Abstract
Background
Salt is directly related to hypertension and cardiovascular disease associated with it. As obesity facilitates the effect of salt, a quantification of obese salt intake is necessary.
Methods
Our patients numbering 56 have been recruited in the consultation of the obesity unit. Patients were given a questionnaire about their knowledge concerning salt. Natriuresis of 24 h was quantified. The average amount of sodium consumed per day from foods was determined (SAL), the average amount of sodium consumed per day from table salt added to cooking and seasoning (SAC) and the average total amount of sodium consumed per day (STOQ).
Results
The mean age of our patients was 44.31 ± 12.8 years. The average BMI of our patients was 37.12 ± 5.9 kg/m2. The average systolic blood pressure was 123.8 ± 14 mmHg and mean diastolic blood pressure was 76.45 ± 10.7 mmHg. The average amount of sodium consumed per day from food (SAL) was 1915 ± 1038 mg. The average amount of sodium consumed per day from cooking salt (SAC) was 2487 ± 1663 mg. The total amount of sodium consumed per day (STOQ) was 4402 ± 1831 mg. This addition is equivalent to 11 ± 4.6 g of salt per day. The total sodium intake exceeded 2000 mg/day in 89.2% of patients. More than half (57%) of spontaneous sodium intake comes from salt added. The average natriuresis in our population is 158 ± 68 mmol/24 h, higher than the norm in 18% of cases.
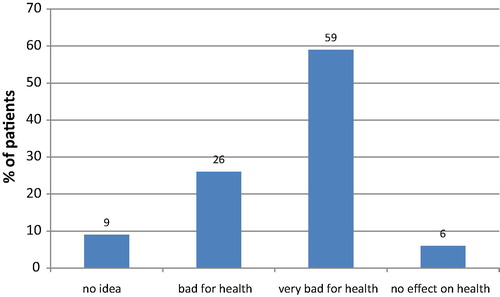
The majority (85%) of our patients have claimed that excess salt is bad to very bad for health.
Conclusion
Our study showed the importance of salt consumption in obeses and especially table salt and yet the majority of our patients consider it to be harmful to health.
It will be necessary to take into account the sodium intake when prescribing the diet.
Keywords:
1 Introduction
Diseases related to salt consumption constitute at present a public health problem. According to WHO,Citation1 more than one in three adults worldwide suffer from hypertension. Regardless of its effect on blood pressure, salt consumption has a direct effect on stroke and progression of kidney disease. Finally, it is probably a major cause of stomach cancer.Citation2 Overweight and obesity are more salt sensitive.Citation4 Some studies have suggested that the presence of obesity may enhance the effect of salt on blood pressure,Citation5,Citation6 the objectives of this study are to quantify the spontaneous intake of table salt of an obese group and evaluate therefore their spontaneous daily intake of sodium.
2 Methods
This descriptive cross-sectional study involved 56 obeses (Body mass index BMI ≥ 30 kg/m2) (9 male and 47 female) aged 14 years old and more. The 56 obeses were Randomly recruited from the outpatient clinic. The study was conducted in the research unit on human obesity at the National Institute of Nutrition and Food Technology in Tunisia. Patients were interviewed and examined by nutritionists doctors. Food surveys and the calculation of salt intake were carried out by a qualified and trained dietician. Hypertensive and patients with heart or kidney failure were not included in our study even patients with thyroid dysfunction and pregnant and lactating women. Because these patients are already under diet which can influence their spontaneous salt intake. Each of these obese patient underwent a thorough examination, a questionnaire about their knowledge concerning salt, anthropometry, determination of body composition with a TANITA type of impedance meter, a natriuresis of 24 h (1 g NaCl consumed per day = 17 mmol Na urinary excreted through 24 h) and a dietary survey. The average amount of sodium consumed per day from foods was determined (SAL). This amount (SAL) is achieved by Bilnut software. To determine the contribution of food in the salt intake of the population studied, a manual calculation was made according to the following example:
100 g olive = 2250 mg sodium; 5 g (an olive) = 112.5 mg sodium.
If an individual consumes 2 olives per day, then 225 mg of the total sodium intake comes from olive.
It was also determined the average amount of sodium consumed per day from table salt added to cooking and seasoning (SAC), to do this, we proceeded as follows: A pack of 1 kg of iodized table salt dried (The Flamingo) was distributed for every patient. Asked to only use this packet of salt for its cooking and seasoning for 7 days. It records on a weekly diary the number of people having lunch and/or dined the food prepared by the salt of the study and the amount of rest discarded.
The day of the appointment (day 7), the patient returns the completed table and remaining salt to be weighed by scales Kenwood type of electronic food. The difference ΔP = weight of sealed packet – weight rendering package (day 7) represents the total amount of salt used during the 6 days. To evaluate the contributions in added salt, ΔP was divided by the number of meals actually consumed during the 6 days and then multiplied by 2 (lunch, dinner).
The total average amount of sodium consumed per day (STOQ) was obtained by the following addition: STOQ = SAL + SAC. The result is in milligrams per day. To convert the amounts of sodium (Na) mg/d in salt (NaCl) in g/d is multiplied by a 2.54 and divided by 1000.
For statistical analysis of our results, we used the “SPSS 15” software.
3 Results
The mean age of our patients was 44.31 ± 12.8 years with extremes of 14 and 68 years. Only three patients wereunder the age of 18 years. The average BMI of our patients was 37.12 ± 5.9 kg/m2. The average percentage of body fat in men was 42.8 ± 9.61% and the average percentage of body fat in women is 44.57 ± 4.6%. In our study, the average systolic blood pressure was 123.8 ± 14 mmHg and mean diastolic blood pressure was 76.45 ± 10.7 mmHg .
Table 1 Characteristics of the population.
The average amount of sodium consumed per day from food (SAL) was 1915 ± 1038 mg with a range of 321 mg and 6737 mg.
The average amount of sodium consumed per day from table salt (SAC) was 2487 ± 1663 mg with extremes of 348 mg and 8320 mg.
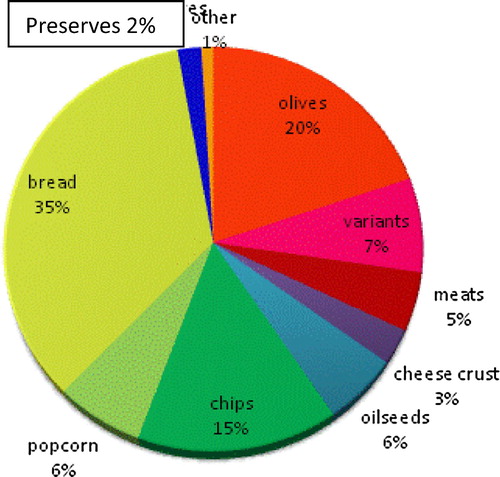
The total amount of sodium consumed per day (STOQ) was 4402 ± 1831 mg with a range of 1071 mg and 9606 mg. This addition is equivalent to 11 ± 4.6 g of salt per day. The total sodium intake exceeded 2000 mg/day in 89.2% of patients. More than half (57%) of spontaneous sodium intake comes from salt added ().
Fig. 1 Contribution of commonly consumed food in spontaneous sodium intake in the population studied.
The average natriuresis in our population was 158 ± 68 mmol/24 h, higher than the norm in 18% of cases. Indirect estimation of spontaneous salt intake of our obese through natriuresis 24 h showed intakes of 9.4 ± 4 g/d.
The majority (85%) of our patients have claimed that excess salt is bad to very bad for health ().
As for the level of perception of salinity in our patients, over half (58.9%) consider their diet is normaly salt versus 8.9% who considered it too salty.
4 Discussion
An adequate intake of salt is essential for proper physiological functioning of the body. At the level of the neuromuscular system, the transmission of nerve impulses and muscle contractions are directly related to the concentration of sodium in the body. It also plays a role in the transfer of sugars and other nutrients necessary for the cell. Salt is also a vector of iodine, an element necessary for brain development and thyroid gland to secrete thyroid hormone. Salt also has a bactericidal action. Sodium chloride is the principal source of sodium, but not the only one, there are in fact other than foods naturally contain such as meat, milk, fresh dairy products, eggs, some fruits and vegetables…
ANSES (French Agency for Food, Environmental and Occupational Health and Safety) considers that the sodium requirement is 400–800 mg of sodium per day to ensure homeostasis.Citation7 For ANSES, the average physiological needs of human adult sodium chloride should not exceed 4 g per day (The French Agency for Food Safety opinion in the report “salt” 2002).Citation8
Globally, the WHOCitation9 established in January 2013 a daily target of 5 g or less of salt (<2000 mg of sodium per day) given the relatively high daily intake worldwide.
This situation is comparable to that of Brazil which has an average daily consumption of sodium 4500 mg, according to a survey conducted in 2003 and published in 2009 by Sarno et al.Citation10
However, the most important results have been reported in Turkey, where the analysis of urine samples (natriuresis) in 2008 showed an average daily intake of 7200 mg/day of sodium.Citation11
This over-consumption is also observed but with lesser amounts in France, Canada, Spain, Finland and the United States with daily intake of 3120 mg sodium means, 3400 mg, 2142 mg, 3300 mg and 3435 mg, respectively. summarizes the results of other similar studies to ours:
Table 2 Comparative table of results of French Studies.
Our study shows that the majority of sodium in the typical diet of respondents comes from salt added during food preparation and seasoning (57%) unlike Canadian and French populations where there is a predominance of food products processing (77% and 75% respectively).
Analysis of the results of our investigations shows that the bread is the main vector of salt in foods of our obese (35%) (). A similar prevalence was revealed by the NutriNet-health studyCitation12 carried out on the French population in 2010 showed off a contribution of 24.1%.
Study natriuresis 24 h is the Gold standard for estimating that salt intake.Citation13 The amount of sodium excreted in urine represents almost all of the sodium ingested and varies depending on the sodium intake. So the only reliable method to assess the amount of sodium ingested daily is the measurement of urinary sodium excretion over 24 h, natriuresis. It has the advantage of being insensitive to the characteristic subjectivity food intake.Citation14
Our results showed that the average natriuresis in our population was 158 ± 68 mmol/24 h. Indirect estimation of spontaneous salt intake of our obese through natriuresis of 24 divided by 17 shows the contributions of 9.4 ± 4 g/d. These are lower than the results of the dietary survey of our patients (11 ± 4 g/d). This difference is probably explained by other sodium losses in sweat and fecal losses. Moreover, since obese have an increase in tubular reabsorption of sodium in relation hyperinsulinism, it is obvious that their natriuresis 24 h could be reduced.Citation15
However, this method of assessing sodium intake is widely used and recommended for epidemiological investigations mass,Citation16–Citation18 and therefore we recommend its application for the Tunisian population.
Similar results were reported in a Swiss study,Citation19 with 75% of respondents felt that the salt has an impact on health. The majority (81%) considered rightly as hypertension had a direct link with salt consumption. Also among Swiss who consider their salt intake is very low, 80.3% had high natriuresis and thus excessive salt diet.
These results lead us to conclude that our population like many others do not know evaluate the salt content in their diet and therefore the mass nutrition education should be complemented by actions of intervention on reducing salt in processed foods and in particular bread.
5 Conclusions
Education campaigns could significantly improve the knowledge of the main sources of salt ingested by the population. In this regard, it would be useful to develop, in cooperation with industry, a strategy including the labeling of salt content and the reduction thereof foods including bread. The ultimate aim of these measures is to lower blood pressure, reduce the prevalence of high blood pressure and consequently the cardiovascular morbidity and mortality and the prevalence and incidence of other diseases associated with salt consumption.
Conflict of interest
The authors declared that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 16 November 2017
References
- OMS | Questions-réponses l’hypertension artérielle [Internet]. WHO. [cité 16 mai 2016]. Disponible sur: <http://www.who.int/features/qa/82/fr/index.html>.
- F.DelahayeDevons-nous consommer moins de sel?Presse Méd412012644649
- A.UzanP.DelaveauThe salt content of food: a public health problemAnn Pharm Fr Juill672009291294
- T.FujitaMineralocorticoid receptors, salt-sensitive hypertension, and metabolic syndromeHypertension Avr552010813818
- J.ChenD.GuJ.HuangMetabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China a dietary intervention studyLancet Lond Engl3732009829835
- Rocchini AP, Key J, Bondie D, et al. The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N Engl J Med. 1989;321:580–5.
- Agence française de sécurité sanitaire des aliments (Afssa). Apports nutritionnels conseillés pour la population française; 2001.
- Afssa. Rapport sel, évaluation et recommendations; 2002.
- Organisation mondiale de la Santé (OMS). Régime alimentaire, nutrition et prévention des maladies chroniques. Rapport d’un Groupe d’étude de l’OMS. Genève: OMS; 2003.
- F.SarnoR.M.ClaroR.B.LevyD.H.BandoniS.R.G.FerreiraC.A.MonteiroEstimated sodium intake by the Brazilian population, 2002–2003Rev Saúde Pública. Avr432009219225
- F.J.HeK.H.JennerG.A.MacgregorWASH-world action on salt and healthKidney Int782010745753
- Etude Nutrinet-Sante. <http://www.etude-nutrinet-sante.fr>.
- Jallet C. Evaluation De La Consommation De Sel En Pratique Medicale: Validation D’un Auto-Questionnaire [Internet]; 2012 [cité 17 mai 2016]. Disponible sur: <http://aurore.unilim.fr/theses/nxfile/default/ecb99db5-c347-43bc-a99e-c8e7c083d603/blobholder:0/M20123169.pdf>.
- Frey J, Daudon M, Raby N, et al. Valeur séméiologique des paramètres biochimiques urinaires. Ann Biol Clin (Paris). 2001;59:13–25.
- H.P.DustandObesity and hypertensionAnn Intern Med103198510471049
- Cook NR, Obarzanek E, Cutler JA, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009;169:32–40.
- Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279:839–46.
- J.StamlerP.ElliottB.DennisINTERMAP: background, aims, design, methods, and descriptive statistics (nondietary)J Hum Hypertens172003591608
- A.ChappuisM.BochudN.GlatzP.VuistinerF.PaccaudM.BurnierSwiss survey on salt intake: main results2011Bundesamt für GesundheitAbteilung Strahlenschutz, Bern