Abstract
Introduction
Percutaneous Transhepatic Biliary Drainage (PTBD) is a procedure indicated in patients with non-operative lesions, when endoscopic application of prosthesis is impossible due to anatomic reasons, complications or severe general condition of patient. Most often it is a palliative procedure, aiming for live-quality improvement, although not altering prognosis of basic disease.
Aim
This study presents own experience in biliary drainage with the aid of percutaneous transhepatic method and simultaneous assessment of method effectiveness and safety. The aim was to assess outcomes and complications of PTBD in a large group of patients.
Materials and method
In time period 2007–2014, 167 patients hospitalized in Radiodiagnostics and Radiology Department of Clinical Hospital, were investigated retrospectively. PTBD procedure was applied to patients with biliary tract obstruction. In total 186 procedures of percutaneous drainage were applied. Average age of patients was 63.6 years. Bilirubin, alkaline phosphatase and gamma-glutamyl transferase were measured before and after procedure. All data were analyzed statistically.
Results
In examined group percutaneous drainage was successful in 90.7% interventions. In 8.1% procedures drainage application was ineffective. The most common complication during procedure was hemobilia (3.2%) and the long term complication was drain dislocation (2.7%). The mean bilirubin levels declined from 397.06 μmol/l before drainage to 297.88 μmol/l after drainage (p < 0.05).
Conclusions
PTBD is an effective method of biliary tract decompression and it is an important alternative to endoscopic drainage. This method is indicated in patients with neoplastic obstruction of biliary tract with low expected survival rate and thus is a palliative procedure.
1 Introduction
Two main neoplasms causing obstructive jaundice are pancreas carcinoma and cholangiocarcinoma. Other causes include gall bladder carcinoma, hepatocellular carcinoma, metastases to the liver and advanced carcinoma of stomach or duodenum. Therapy of obstructive jaundice aims at restoring patency of biliary ducts. Thanks to technical and instrumental development of interventional radiology, decompression of biliary ducts is possible []. Percutaneous Transhepatic Biliary Drainage (PTBD) is intended for patients with non-operative lesions, when endoscopic stent application is impossible due to anatomic reasons, complications or severe general state of patient.Citation1,Citation2 In such patients PTBD plays an important role in treatment. Drainage can normalize plasma bilirubin levelCitation3,Citation4 and alleviate jaundice symptomsCitation5, leading to improvement in quality of life, thus optimizing the clinical state of patient allowing for resection or palliative radio or chemotherapy. However, the negative side of this method is a large number of early or late complications as well as necessity of bile delivery to the gastrointestinal tract.Citation5,Citation6 Complications include hemorrhage, cholangitis, hemobilia, biliary duct perforation, peritonitis, edema, sepsis, infection and neoplastic cells spreading among biliary duct.Citation7
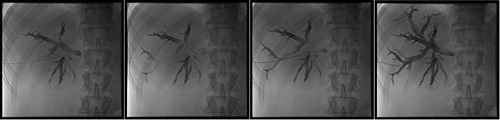
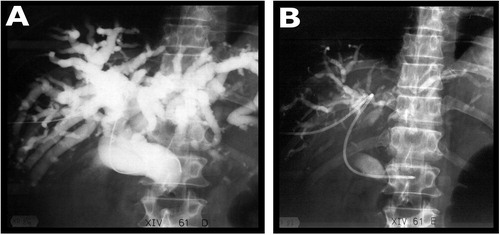
Figure 1 A 67-year-old patient. Percutaneous drainage of biliary ducts carried out on account of inoperable neoplasma infiltration of biliary tract. Fluoroscopy images demonstrating distal CBD obstruction (A) and state of biliary tracts after decompression (B).
Reduction in plasma bilirubin level is usually a significant marker of successful drainage. Nevertheless, in spite of proper catheter positioning in the biliary duct, some patients have poor bile drainage and a high plasma bilirubin level.Citation8 PTBD most often is a palliative procedure, aiming to improve a patients’ quality of life, although not changing the prognosis related to the basic condition.
This paper aims for the assessment of effectiveness and complication numbers in patients with obstructive jaundice treated by PTBD.
2 Materials and methods
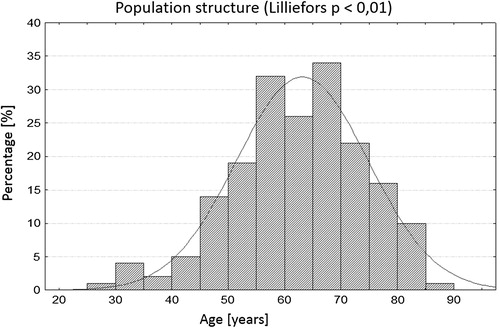
The Department of Radiology of the Central Clinical Hospital performed 186 procedures of Percutaneous Transhepatic Biliary Drainage (PTBD) in the years spanning 2007–2011. The clinical records of patients with obstructive jaundice from the General Surgery Ward and Gastroenterology Ward were analyzed. The study group consisted of 167 patients: 87 females (52%) and 80 males (48%). The average age of women was 62 years and the average age of men was 62 years. Population structure of the study [].
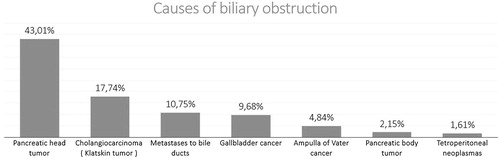
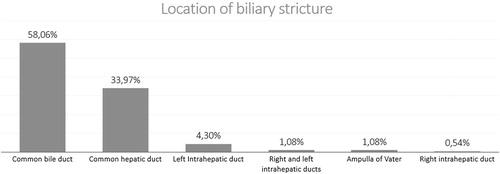
The main indications for PTBD include failed ERCP and patients with conditions that do not qualify for ERCP. Patients who qualified for PTBD were found to have dilated intrahepatic ducts (right hepatic duct or left) of at least 5 mm, which was necessary for the insertion of the catheter without damaging the duct walls. All patients were qualified for the procedure on the basis of imaging tests including ultrasonography, tomography and magnetic resonance imaging. These tests revealed the presence of unresectable tumors and biliary obstructions. All patients achieved histologic confirmation of the neoplastic nature of the change. In our study, the three main unresectable tumors were pancreatic head tumors (43.01%), cholangiocarcinoma (17.7%) and metastases to the bile duct (10.75%) []. The most common location of biliary stricture was the common bile duct (58.06%), common hepatic duct (33.97%) and left bile duct (4.3%) [].
Signs and symptoms of biliary obstruction vary depending on the disease process, history of prior intervention, and comorbidities. In our case the most common sign and symptom was clinical jaundice, which is common with a serum bilirubin over 3 mg/dl. Additionally, to qualify for PTBD patients’ INR had to be within normal limits.
Our patients were monitored carefully for 24 h after drainage. In each case biochemical parameters’ control was carried out.
2.1 Procedure evaluation
Patients abstained from oral intake or were on a clear liquid diet for a minimum 4 h before the procedure. Biliary drainage was performed using conscious sedation. Short-acting benzodiazepines and narcotic agents were applied.
Approach to the right hemiliver was found from the 11th intercostal space in the midaxillary line and on the left from three finger breadths below the xyphoid. When chosen, the site for dermatotomy was anesthetized.
A needle was introduced through the liver into an intrahepatic bile duct to obtain a cholangiogram. Then the needle was removed and another thinner needle with an overlying catheter was inserted. After obtaining bile, the needle was withdrawn but the catheter remained. Then a narrow guide wire was introduced into the bile duct through the catheter.
After positioning the wire in one of the larger bile ducts, the catheter was withdrawn and a Seldinger catheter was introduced over the guide wire. Then the guide wire was withdrawn and the Seldinger catheter was fixed to the skin with a suture [].
3 Results
3.1 Procedure outcomes
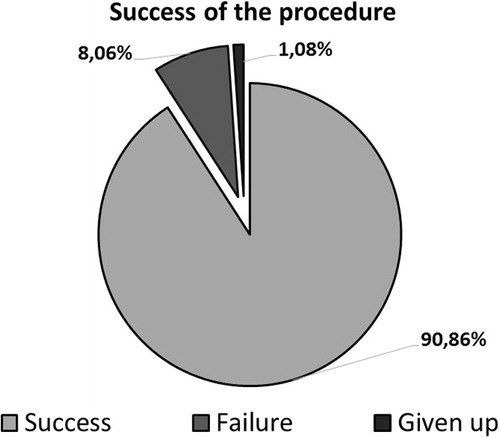
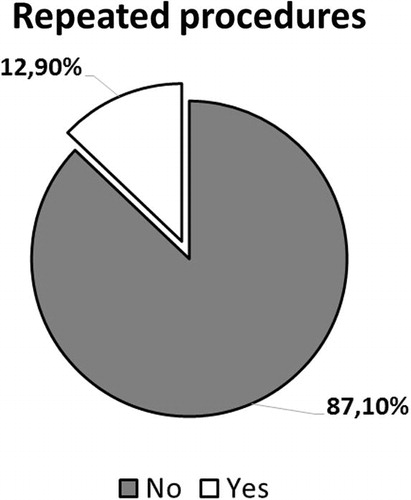
In the study group, 186 procedures of Percutaneous Transhepatic Biliary Drainage (PTBD) were performed on 168 patients. The technical success (hepatic ducts cannulated at the conclusion of the procedure) was achieved in 90.7% of the procedures (n = 168). In 8.1% (n = 15), drainage application was ineffective []. Repeat procedures were required in 24 (12.9%) patients []. In treatment process, 22 patients needed two stages – repeating the PTBD procedure, and the other 2 patients underwent interventions tree times. Two cases (1.08%) withdrew from performing the procedures.
Of all the treatments, 179 (98.78%) procedures were performed on extended bile ducts. In 4 cases, intervention was carried out despite patients not having expanded bile tracts, with two of them achieving technical success. Two others withdrew from performing the procedure.
3.2 Patient outcomes
Laboratory tests were conducted before (last result immediately preceding drainage) and after PTBD in patients to assess their general condition and the effectiveness of treatment. Laboratory tests included total bilirubin, alkaline phosphatase, and gamma-glutamyl transferase.
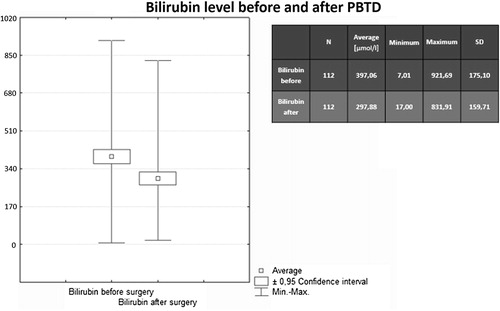
Serum bilirubin values were collected at baseline and during follow-up. Elevated serum bilirubin was noted in 165 (98.31%) of patients. The serum bilirubin level of three patients did not exceed 17.1 μmol/l before the procedure. In 82.14% treatments, decrease of bilirubin was achieved (p < 0.05). The mean value of total bilirubin, presented before procedure of PTBD was 397.06 μmol/l, with a range of 7.01–921.69 μmol/l. The average declined level of bilirubin after percutaneous drainage was to 297.88 μmol/l, with a range of 17.00–831.91 μmol/l [].
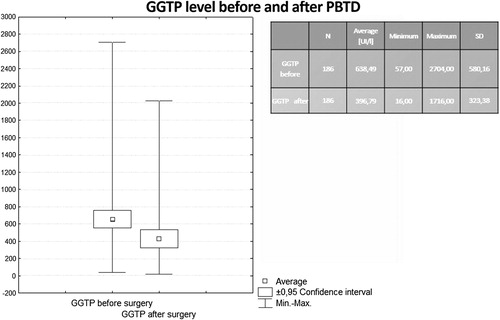
The mean concentration of gamma-glutamyl transpeptidase (GGTP) was found to be 638.49 IU/l, with a range of 57.00–2704.00 IU/l. The decrease of GGTP was observed in 84.62% cases, to an average GGTP level to 396.79 IU/l (range 16.00–1716.00 IU/l) (p < 0.05) [].
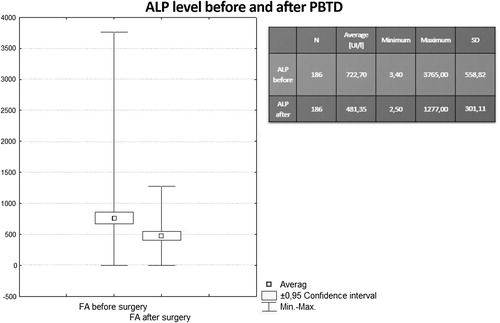
Following biliary drainage there was a decrease of alkaline phosphatase in 86.89%. The mean level of ALP before treatment was 722.70 IU/l and was reduced after percutaneous biliary drainage to an average to 481.35 IU/l (p < 0.05) [].
Percutaneous biliary decompression in the objective assessment found regression of hyperbilirubinemia and reduction of elevated values of GGT and ALP.
3.3 Complications
With proper technique, including peripheral bile duct puncture, serious bleeding complications are uncommon. Since the hepatic artery, portal vein, and bile duct travel side by side within portal triads, it is not unusual for blood to enter the bile duct during catheter fixing, resulting in transient hemobilia.Citation9 It is not surprising that the most common complication stated in the study group was hemobilia.
Any abnormality of a hepatic arterial branch adjacent to the biliary drainage catheter should be taken as presumptive evidence of injury to the branch. Despite prophylactic antibiotic coverage, sepsis may be seen immediately after drainage or within several hours.Citation10
Complications and adverse events occurred in 13.52% (n = 25), documented in patient’s medical record 30 days following procedure. Complications occurred in eleven patients (5.95%) immediately postprocedure (till 24 h). The most common complication during drainage was hemobilia (3.2%). Immediately after the procedure hemobilia was observed in 7 patients – through a drain came out of the bloody content. Perforation of bile ducts appeared in 3 patients (1.62%). One patient, instantly during procedure had a dislocation of the drain [].
Table 1 Complications during the procedure [%].
Long-term complications of PTBD appeared in 7.57% (n = 14). Of these 14 patients, 5 (2.70%) had drain dislocation, 2 (1.08%) reported dysfunction of the drain and 2 (1.08%) had biliary tract hemorrhage to the peritoneal cavity [].
Table 2 Complications after the procedure [%].
3.4 Survival
Mortality in the first week postprocedure was 5.95% (n = 10). In the second week after the treatment two deaths were reported. One patient died within 4 weeks, and also one patient died within 3 weeks of biliary drainage. Two deaths were directly related to PTBD (1 sepsis, 1 hemorrhage). The rest of the deaths were caused by severe general condition and cancer cachexia.
4 Discussion
PTBD is a second-line nonsurgical treatment for patients with malignant biliary obstruction after ERCP failure despite the higher risk of hemorrhage.Citation11–Citation13 The PTBD in our center was successful in 90.86% of the cases. This confirms numbers reported in several studies.Citation11
The main indication for PTBD was pancreatic head tumor (43%), before cholangiocarcinoma (17.7%). Literature points out similar causes of jaundice.Citation14,Citation15 However, it is also important to remember that metastasis to the porta hepatis from many different tumors, can cause malignant biliary obstruction.Citation16 Other indications, like HCC, were shown in different studies.Citation11
After successful PTBD, the total bilirubin level was reduced.Citation14,Citation15,Citation17,Citation18 However, the TBIL levels of patients belonging to the uninfected group were significantly lower compared to those from the infected group.Citation19 In the current study, the average value before the procedure amounted to 23.22 mg% while postprocedure 17.42 mg%. Moreover, both levels of PA and GGTP were reduced after PTBD. Comparable figures were presented in another studyCitation14 where PA levels had been also reduced.
In our case, the most common postprocedure complication was drain dislocation, which also appeared in other studies.Citation11,Citation17 The low percentage of patients with postprocedure hemobilia (1.61%) was confirmed in several published studies.Citation9,Citation14,Citation17,Citation20 However, because of the anatomy of portal triads, the procedure must be performed with suitable technique in order to prevent severe bleeding. Moreover, PTBD should not be performed on patients with nondilated bile ducts, because of high risk of complications. The success rate of PTBD for patients with dilated bile ducts is significantly greater.Citation9,Citation21
Despite prophylactic antibiotics coverage, sepsis can occur right after drainage or within few hours after the procedure.Citation10 In presented case, the number of sepsis and peritonitis reached 1.08%, although other studies show that these can be the most common complications after PTBD.Citation14,Citation15,Citation19
Quality of living does not improve significantly after PTBD, because of high mortality rate in this population and fast progression of the underlying disease.Citation17 Nevertheless, the deleterious effect of pruritus on quality of living can be eliminated by drainage of the biliary ducts.Citation14,Citation17,Citation20
Unfortunately, we were not able to examine the overall survival in our patients. Our numbers showed that 92.47% of patients were discharged, while 7.53% of patients died. The main cause of death was the primary tumor progression. Teixeira et al. reported that the median survival period after PTBD was 2.9 months.Citation13 Many studies involving patients with malignant biliary obstruction show similar values.Citation2,Citation12,Citation22
Final conclusion
| 1. | PTBD is an effective method of biliary tract decompression and it is an important alternative to endoscopic drainage. | ||||
| 2. | Percutaneous drainage of biliary ducts decompresses mechanical jaundice and decreases typical serum markers of cholestasis. | ||||
| 3. | PTBD is indicated in patients with neoplastic obstruction of biliary tract with low expected survival rate and thus is a palliative procedure. | ||||
Conflict of Interest
There are no conflicts of interest to declare for this study. It was not financed by external funding.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 19 August 2015
References
- H.G.CoonsSelf-expanding stainless steel biliary stentsRadiology1701989979
- M.SutR.KennedyJ.McNameeLong-term results of percutaneous transhepatic cholangiographic drainage for palliation of malignant biliary obstructionJ. Palliat. Med.1320101311
- J.T.FerruciP.R.MuellerW.P.HarwimPercutaneous transhepatic biliary drainageRadiology1351980113
- C.HellekantK.JonssonS.GerllPercutaneous internal drainage in obstructive jaundice: experimental and clinical aspectsBr. J. Surg.801993834842
- M.KarasekJ.GarcarekK.JarnickiPowikłania po przezskórnym drenażu dróg żółciowychPol. Przegl Radiol.621997187189
- B.CiesielczykM.SkommerAlgorytm postępowania po przezskórnym drenażu dróg żółciowychPol. Przegl Chir.2002713721
- M.J.KangY.S.ChoiJ.Y.JangCatheter tract recurrence after percutaneous biliary drainage for hilar cholangiocarcinomaWorld J. Surg.377201317431744
- R.RerknimitrN.KladcharoenV.MahachaiResult of endoscopic biliary drainage in hilar cholangiocarcinomaJ. Clin. Gastroenterol.382004518523
- A.M.CoveyK.T.BrownPercutaneous transhepatic biliary drainageTech. Vasc. Interv. Radiol.11120081420
- T.P.SmithJ.M.RyanSepsis in the interventional radiology patientJ. Vasc. Interv. Radiol.152004317325
- M.YasunoriK.MasatoshiHepatocellular carcinoma with obstructive jaundice: endoscopic and percutaneous biliary drainageDig. Dis.3062012592597 (13)
- S.S.SalujaM.GulatiP.K.GargEndoscopic or percutaneous biliary drainage for gallbladder cancer: a randomized trial and quality of life assessmentClin. Gastroenterol. Hepatol.62008944950
- O.M.van DeldenJ.S.LamerisPercutaneous drainage and stenting for palliation of malignant bile duct obstructionEur. Radiol.182008448456
- AndrzejFedakWojciechUchtoAndrzejUrbaniakTranscutaneal drainage intrahepatic biliary ducts as a method of paliative treatment of inoperative liver hilum tumoursPrzegląd Lekarski7020135
- M.C.TeixeiraM.P.MakD.F.MarquesPercutaneous transhepatic biliary drainage in patients with advanced solid malignancies: prognostic factors and clinical outcomesGastrointest. Cancer442013398403
- Z.DambrauskasS.PaskauskasP.LizdenisPercutaneous transhepatic biliary stenting: the first experience and results of the Hospital of Kaunas University of MedicineMed (Kaunas)442008969976
- P.C.RobsonN.HeffernanM.GonenProspective study of outcomes after percutaneous biliary drainage for malignant biliary obstructionAnn. Surg. Oncol.17201023032311
- K.ObholzerM.B.PittonP.MildenbergerThe current value of percutaneus transhepatic biliary drainageRofo Fortschr Geb Romntgenstr Neuen Bildgeb Verfahr17420021081
- Ch.XuP.H.LvX.E.HuangInternal-external percutaneous transhepatic biliary drainage for patients with malignant obstructive jaundiceAsian Pac. J. Cancer Prev.1521201493919394
- N.S.AbrahamJ.S.BarkunA.N.BarkunPalliation of malignant biliary obstruction: a prospective trial examining impact on quality of lifeGastrointest. Endosc.562002835841
- G.CozziA.SeveriniE.CivelliPercutaneous transhepatic biliary drainage in the management of postsurgical biliary leaks in patients with nondilated intrahepatic bile ductsCardiovasc. Intervent. Radiol.2932006380388
- M.IwasakiJ.FuruseM.YoshinoPercutaneous transhepatic biliary drainage for the treatment of obstructive jaundice caused by metastases from nonbiliary and nonpancreatic cancersJpn. J. Clin. Oncol.261996465468