CasanovaC.MeazzaL.PivaG.CecchettoParatesticular rhabdomyosarcoma: report from the Italian and German Cooperative GroupJ Clin Oncol2022002449455
- B.J.BrownA.O.OluwasolaChildhood rhabdomyosarcoma in Ibadan, Nigeria: 1984–2003Ann Trop Paediatr2642006349355
- N.MissaouiH.LandolsiL.JaideneA.AnjorinA.B.AbdelkaderM.T.YaacoubiPediatric rhabdomyosarcomas in TunisiaAsian Pac J Cancer Prev115201013251327
- I.A.AdigunG.A.RahmanM.O.BuhariK.O.OgundipeJ.A.OmotayoPattern of rhabdomyosarcoma in Nigerian childrenJ Natl Med Assoc10082008906909
- D.Seleye-FubaraE.N.EtebuJuvenile rhabdomyosarcomas in Port Harcourt, Nigeria: a twelve year reviewWest Afr J Med25120065760
- A.A.BouchikhiS.MellasM.F.TaziK.LahlaidiY.KharbachK.BenhayouneEmbryonic paratesticular rhabdomyosarcoma: a case reportJ Med Case Rep7201393
- B.J.MassonR.KierSonographic and MR imaging appearances of paratesticular rhabdomyosarcomaAJR Am J Roentgenol1711998523524
- A.P.StoutRhabdomyosarcoma of the skeletal musclesAnn Surg1231946447472
- J.G.GurneyJ.L.YoungS.D.RoffersM.A.SmithG.R.BuninSoft tissue sarcomas, SEER pediatric monograph2005National Cancer Institute
- R.J.StewartH.MartelliO.OberlinA.ReyN.BouvetR.D.SpicerTreatment of children with nonmetastatic paratesticular rhabdomyosarcoma: results of the malignant mesenchymal tumors studies (MMT 84 and MMT 89) of the international society of pediatric oncologyJ Clin Oncol2152003793798
- B.RaneyJ.AndersonC.ArndtW.CristH.MaurerS.QualmanPrimary renal sarcomas in the intergroup rhabdomyosarcoma study group (IRSG) experience, 1972–2005: a report from the children’s oncology groupPediatr Blood Cancer5132008339343
- G.M.FarrowE.G.HarrisonJr.D.C.UtzW.H.ReMineSarcomas and sarcomatoid and mixed malignant tumors of the kidney in adults – Part ICancer221968545550
- V.SrinivasP.C.SoganiS.I.HajduW.F.WhitmoreJr.Sarcomas of the kidneyJ Urol13219841316
- W.LawrenceJr.E.A.GehanD.M.HaysM.BeltangadyH.M.MaurerPrognostic significance of staging factors of the UICC staging system in childhood rhabdomyosarcoma: a report from the intergroup rhabdomyosarcoma study (IRS-II)J Clin Oncol5119874654
- W.LawrenceJr.J.R.AndersonE.A.GehanH.MaurerPretreatment TNM staging of childhood rhabdomyosarcoma: a report of the intergroup rhabdomyosarcoma study group. Children’s cancer study group. Pediatric oncology groupCancer806199711651170
- F.T.DenesR.J.DuarteL.M.CristofaniR.J.LopesPediatric genitourinary oncologyFront Pediatr120134810.3389/fped.2013.00048
