Abstract
Post-tuberculosis destroyed lung is a fatal complication of pulmonary tuberculosis which can manifest with severe life-threatening haemoptysis. Its occurrence during pregnancy is rare and challenging because of the significant risk to both the mother and the foetus.
We present an unbooked 36 year old G6P4+1 (4 alive) woman who presented with chronic cough, massive haemoptysis and multiple pregnancy (twin) at 35 week gestation. She had completed anti-tuberculosis treatment twice at and over nine years prior to presentation. On evaluation, there were clinical and radiological evidences of unilateral (right) destroyed lung but no evidence of active tuberculosis; resuscitation was with antibiotics, blood transfusion and oxygen therapy followed by an emergency caesarean delivery due to significant maternal compromise. The symptoms resolved following antibiotic therapy and she was subsequently discharged home. Post-tuberculosis destroyed lung is a fatal uncommon condition that may present during pregnancy and requires a multi-disciplinary specialist care to ensure good maternal and foetal outcome.
1 Introduction
Post-tuberculosis destroyed lung is fatal but preventable; it follows progressive lung parenchymal damage from pulmonary tuberculosis.Citation1,Citation2 It is reappearing consequent to the resurgence of pulmonary tuberculosis following the HIV/AIDS pandemic in the last two decades.Citation2,Citation3 Fawibe et al. reported a 1.3% prevalence for post-tuberculosis unilateral lung collapse among patients attending pulmonology clinic in NigeriaCitation2; however, the incidence of tuberculosis in pregnancy is not readily available in many countries with a report of 4.2 per 100,000 maternities in the United Kingdom.Citation4 A life-threatening complication of post-tuberculosis destroyed lung is massive haemoptysis; when this occurs in pregnancy, it may present a risk for both maternal and neonatal morbidity and mortality. There is no solid evidence that pregnancy has an adverse effect on tuberculosis and an isolated report of successful conservative management of massive haemoptysis with complete unilateral lung collapse from tuberculosis in pregnancy has been reported.Citation5
2 Case presentation
A 36-year old unbooked, G6P4+1 (4 alive) woman with twin pregnancy presented at 35 week gestation with cough (four months) and haemoptysis (15 h). There was weight loss, haemoptysis was 100 ml/episode but no history of anticoagulant therapy. She completed treatment with anti-tuberculosis agents for smear positive PTB eleven and nine years prior to presentation and there was no history of smoking in the couple.
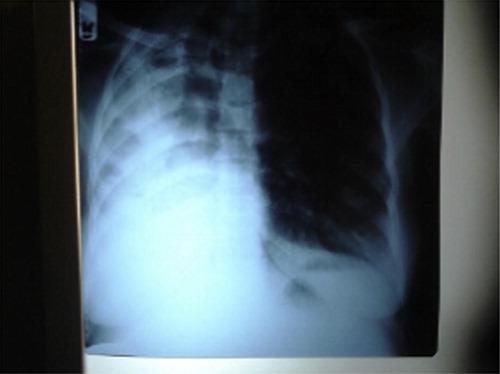
At presentation, temperature was 36.5 °C, no pallor, anicteric with no peripheral lymphadenopathy. Respiratory rate was 22/min; trachea was deviated to the right with coarse crepitations and bronchial breath sounds over right hemithorax. Her pulse rate was 110/min, blood pressure 110/70 mmHg with normal heart sounds. Symphysio-fundal height was 38 cm, leading twin was cephalic and the foetal heart tones were normal. She was nursed in cardiac position, she had oxygen therapy, haemoglobin was 10 g/dl, HIV screening and sputum culture were negative, acid–alcohol fast bacilli were negative on Ziehl-Neelsen staining, and MTB was not detected on sputum GeneXpert test; chest radiograph showed features of destroyed right lung with fibrocystic changes, complete shift of the tracheal air column to the right and compensatory hyperinflation of the left lung (). The assessment was massive haemoptysis from post-tuberculosis destroyed right lung in pregnancy.
Figure 1 Chest radiograph showing features of destroyed right lung with fibrocystic changes, complete shift of the tracheal air column to the right and compensatory hyperinflation of the left lung.
Parenteral Amoxicillin–clavulanate, Metronidazole and cough suppressant were commenced, and her repeat haemoglobin was 7 g/dl after 48 h which necessitated blood transfusion (three units) and emergency caesarean delivery of a set of twins (weight 2.3 kg; 2.0 kg) with good APGAR scores four days after admission; the babies had prophylactic isoniazid for six weeks. Haemoptysis subsided following the treatment; mother and babies were fine on follow-up eight weeks after delivery with plans for pneumonectomy later. The management involved obstetricians, physician, cardio-thoracic surgeon, anaesthesiologist and neonatologist.
3 Discussion
Tuberculosis (TB) associated haemoptysis is a complex condition occurring in old or active TB; it may be due to vascular erosion, bronchiectasis or fungal colonization.Citation6 Management options include conservative management using anti-tuberculosis agents for active TB cases or antibiotics for old inactive cases with bronchiectasis, bronchial artery embolization or surgical intervention especially for those with vascular erosion and antifungal agents for fungal colonization.Citation6 The patient presented had no active TB infection, the features on evaluation suggested bronchiectasis and she improved with antibiotics therapy. The pregnancy was terminated via an emergency abdominal delivery due to maternal compromise from the massive haemoptysis but she and her babies had remained well post-delivery. Pneumonectomy is recommended for destroyed lung but planned surgery is recommended due to higher morbidity and mortality in emergency cases; this explains the postponement in the patient. Destroyed lung is uncommon with the right lungCitation7 and most of the patients are HIV sero-negative as in the case presented.Citation2 This case underscores the rarity of this condition especially in pregnancy, the role of conservative multi-disciplinary care and need for termination of pregnancy if haematocrit falls or haemodynamic instability occurs.
Ethical issues
An informed consent was obtained from the patient to present the case.
Conflict of interest
The authors declare no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 29 April 2015
References
- M.AshourL.PandyaA.MezraqjiUnilateral post-tuberculous lung destruction: the left bronchus syndromeThorax451990210212
- A.E.FawibeA.K.SalamiP.O.OluboyoO.O.DesaluL.O.OdeighaProfile and outcome of unilateral tuberculous lung destruction in Ilorin, NigeriaWest Afr J Med3022011130135
- M.O.LotoI.AwowoleTuberculosis in pregnancy: a reviewJ Preg15201210.1155/2012/379271 Article ID 379271
- M.KnightJ.J.KurinczukC.Nelson-PiercyTuberculosis in pregnancy in the UKBJOG11642009584588
- G.MasukumeE.SengurayiP.MoyoMassive haemoptysis and complete unilateral lung collapse in pregnancy due to pulmonary tuberculosis with good maternal and foetal outcome: a case reportBMC Res Notes6201316
- S.HalezerogluE.OkurThoracic surgery for haemoptysis in the context of tuberculosis: what is the best approach?J Thorac Dis632014182185
- Adefuye BO, Adefuye PO, Ogunkoya OJ. Right destroyed lung in a Nigerian woman with complicated tuberculosis simulating situs inversus. Available at <http://www.atsjournals.org/doi/abs/10.1164/ajrccm>; [accessed 12.12.13].
