1 Introduction
Otodystrophy of the otic capsule or what is known as otosclerosis (OS) is seen located in the majority of patients in the anterior aspect of the oval window or what is known as the fissula ante fenestrum.Citation1 Patients usually present between the ages of 10 and 40 with hearing loss whether conductive, sensorineural or mixed hearing loss; depending on the type of otosclerosis.Citation2 There are two types of otosclerosis; fenestral and retrofenestral. The classical clinical findings are an intact tympanic membrane with no signs of middle ear inflammation, progressive conductive hearing loss (CHL) and absent stapedial reflexes.Citation3–Citation7
Usually, clinicians do not proceed to imaging those patients with the typical clinical picture. A Stapedectomy with stapes prosthesis is the treatment of choice for fenestral otosclerosis.Citation3–Citation7
Since its introduction into otology, the computed tomographic (CT) scan has been shown to be a useful instrument for diagnosis of otosclerosis.Citation3 Many studies found a reliability of more than 90% in the diagnosis of otosclerosis.Citation3
The temporal bone is fully imaged with no need for intravenous contrast material. Axial images best demonstrate the lucent spongiotic fenestral otosclerotic foci because of the location of the footplate of stapes as well as that of the oval window.Citation2
Stapedectomy usually involves stapes prosthesis insertion in an aim to improve hearing by removing the fixed stapes bone and replacing it with a microprosthesis. Prosthesis insertion may be linked to a few built-in problems such as outward displacement or inward protrusion of the prosthesis into the vestibule, granuloma development to the more serious complications as labyrinthitis or perilymphatic fistulas. HRCT is the modality of choice as it accurately shows the position of the prosthesis and helps to exclude other complications mentioned above. Because of the hyperdensity of the prosthesis, it can be easily identified on HRCT. However, MRI may be needed as a supplementary study to exclude labyrinthitis or fibrotic changes within the labyrinth.Citation4,Citation5,Citation8–Citation10
Aim of this study is to assess the importance and utility of both CT and MRI in the evaluation of poststapedectomy complications and to properly select the right imaging modality according to the suspected clinical postoperative complication.
2 Materials and methods
2.1 Patients
From September 2015 to July 2016, we evaluated twenty patients; including 12 females and 8 males, aged 31–64 years old, with a mean age of 47.5. They were all referred from the ENT surgical department. All are known cases of otosclerosis with history of stapedectomy, ranging from 4 weeks to 2 years ago. Their clinical presentation included hearing loss (8 cases), vertigo (7 cases) and routine follow up (5 cases). Onset of symptoms ranged from 4 weeks following the operation to up to 2 years later.
CT was done for all the 20 patients followed by an MRI study for only two patients where CT showed no well-defined cause and labyrinthitis was suspected. CT/MR diagnosis was correlated with the clinical diagnosis and the operative findings as the standard of reference. The study was supported by the ethical board of our institution.
2.2 Imaging technique
MDCT examinations were performed with Siemens Somatom Definition Flash, 128 slice combined with Advantage Workstation GE; parameters consisted of a voltage of 120 kV, a current of 240 mA, FOV 16cm, pitch/speed 1, and a rotation time 1, no gantry tilt: 0, slice thickness 0.4 mm at 0.4 mm interval, patient position: supine. No intravenous contrast was given to the patients in the routine study. Acquisition of ultra-thin axial cuts was done using a multidetector CT machine, with reformats taken in both coronal and sagittal planes with respect to the lateral semicircular canal. MRI was done for only 2 patients around 5–7 days after CT imaging. Stapedectomy is not a contraindication for doing an MRI. MRI was performed on a 3 T unit. The conventional T1 and T2 weighted sequences were done with a slice thickness of 2 mm. Both axial as well as coronal planes were taken, for better spatial assignment. T1- weighted sequence following IV contrast administration was also acquired. A 3D high resolution heavily T2 weighted submillimetre was then followed to allow evaluation of the facial vestibulo-cochlear nerve complex and for detection of alterations in the labyrinth.
2.3 Images interpretation
All images were reviewed and analyzed by two radiologists. CT interpretation included a comment on the position of the stapes prosthesis for either migration or protrusion, exclusion of perilymphatic fistula and labyrinthitis ossificans as well as middle ear assessment for any soft tissue lesions. MRI interpretation included evaluation of T1 and T2 signal intensity as well as postcontrast enhancement of the membranous labyrinth.
3 Results
A total of 20 symptomatic patients poststapedectomy were submitted for Multidetector CT examination with 2 of the cases followed by an MRI study. Seven (35%) patients showed medial migration of the prosthesis into the vestibule (). Six (30%) patients were diagnosed as outward protrusion of the prosthesis (). Two patients (10%) showed a perilymphatic fistula (). Three patients (15%) had a lesion in the oval window region (). Two patients (10%) showed signs of labyrinthitis diagnosed on MRI (). The radiological results were in concordance with the intraoperative findings.
Fig. 1 Two different patients with vertigo and dizziness postoperative to stapes surgery. (A) Coronal CT reformatted and (B) axial CT images showed intravestibular protrusion of the prosthesis superior to 2 mm (arrows).
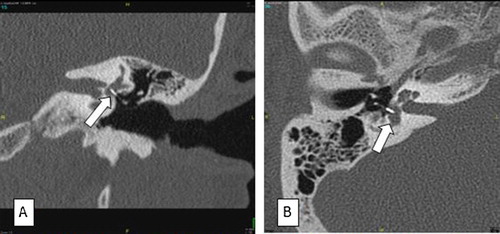
Fig. 2 55 years old male presented with CHF 6 months after stapes surgery. Coronal reformatted CT images showed outward and inferior displacement of the stapes prosthesis seen between the oval window and prosthesis (arrow).
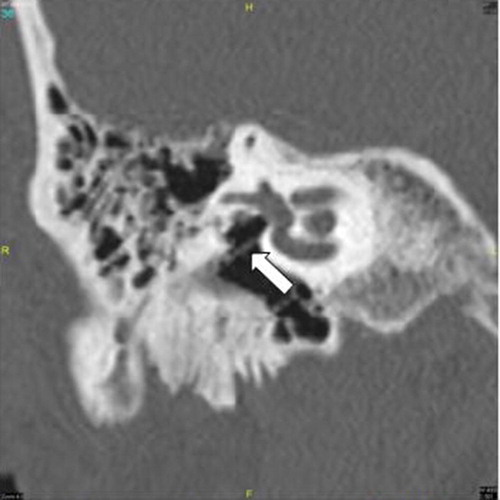
Fig. 3 Postoperative vertigo and sensory neural hearing loss in a 52 year old female patient following stapedectomy. (A) Axial CT and (B) coronal MPR CT reformatted images showed deep intravestibular protrusion of the prosthesis with evidence of pneumolabyrinth (arrows).
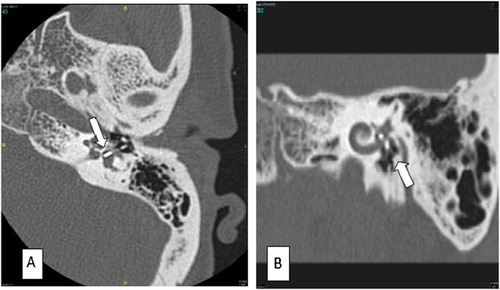
Fig. 4 Dizziness and vertigo in a 35 year-old the female after stapes surgery. (A) Coronal CT reformatted and (B) axial reformatted CT images showed a nonspecific soft tissue mass around the tip of the prosthesis and in the oval window niche suggestive of an intravestibular granuloma (arrows).
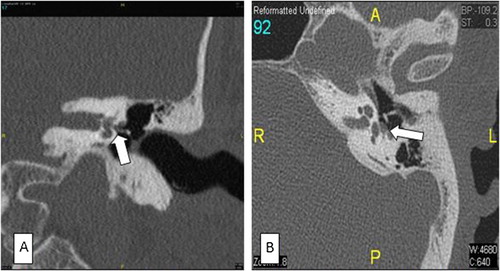
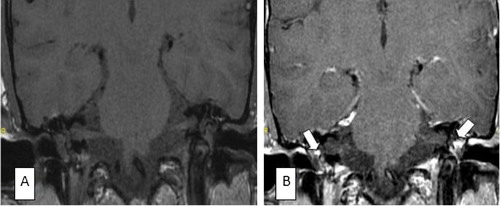
Fig. 5 Patient presented with intermittent tinnitus and vertigo 2 weeks post stapedectomy. (A) coronal reformatted pre-contrast T1 WI and (B) coronal reformatted post contrast T1 WI showed bilateral intense post contrast enhancement in the lesion of both oval window and vestibule on the left side; suggestive of early labyrinthitis (arrows). Incidentally noted bilateral middle ear effusion.
4 Discussion
Otosclerosis is a disease resulting in various foci of bone resorption involving the otic capsule region and is characterized by the presence of demineralization in the active phase followed by sclerosis in remission.Citation11–Citation13 The recommended surgical procedures for otosclerosis are Stapedotomy or stapedotomy.Citation17
Stapedectomy involves the insertion of a stapes prosthesis aiming to restore ossicular chain linkage. A variety of different stapes prosthesis are available, with different materials used as Teflon, stainless steel and platinum; all of which are of variable hyperdensities on CT.Citation15 80% of the causes for surgical revision are due to surgical failure, which is why imaging following the operation is extremely essential in the therapeutic decision. Least encountered complications are the labyrinthine complications reaching to less than 20%. Main complications following surgery are: prosthesis displacement, fibrosis of the oval window, incudo-mallear dislocation, and obliterative otosclerosis.Citation1
Temporal bone CT examination can identify many complications of stapes surgery; especially prosthesis dislocation and graft retraction. Postoperative otitis media and injury of the tympanic membrane are frequently seen with few cases of cholesteatoma formation being reported as a complication following Stapedectomy.Citation15
MR examination, on the other hand, may reveal inner ear complications as an intralabyrinthine hemorrhage, intravestibular extension of a granuloma or inflammatory labyrinthitis.Citation15 Our study showed more prevalent complications among females, which is in agreement with Maria et al.Citation17
Position of the prosthesis; whether intravestibular bulging or outward protrusion has been reported as the most common complication. CT can easily diagnose intravestibular protrusion of the prosthesis- a bulge of the tip of prosthesis more than 2 mm into the vestibule is highly diagnostic.Citation4 In our study, 55% of the cases were due to prosthesis displacement- 30% of them had medial migration of the prosthesis into the vestibule whereas 25% had outward protrusion into the middle ear cavity. Our findings are in agreement with Feldman et al.Citation18 and Han et al.Citation19 The incidence of occurrence of perilymphatic fistula following Stapedectomy is quite rare, ranging from 3 to 10%.Citation20
Air bubbles seen within the vestibule or even a few bubbles seen adjacent to the prosthesis (pneumolabyrinth) is highly suspicious, especially if associated with a fluid-filled middle ear cavity.Citation21 In our study, we encountered only 2 cases out of the 20 (10%) which showed few air bubbles adjacent to the prosthesis particularly the tip on CT. Findings were confirmed on surgery.
Granulation tissue formation may result in recurrent CHL and if visualized at the oval window niche is known as a reparative or postoperative granuloma. Granulation tissue is seen as soft tissue attenuation; however small size, suboptimal technique, and/or motion may limit visualization. Three of our cases showed a small well-defined round lesion within the oval window by CT; one of which showed suspected intravestibular extension as well. One of the severely encountered complications of stapedectomy is suppurative labyrinthitis, as infection could spread intracranially resulting in serious complications as meningitis.Citation22
Two of our cases showed no well-defined cause by CT inspite of persistent SNHL. MRI was thus followed and they were diagnosed as early labyrinthitis by the presence of enhancement of the membranous labyrinth on the postcontrast sequence. Labyrinthitis may be suggested late in the course of the disease if CT shows increased density within the labyrinth, irregularity or obliteration of the labyrinth.Citation22 There were no suspected cases of postoperative cholestaetomas in our study.
Fortunately, complications of stapedectomy are not commonly seen, reaching up to only 1%.Citation10
CT is the most important imaging modality to be done following operation as most of the complications are diagnosed by CT. The thin cuts taken allows accurate and clear identification of all the middle ear complications encountered postoperatively as prosthesis location and presence or absence of a reparative granuloma. Even progression of the otosclerosis can be diagnosed by CT alone.
On the other hand, MRI is rarely performed and used for only those cases where labyrinthine complications are suspected and which usually occur secondary to intravestibular migration of the prosthesis, labyrinthitis or intravestibular hemorrhage. Another complication diagnosed by CT but which can be confirmed by MRI is the presence of a perilymphatic fistula.
SNHL may appear immediately following surgery or over years later; with vertigo being the main complaint in patients with profound SNHL. Revision Stapedectomy is required in these cases.Citation20 In those patient’s with deteriorated cochlear function following stapes surgery, many studies stressed the need for emergency surgical revision to avoid permanent deafness.Citation20
In our study, CT and in few of the cases MRI, were of great help to the surgeons and helped determine the cause of failure of the stapedectomy procedure; allowing further management and intervention. We had some limitations in our study, which included the limited number of the study population and lack of long-term follow up after diagnosis and surgical revision.
5 Conclusion
Complications following stapedectomy are uncommon, but require urgent management in some cases. CT is the primary imaging modality for evaluating those patients with clinical complaints poststapedectomy and who may require revision surgery. MRI may be further on needed if CT was inconclusive.
Conflict of interest
The authors declared that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 10 August 2017
References
- O.NaggaraT.WilliamsD.AyacheImaging of postoperative failures and complications in stapes surgery for otosclerosisJ Radiol86200517491761
- BelaPurohitRobertHermansKatya Opde beeckImaging in otosclerosis: a pictorial reviewInsights Imaging52014245252
- G.E.ValvassoriImaging of otosclerosisOtolaryngol Clin North Am261993359371
- J.D.SchwartzS.K.MukherjiThe Inner Ear and Otodystrophies. Imaging of the Temporal Bone2009New YorkThieme298411
- T.HutchinsOtosclerosis, Diagnostic Imaging Head and Neck2nd ed.2011AmirsysManitoba
- T.C.LeeR.I.AvivJ.M.ChenCT Grading of otosclerosisAJNR Am J Neuroradiol30200914351439
- I.C.NaumannB.PorcelliniU.FischOtosclerosis: incidence of positive findings on high resolution computed tomography and their correlation to audiological test dataAnn Otol Rhinol Laryngol1142005709716
- D.PicuthS.BrandtA.BerghausVertigo after stapes surgery: the role of high resolution CTBr J Radiol73200010211023
- S.KoslingF.BootzCT and MR imaging after middle ear surgeryEur J Radiol402001113118
- J.P.ThomasA.MinoviS.DazertCurrent aspects of etiology, diagnosis and therapy of otosclerosisOtolaryngol Pol652011162170
- A.Paz CordovésE.Leyva MonteroA.M.García de HombreG.M.Prieto ZelayaEar surgery outcomes in patients operated on for otosclerosisActa Otorrinolaringol Esp5820077982
- V.V.RautJ.G.TonerA.G.KerrM.StevensonManagement of otosclerosis in the UKClin Otolaryngol272002113119
- Anne-SophieRangheardaKathlynMarsot-DupuchaAlexander S.MarkaPostoperative complications in otospongiosis: usefulness of MR imagingAJNR22200111711178
- Maria TeresaBernardoJoanaDiasDanielaRibeiroLong term outcome of otosclerosis surgeryOtorhinolaryngology782012115119
- B.A.FeldmanH.F.SchuknechtExperiences with revision stapedectomy proceduresLaryngoscope80197012811291
- WW.HanA.IncesuluMJ.MckennaRevision stapedectomy intraoperative findings results and review of the literatureLaryngoscope107199711851192
- F.MokhtarinejadN.A.RoozbahanyM.AjamiBilateral hearing loss following unilateral stapes surgeryJ Hearing Sci Otolaryngol120152528
- R.J.WietS.A.HarveyG.P.BauerComplications in stapes surgery: options for prevention and managementOtolaryngol Clin North Am261993471490
- G.J.MatzH.B.LockhartJ.R.LindsayMeningitis following stapedectomyLaryngoscope7819685663
