Abstract
Mycoplasma hominis (MH) and Ureaplasma urealyticum (UU) are important members of genital Mycoplasmas. They are implicated in urogenital infections and complicated pregnancy (chorioamnionitis, preterm delivery, abortion, and preterm birth) as well as bacterial vaginosis and cervicitis. The administration of antimicrobial agents to pregnant women with preterm rupture of the membranes (PROM) may extend the gestation period and decrease the risks of associated complications and neonatal infections. Despite empirical therapy is the rule in cases suspected to have genital infection in Egypt, the surveillance of the susceptibilities of used antibiotics is mandatory to ensure treatment efficacy and good prevention of any possible complications. This study aimed to assess the infection rate of genital Mycoplasmas (MH and UU) among pregnant females and their antimicrobial susceptibility pattern to provide a provisional idea about the effectiveness of antibiotics used empirically to treat cases of genital infections in pregnant women. High vaginal swabs of 50 pregnant females were examined using Mycoplasma IES kit, for identification of UU and MH. The kit also provides the antimicrobial susceptibility results for 12 antimicrobials of five different classes. UU and MH were detected in 26/50 (52%), and 7/50 (14%) of cases respectively, of which 5 cases showed mixed infection with both organisms. UU was most sensitive to quinolones (90–95%), followed by tetracyclines (80–85%). The least sensitivity was detected with chloramphenicol and clindamycin (40% and 30% respectively). The two MH isolates (100%) were sensitive to the three tested quinolones in addition to clindamycin and thiamphenicol. MH showed 100% sensitivity to clindamycin and 75% of UU isolates were sensitive to azithromycin. Further studies are needed to detect any future changes in the susceptibility pattern for these drugs or other antibiotics.
1 Introduction
Mycoplasma hominis (MH) and Ureaplasma spp., including Ureaplasma parvum and Ureaplasma urealyticum (UU) are collectively known as genital Mycoplasmas. They are found in the genital milieu of up to 80% of pregnant and non-pregnant women.Citation1
M. hominis-as a common commensal of the female genital tract- has been associated with pyelonephritis, bacterial vaginosis, cervicitis, endometritis, PID and postpartum septicemia. U. urealyticum is considered as the main cause of non-chlamydial, non-gonococcal urethritis, chorioamnionitis, preterm delivery, abortion, preterm birth, bacterial vaginosis and cervicitis.Citation2–Citation4 The administration of antimicrobial agents to pregnant women with preterm rupture of the membranes (PROM) may extend the gestation period and decrease the risks of associated complications and neonatal infections.Citation5,Citation6
Bacterial resistance to routine antimicrobial agents is a growing and a worldwide problem. The lack of a rigid cell wall renders genital Mycoplasmas innately resistant to antimicrobial agents, such as β-lactam antibiotics and vancomycin.Citation7 Although macrolides are often the drugs of choice for treating these infections, M. hominis is intrinsically resistant to the C14 and C15 macrolides (e.g. erythromycin and azithromycin).Citation8 Ureaplasma species also have natural resistance to lincosamides (e.g. clindamycin); observed resistance to macrolides is associated with mutations in the 23S rRNA gene.Citation9,Citation10 Mycoplasma and Ureaplasma infections are usually treated with tetracycline, except in neonates or children – during the first 6 years of life-in whom the drug is deposited in bony structures and teeth causing discoloration. It occurs also in newborns of mothers who received tetracyclines for long periods during pregnancy. Tetracyclines may also cause hepatic damage or severe vestibular toxicity. Instead, erythromycin is recommended.Citation11 However, the amniotic sac is not effectively penetrated by erythromycin and Ureaplasmas are not eradicated from the vagina or cervix by this agent. Newer macrolides (e.g. azithromycin and clarithromycin) allow for better tolerability and the once daily dosing benefit can increase compliance. Treatment with azithromycin is equally successful compared to erythromycin but with fewer side effects.Citation6
The increase in resistance of genital Mycoplasmas to antimicrobial agents has prompted the implementation of ongoing surveillance studies.
2 Aim of the work
The aim of the present study was to assess the infection rate and antimicrobial susceptibilities of these two sexually transmitted pathogens M. hominis and U. urealyticum among a group of Egyptian pregnant women attending antenatal care clinic.
3 Subjects and methods
3.1 Subjects
This cross-sectional study included 50 pregnant females aged >18 years, attending the antenatal care clinic – Gynecology and Obstetrics Hospital – Faculty of Medicine – Ain Shams University, from January 2015 to June 2015. All women enrolled in the study gave informed written consent prior to their participation. Data collected from participants included age, gestational age, the presence or absence of any symptoms suggesting of vaginitis (change in amount of vaginal secretion with changing in odor or color and itchy vaginal irritation), samples were collected and laboratory work was conducted in Medical Microbiology and Immunology Department- Faculty of Medicine- Ain Shams University. The only exclusion criterion was antimicrobial intake 3 weeks prior to the sample collection time.
3.2 Samples collection
High vaginal swabs were taken from each subject enrolled in the study using sterile cotton swabs. Each swab was inoculated to one diluent vial (provided by the kit). Diluent vials were then recapped and sent to the Medical Microbiology and Immunology Department laboratory for processing.
3.3 Genital Mycoplasmas detection and antimicrobial susceptibility testing
3.3.1 Principle of the test
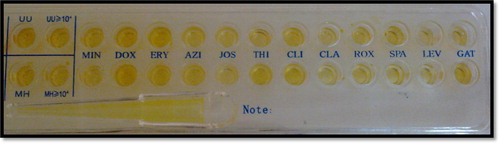
Genital Mycoplasmas detection and antimicrobial susceptibility testing were done using Mycoplasma Culturing, Identification, Enumeration, and Susceptibility Kit (Mycoplasma IES kit – Autobio Diagnostics – China). Mycoplasma IES kit is based on cultivation and biochemical reactions. Urea is decomposed by the urease enzyme produced by U. urealyticum with release of NH3. For detection of M. hominis, arginine is decomposed by Arginase enzyme-produced by the organism- and releases NH3. Then NH3 causes an increased pH of the liquid medium. The corresponding color change of the indicator was used to judge the result. The susceptibility strip contains 12-antibiotics, each one in two concentrations . If Mycoplasma was sensitive to an antibiotic, the activity of the enzyme was inhibited causing no change in color. Types and concentrations of tested antibiotics are summarized in . The kit also provides further data about the detected organism either there is colonization (<104 CFU) or infection (>104 CFU).
Table 1 Types and concentrations of tested antibiotics.
3.3.2 Procedure
Culture media were prepared by mixing the freeze-dried powder vial (peptone of bovine origin and beef heart infusion) and the inoculated diluent vials (both provided by the kit).
The procedure was done according to the manufacturer’s instructions. Each inoculated diluent vial was added to one of the freeze-dried powder vials (both were provided by the kit). After well shaking and complete dissolution, 100 μl of the mixture was added to each well of the strip by automatic pipetting. Strip was then shaken gently then each well was covered with one drop of mineral oil. The strip was then covered and incubated at 37 °C for 24 h. Change in color of the well to red color indicated positive reaction and microbial growth .
4 Results
The present study was conducted on 50 pregnant females attending the antenatal care clinic of Ain Shams University Gynecology and Obstetrics Hospital. Their ages ranged from 16 to 35 with a mean of 25.3 ± 4.99. The gestational age ranged from 10 to 36 weeks with a mean of 25 ± 6.23. History of symptoms suggesting for vaginal infection was recorded, and only 10 females (20%) gave history of symptoms.
Using Mycoplasma IES kit, Out of the 50 vaginal swabs, 28 cases (56%) were positive for either M. hominis, U. urealyticum or both. Of these 28 cases, 5 cases showed mixed infection of both organisms .
Table 2 Demographic data and infection percentage among the studied cases.
26 isolates of U. urealyticum were detected (52%) of total swabs. Among these 26 isolates positive for U. urealyticum, 5 cases (10%) represented colonization (<104 CFU), and 21 cases (42%) represented infection (>104 CFU) .
Only 7 isolates of M. hominis were detected (14%) of total cases. The 7 cases represented infections (>104 CFU) .
No significant correlation was detected between symptoms suggesting of genital infection and the presence of either colonization, infection with U. urealyticum or infection with M. hominis, and p values were 0.23, 0.2, and 0.68 respectively.
Antimicrobial susceptibility testing was performed by the kit for both organisms for 12 antibiotics of 5 categories: Macrolides [roxithromycin (ROX), azithromycin (AZI), josamycin (JOS), clarithromycin (CLA), and erythromycin (ERY)], quinolones [sparfloxacin (SPA), levofloxacin (LEV), gatifloxacin (GAT)], tetracyclines [doxycycline (DOX), minocycline (MIN)], chloramphenicols [thiamphenicol (THI)], and lincosamides [clindamycin (CLI)].
Antimicrobial susceptibility testing could not be done to the isolates from the five cases of mixed infection. Susceptibility testing results could not be read clearly in one out of the 21 isolates of U. urealyticum, which may be due to the low organism load in this case. shows the results of antimicrobial sensitivity of the 20 isolates of UU and 2 isolates of MH.
Table 3 Results of antimicrobial susceptibility among isolates of both Mycoplasma hominis and Ureaplasma urealyticum.
The results of antimicrobial sensitivity testing revealed that UU isolates were most sensitive to the tested quinolones with sensitivity rates 90%, 95% and 90% for sparfloxacin, levofloxacin and gatifloxacin respectively. This was followed by tetracyclines with sensitivity rates of 80% and 85% for doxycycline and minocycline respectively. Regarding the group of tested macrolides, the sensitivity rates ranged from 45% for erythromycin and 75% for azithromycin and clarithromycin. The least sensitivity rates were for clindamycin (30%) and thiamphenicol (40%).
For the isolates of MH, the 2 isolates (100%) were sensitive to the 3 tested quinolones in addition to clindamycin and thiamphenicol.
5 Discussion
M. hominis, U. urealyticum and Mycoplasma genitalium are the mollicutes (class of bacteria lacking cell walls) most frequently isolated in the genital tract and the most potentially pathogenic. They are associated with pelvic inflammatory disease, urethritis, salpingitis, bacterial vaginosis, infertility, ectopic pregnancy, obstetric pathologies (spontaneous abortion, preterm delivery and puerperal infections) as well as perinatal disorders (low birth weight, respiratory and neurological infections).Citation12 Culture of Mycoplasma is labor intensive and time consuming, as it requires the use of an enrichment broth for up to seven days, followed by sub-culturing on solid media. Analytical sensitivities in the range of 60% are only obtained in skilled laboratories and identification is restricted to the genus level. The development of commercially available diagnostic assays, which are based on liquid broth cultures provides easy to use and faster alternatives to conventional culture methods for the detection of genital Mycoplasmas.Citation13 In the present study, identification and antimicrobial susceptibility testing of genital Mycoplasmas were performed using the Mycoplasma Culturing, Identification, and Enumeration, Susceptibility Kit (Mycoplasma IES kit) as a rapid and simple phenotypic based diagnostic method.
In the present study, 26 isolates of U. urealyticum were detected in 26 out of 50 samples (52%), while M. hominis was only isolated from 7 (14%) of the samples, of which 5 (10%) isolates were mixed with UU; similar to our results Zhu et al.Citation14 in their study reported an overall positive incidence of genital Mycoplasmas of 62.16%. The most common pattern was UU monoinfection (46.52%), the UU–MH coinfection pattern ranked second (13.91%) and MH monoinfection was the lowest (1.71%).
The prevalence of genital Mycoplasmas varied widely in different reports. In a study by Sobouti et al.Citation15, vaginal colonization among a group of recent mothers was found to be 15% (25/165) for U. urealyticum and 15% (25/165) for M. hominis. A lower percentage was reported by Bayraktar et al.Citation1 who examined samples from one hundred pregnant women, they successfully cultured M. hominis in five women (5%) and U. urealyticum in 27 (27%), and they reported simultaneous colonization with both M. hominis and U. urealyticum in 6% of symptomatic patients.
A higher rate of detection of both organisms was reported by Redelinghuys et al.Citation6, and they found that 76% (73/96) of specimens contained Ureaplasma spp., with also a higher percentage of simultaneous colonization with M. hominis [39.7% (29/73)].
In a study by Kechagia et al.Citation8 U. urealyticum was grown as a single pathogen in 65 (47.44%) out of specimens, while M. hominis was grown as a single pathogen in 0.72% and in 2.92% both urogenital Mycoplasmas were grown.
Earlier studies reported colonization rate with U. urealyticum ranging between 10% and 50% of women, and colonization rates with M. hominis of less than 30%.Citation16,Citation17
The discrepancy in prevalence rates can be attributed to the different study populations and the different detection methods.Citation12 The type of assay may have an effect on the accurate detection of genital Mycoplasmas, depending on the growth factors and antimicrobial agents included in the media of the commercial assay.Citation13
Using quantitative PCR by Campos et al.Citation18 increased the isolation rate of M. hominis and M. genitalium to 31.8% and 28.1%, respectively, also using multiplex PCR increased the detection rate of genital Mycoplasmas up to 84% (185/220) as reported by Redelinghuys et al.Citation19
In the present study, no significant correlation was determined between the detection of genital Mycoplasma and the symptoms of the cases. This is similar to the results of Redelinghuys et al.Citation6 as they reported that symptoms were vague and subjective and did not correlate with the study results, and the women could not definitely distinguish between a physiological discharge and an unusual vaginal discharge.
Although agar and broth dilution methods may be used to determine antibiotic susceptibilities, the complex growth requirements of Mycoplasmas have restricted their performance.Citation20 In the present study, the Mycoplasma IES kit showed that UU isolates were most sensitive to the tested quinolones with sensitivity rates 90–95%, followed by tetracyclines with sensitivity rates of 80% and 85%. Regarding the group of tested macrolides, the sensitivity rates ranged from 45% for erythromycin to 75% for azithromycin and clarithromycin. The least sensitivity rates were for clindamycin (30%) and thiamphenicol (40%).
There was a wide range of variability in the results of antimicrobial sensitivity of different antimicrobial categories. In agreement with our results, Redelinghuys et al.Citation6 reported susceptibilities of Ureaplasma spp. to levofloxacin and moxifloxacin of 59% (26/44) and 98% (43/44) respectively. In addition, Krausse and SchubertCitation21 reported that Ofloxacin was effective against U. urealyticum (>95% susceptibility), but ciprofloxacin was less active with a sensitivity of 35.2%.
In contrast to the results of the present study, Bayraktar et al.Citation1 found the highest drug resistance rates in U. urealyticum were 92.6% to ciprofloxacin and 85.2% to ofloxacin. In another study, Leli et al,Citation22 found that 66.4% (101/152) of U. urealyticum isolates were resistant to ciprofloxacin, whereas 27.6% (42/152) were resistant to ofloxacin. In addition, Kechagia et al.Citation8, in their work found that ciprofloxacin and ofloxacin were inactive against most of the isolated strains.
Despite the high sensitivity of quinolones reported in the present study, Fluoroquinolones are classified as category C agents and the use of these agents in pregnancy is controversial.Citation6,Citation23
Similar to the results of the present study regarding sensitivity to tetracyclines, Kechagia et al.Citation8 found that 87.4% and 98.2% of the isolated U. urealyticum strains were susceptible to tetracycline and doxycycline, respectively. Tetracyclines were also most effective against isolated U. urealyticum (sensitivity rates of 81–100%) according to Koh et al.Citation24, Bayraktar et al.Citation1, Krausse and SchubertCitation21, and Leli et al.Citation22
In contrast to these results, Redelinghuys et al.Citation6 reported the susceptibility of Ureaplasma isolates to tetracycline was found to be 27%.
Regarding sensitivity to macrolides, Krausse and SchubertCitation21, and Bayraktar et al.Citation1 reported a very high sensitivity of U. urealyticum isolates especially to josamycin which is a novel drug. However, in the study of Kechagia et al.Citation8 they reported that only 79.2% of isolates were susceptible to josamycin, while erythromycin and azithromycin, proved to be inactive against most of the strains.
The use of erythromycin in pregnant women has permitted the surveillance of long-term effects of this antimicrobial agent. These include infantile hypertrophic pyloric stenosis, cardiac toxicity and maternal hepatotoxicity. There is not enough data available to know whether the risks of toxicity in neonates are similar with newer macrolide antimicrobial agents. It was suggested that if the price of azithromycin in many countries decreases to an affordable level, it might potentially replace erythromycin as a general treatment option in the future. The treatment options of genital Mycoplasmas in pregnancy therefore remain limited.Citation7,Citation6
In the present work, the 2 isolates of M. hominis (100%) were sensitive to the 3 tested quinolones in addition to clindamycin and thiamphenicol, and other drugs showed 0% or 50% sensitivity. In agreement with our results, Bayraktar et al.Citation1 reported that M. hominis was more sensitive to quinolones and naturally resistant to erythromycin. In contrast to our results, they also reported a potent activity of josamycin against M. hominis.
Similarly, Bayraktar et al.Citation1 found that among M. hominis, the highest drug resistance rate was 100% to erythromycin, while No resistance was observed to josamycin, although some strains had intermediate resistance.
Different results were reported by Kechagia et al.Citation8 who found that M. hominis isolates were 100% susceptible to tetracycline, doxycycline and pristinamycin, while susceptibilities to the other antimicrobial agents varied mainly in the range of ‘intermediate’ or ‘resistant’.
Krausse and SchubertCitation21 in their study reported that doxycycline was the most active tetracycline against M. hominis, with resistance rate approximately 10–13%. Ofloxacin was also effective (>95% susceptibility). Ciprofloxacin was moderately active against M. hominis (70.3% susceptibility). The wide range of variability in the antimicrobial susceptibility patterns can be attributed to the different antimicrobial-use policies, which lead to the emergence of resistance to one or other antimicrobial group. Other variables contributing to this discrepancy might include the population studied, the study period, or the kits used for specimen processing and analyses.Citation6
Although this research involves a short study period and does not include a representative population sample (its main limitations), to our knowledge it is the first study carried out locally in Gynecology and Obstetrics Hospital – Faculty of Medicine – Ain Shams University on this topic. Thus, further research is needed to see whether these results hold for the larger population; such research will require a larger sample size and full access to clinical, epidemiological and microbiological variables. In the present study, MH showed 100% sensitivity to clindamycin and 75% of UU isolates were sensitive to azithromycin. Both drugs are used empirically during pregnancy. Further studies are recommended to detect any changes in the susceptibility pattern for these drugs or other antibiotics that will affect the effectiveness of treatment.
6 Conclusions
Despite empirical therapy is important in the treatment of Mycoplasmas, the discrepancies in antimicrobial sensitivity patterns in different countries make it uncertain to establish common guidelines for the empirical treatment of genital Mycoplasmal infections.
In the present study, MH showed 100% sensitivity to clindamycin and 75% of UU isolates were sensitive to azithromycin. Both drugs are used empirically during pregnancy. Further studies are recommended to detect any changes in the susceptibility pattern for these drugs or other antibiotics that will affect the effectiveness of treatment.
Effective treatment depends on the antimicrobial susceptibilities of genital Mycoplasmas in a specific region. Routine monitoring is mandatory to ensure the efficacy of treatment.
The implementation of rational treatment regimens that requires the in vitro determination of the antimicrobial susceptibility of the isolated genital Mycoplasmas in each clinical case is now a simple routine laboratory procedure using commercially available systems.
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 17 February 2016
References
- M.R.BayraktarI.H.OzerolN.GucluerO.CelikPrevalence and antibiotic susceptibility of Mycoplasma hominis and Ureaplasma urealyticum in pregnant womenInt J Infect Dis142010e90e95
- L.FalkH.FredlundJ.JensenSigns and symptoms of urethritis and cervicitis among women with or without Mycoplasma genitalium or Chlamydia trachomatis infectionSex Transm Infect8120057378
- N.AmirmozafariR.MirnejadB.KazemiE.SaririM.R.BojariF.D.DarkahiComparison of polymerase chain reaction and culture for detection of genital Mycoplasma in clinical samples from patients with genital infectionsSaudi Med J30200914011405
- B.D.TaylorT.DarvilleC.L.HaggertyDoes bacterial vaginosis cause pelvic inflammatory disease?Sex Transm Dis402013117122
- C.H.Raynes-GreenowC.L.RobertsJ.C.BellB.PeatG.L.GilbertS.ParkerAntibiotics for Ureaplasma in the vagina in pregnancyCochrane Database Syst Rev9201111810.1002/14651858.CD003767 CD003767
- M.J.RedelinghuysM.M.EhlersA.W.DreyerH.A.LombaardM.M.KockAntimicrobial susceptibility patterns of Ureaplasma species and Mycoplasma hominis in pregnant womenBMC Infect Dis142014171176
- K.B.WaitesB.KatzR.L.SchelonkaMycoplasmas and Ureaplasmas as neonatal pathogensClin Microbiol Rev182005757789
- N.KechagiaS.BersimisS.ChatzipanagiotouIncidence and antimicrobial susceptibilities of genital Mycoplasmas in outpatient women with clinical vaginitis in Athens, GreeceJ Antimicrob Chemother622008122125
- M.DongyaX.WenchengM.XiaoboW.LuTransition mutations in 23S rRNA account for acquired resistance to macrolides in Ureaplasma urealyticumMicrob Drug Resist142008183186
- L.XiaoD.M.CrabbL.B.DuffyV.ParalanovJ.I.GlassD.L.HamilosMutations in ribosomal proteins and ribosomal RNA confer macrolide resistance in human Ureaplasma sppInt J Antimicrob Agents372011377379
- B.B.MardassiN.AissaniI.MoallaD.DhahriA.DridiB.MlikEvidence for the predominance of a single tet (M) gene sequence type in tetracycline-resistant Ureaplasma parvum and Mycoplasma hominis isolates from Tunisian patientsJ Med Microbiol61201212541261
- L.DíazL.E.CabreraT.FernándezI.IbáñezY.ObregónY.TorresFrequency and antimicrobial sensitivity of Ureaplasma urealyticum and Mycoplasma hominis in patients with vaginal dischargeMEDICC Rev15420134647
- M.J.RedelinghuysM.M.EhlersA.W.DreyerH.LombaardM.M.KockComparison of the new Mycofast revolution assay with a molecular assay for the detection of genital Mycoplasmas from clinical specimensBMC Infect Dis132013453
- C.ZhuJ.LiuY.LingC.DongT.WuX.YuPrevalence and antimicrobial susceptibility of Ureaplasma urealyticum and Mycoplasma hominis in Chinese women with genital infectious diseasesIndian J DermatolVenereol Leprol783201240640710.4103/0378-6323.95480
- B.SoboutiS.FallahM.MobayenS.NoorbakhshY.GhavamiColonization of Mycoplasma hominis and Ureaplasma urealyticum in pregnant women and their transmission to offspringIranian J Microbiol642014219224
- D.DominguesL.TávoraTaviraA.DuarteA.SancaE.PrietoF.ExpostoGenital mycoplasmas in women attending a family planning clinic in Guinea-Bissau and their susceptibility to antimicrobial agentsActa Trop8620031924
- F.E.KeaneB.J.ThomasC.B.GilroyA.RentonD.Taylor-RobinsonThe association of Mycoplasma hominis, Ureaplasma urealyticum and Mycoplasma genitalium with bacterial vaginosis: observations on heterosexual women and their male partnersInt J STD AIDS112000356360
- G.B.CamposN.N.SelisT.N.LobãoA.T.AmorimH.B.MartinsM.S.BarbosaPrevalence of Mycoplasma genitalium and Mycoplasma hominis in urogenital tract of Brazilian womenBMC Infect Dis20151560
- M.J.RedelinghuysM.M.EhlersA.W.DreyerH.LombaardS.A.OlorunjuM.M.KockA cross-sectional study on the relationship of age, gestational age and HIV infection to bacterial vaginosis and genital mycoplasma infectionBMJ Open520159
- B.A.ForbesD.F.SahmA.S.WeissfeldCell wall-deficient bacteria: Mycoplasma and Ureaplasma12th ed.Baily’sScottDiagnostic microbiology2007Elsevier525
- R.KrausseS.SchubertIn-Vitro activities of tetracyclines, macrolides, fluoroquinolones and clindamycin against Mycoplasma hominis and Ureaplasma ssp. isolated in Germany over 20 yearsClin Microbiol Infect16201016491655
- C.LeliA.MencacciJ.C.BombaciF.D’AlòS.FarinelliM.VitaliPrevalence and antimicrobial susceptibility of Ureaplasma urealyticum and Mycoplasma hominis in a population of Italian and immigrant outpatientsInfez Med20220128287
- F.Sá DelFiolM.GerenuttiF.C.GroppoAntibiotics and pregnancyPharmazie602005483493
- E.KohS.KimI.KimK.MaengS.LeeAntimicrobial susceptibilities of Ureaplasma urealyticum and Mycoplasma hominis in pregnant womenKorean J Clin Microbiol122009159162