Abstract
Background
Fibrous dysplasia (FD) and ossifying fibroma (OF) are fibro-osseous lesions (FOLs) having several overlaps that may make final diagnosis difficult by hematoxylin and eosin (H/E) alone.
Aim
This study seeks to detect any association between Azan and Toluidine blue staining as compared with osteocalcin in FD and OF diagnosis.
Methods
Forty formalin fixed paraffin embedded (FFPE) blocks of FD and OF were prepared for Azan, Toluidine blue and osteocalcin staining. Brown staining of calcified structures was considered as positive for osteocalcin. Scoring for Azan and Toluidine blue was evaluated based on intensity and localization. Level of agreement of original and revised diagnosis was determined.
Results
Six (40%) of 15 FD were corroborated by osteocalcin. Eight cases initially diagnosed as OF were revised to FD. There were 25 OF according to H/E, and 17 (68%) were validated by osteocalcin. Measure of agreement between histology and immunohistochemistry was 0.081; p = .608. Eleven (42.3%) OF expressed strong toluidine blue staining of the intervening fibrous connective tissue stroma while only 2 (14.2%) FD showed similar staining, this difference was statistically significant [p = .001].
Conclusions
Histomorphometric analysis with Toluidine blue may reduce diagnostic errors of OF and FD.
1 Background
Fibrous dysplasia (FD) and ossifying fibroma (OF) are fibro-osseous lesions (FOLs). FOLs are diverse jaw disorders characterized by the replacement of normal bone with benign fibrous connective tissue matrix and a secondary attempt at new bone formation.Citation1–Citation3 Although there are some differences in the biologic behavior, clinical presentation and radiography of these two lesions, there are several overlaps that may make final diagnosis difficult.Citation4 The histology of the two lesions, again, is so similar, that it is virtually impossible to make a diagnosis of either one of them based on histology alone. The basis for final diagnosis and clear objectivity is therefore called into question. So, with overlapping clinical presentation and indistinct histology, reliable diagnosis can only be reached by further investigations.
Establishing related genetic disorders in these two conditions have served to separate them. Polymerase Chain Reaction analysis for mutations at Arg-201 codon of the alpha subunit of the trans-membrane stimulatory G protein gene (GNAS-1) has been shown to be a marker for jaw FD.Citation5 Another report found a mutation of the tumor suppressor gene HRPT2 in OF and suggested that OF was due to haploinsufficiency of the HRPT2 gene.Citation6 Immunohistochemical marking for several bone matrix proteins have shown no significant differences between FD and OF except for osteocalcin, which has strong expression in the calcified regions of FD, but is weak in OF lesions.Citation5 Osteocalcin is the most abundant non-collagenous protein distributed in normal bone and is a negative regulator of bone formation. The abundance of osteocalcin in FD contrasted with OF implies that the calcified material in FD is comparable to normal bone than that in OF.Citation7
Distinguishing between FD and OF using either the genetic or immunohistochemical tests in each case of a FOL may not be feasible in all cases for all laboratories due to overhead costs and or patients inability to afford such tests. Also the results of tests may be needed in a relatively short turn-around time and this may not be possible with genetic or immunohistochemical analysis. Thus, we therefore conduct this study to detect any correlation between relatively simple histo-morphometric analysis with Azan and Toluidine blue as compared with immunohistochemistry by osteocalcin. These may offer a relatively less complex and quicker method for appropriate diagnosis. Azan is a trichrome stain that uses three anionic dyes to mark different tissues histologically. It is an improvement over the traditional Mallory’s method and stains muscle fibers red and cartilage/bone matrix blue.Citation8 Toluidine blue is an acidophilic metachromatic dye that selectively stains acidic tissue components (sulfates, carboxylates, and phosphate radicals). It has been extensively used as a vital stain for mucosal lesions but has also found applications in tissue sections to specifically stain certain components owing to its metachromatic property.Citation9
OF and FD are the FOLs mostly associated with significant cosmetic and functional disturbances. As the treatment and prognosis differs for both, it is important to distinguish between these two lesions.Citation10
2 Methodology
Forty formalin fixed paraffin embedded (FFPE) blocks of FD and OF cases from the Oral Pathology Department of the University College Hospital, University of Ibadan Nigeria were sectioned and stained with hematoxylin and eosin for re-evaluation and inclusion. At the Frankfurt Orofacial Regenerative Medicine (FORM) Lab, Department for Oral, Cranio-Maxillofacial and Facial Plastic Surgery, Medical Center of Goethe University Frankfurt, Frankfurt am Main, Germany, sections were prepared for Azan, Toluidine blue staining and immunohistochemistry to osteocalcin from each FFPE block.
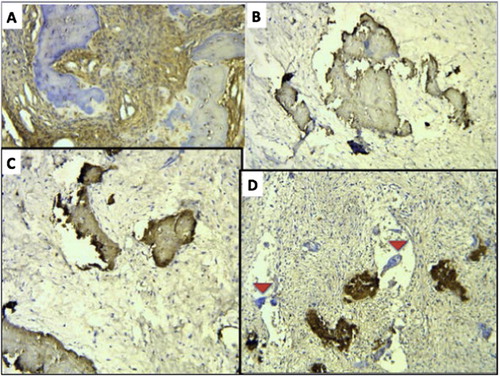
2.1 For osteocalcin
The sections were de-paraffinized using xylene and hydrated with descending grades of alcohol. Each tissue was immersed in heat-induced epitope retrieval 10mMol citrate buffer pH 6.0 (TA-250-PM1X), diluted 1:100 with distilled water and incubated at 95 °C for 20 min. They were cooled in the buffer for 20 min and then rinsed in PBS for 5 min. Positive and negative controls were employed. Thermo-Scientific peroxidase blocking reagent was added to each section for 15 min, and the sections were rinsed in 0.1% TBST for 5 min. The specimen were incubated for 60 min with 1:200 dilutions of Abcam Mouse monoclonal Anti-Osteocalcin antibody [OC4-30] (ab13418) and then rinsed with TBST, followed by incubation with pre-diluted (ready-to-use) Ultra-Vision Quanto Detection System/Horse Radish Peroxidase for 15 min. One ml of diaminobenzidine substrate with one drop of diaminobenzidine chromogen was added to cover the slides, followed by incubation in a humidity chamber for 5 min. The sections were then immersed in aqueous Meyer’s haematoxylin and rinsed in distilled water for 5 min. The tissue was dehydrated and subsequently rinsed with xylene. DPX was applied, and a cover slip placed. Brown staining of calcified structures was considered as positive for osteocalcin. Cases with weak staining (0 or +) were categorized as OF while those with strong staining (++ or +++) where categorized as FD.Citation5
2.2 For Azan
Each tissue was passed through xylene and descending grades of ethanol then rinsed in distilled water for 3 min and placed in nuclear fast red solution for 30 min, rinsed twice under running water and once in distilled water. Section differentiation via 0.1% aniline alcohol solution was done for 3 min and stopped by placement in acetic alcohol solution. They were placed in 5% aqueous phosphotungstic acid for 10 min, rinsed in distilled water and placed for 5 min in 1part Aniline Blue-Orange mixture to 3 parts distilled water and briefly rinsed again in distilled water. Absolute alcohol (100% Isopropanol) was then used to dehydrate the sections through 2 changes for 2 min each. Xylene was finally used 3 times for 3 min each to clear the slides and cover slips placed.
2.3 For toluidine blue
The sections were deparaffinized, hydrated to distilled water and stained with toluidine blue solution for 1–2 min. They were then washed in 3 changes of distilled water and dehydrated quickly through 95% and absolute alcohol, cleared in 2 changes of xylene for 3 min and a coverslip was placed with DPX.
Scoring for Azan and Toluidine blue was evaluated based on intensity and localization of stain. Azan stained the bone periphery and core differentially in some cases and only the core bone staining was used, while toluidine blue staining of bone islands and fibrous connective tissue were used in the final analysis. Intensity was relatively categorized as no staining, weak, moderate, or strong. All slides were viewed with a Nikon ECLIPSE 80i microscope (Nikon, Tokyo, Japan) and microphotographs of selected sections were recorded with a connected digital camera DS-Fi1 together with a Nikon digital sight control unit (Nikon, Tokyo, Japan).
Each sample was examined and scored by an oral pathologist. The data were analyzed using version 20 of the SPSS. The level of agreement of original and revised diagnosis was determined using kappa statistics. The level of significance was set at P < .05.
The Helsinki Declaration was followed for this investigation.
3 Results
There were 15 cases of FD according to Hematoxylin and Eosin (H/E) diagnosis, of these only 6 cases (40%) were confirmed to be FD by osteocalcin. Another 8 cases initially diagnosed as OF were revised to FD following moderate to strong osteocalcin staining (). There were 25 cases of OF according to H/E diagnosis, of these, 17 cases (68%) were validated by osteocalcin. Another 9 cases initially diagnosed as FD were revised to OF following negative to weak osteocalcin staining. The measure of agreement between histology diagnosis and immunohistochemical revision following osteocalcin was 0.081; p = .608.
Fig. 1 Osteocalcin staining of trabecular bone: [A] negative [B] weak (+) [C] moderate (++) [D] strong (+++) (inset red arrow pointing out unstained multinucleated giant cells). Osteocalcin score of 0 and + represent OF cases while ++ and +++ represent FD cases. All sections are X40 magnification.
For the 26 cases diagnosed as OF by weak or negative osteocalcin staining, 20 (76.9%) were negative for toluidine blue bone staining, while out of 14 FD cases 9 (64.2%) were negative (). However, 11 (42.3%) cases of OF expressed very strong (+++) toluidine blue staining of the intervening fibrous connective tissue stroma while only 2 (14.2%) cases of FD showed similar staining (), this difference was statistically significant [p = .001] (). Azan stained the core of the calcified bone differentially from the periphery (). For consistency, we used the bone core staining as representative. Weak to strong yellow azan staining of bone core was seen in 4 (15.3%) cases of OF but this was not seen in any FD case ().
Fig. 2 Toluidine blue stain, [A] negative bone staining with FCT staining strong (+++) X40 [B and C] negative bone staining with FCT staining weakly (+) X40 and X100 respectively [D] bone staining and FCT staining are both moderate (++) X100.
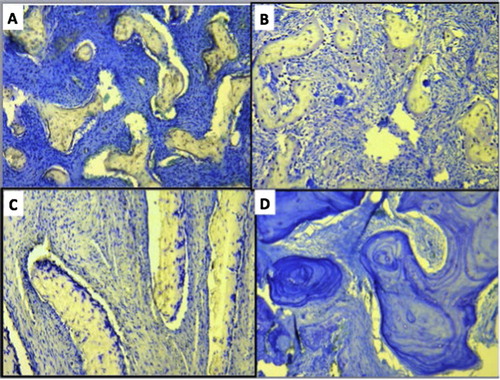
Fig. 3 Azan stain, [A] blue strong (+++) stain [B] yellow moderate (++) stain [C and D] differential bone peripheral and core staining, C was taken as yellow weak (+) and D taken as blue weak (+). All sections are X40 magnification.
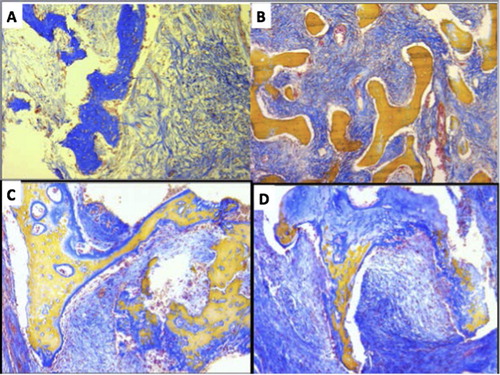
Table 1 Toluidine bone staining intensity compared with osteocalcin bone stain.
Table 2 Toluidine fibrous connective tissue staining intensity compared with osteocalcin bone stain.
Table 3 Azan bone-core staining intensity compared with osteocalcin bone stain.
4 Discussion
The two most confused benign FOLs are FD and OF, and although clinical, histological and radiographic characterization may aid with diagnosis,Citation10 further investigations are still needed for a completely correct final diagnosis. Previously, researchers considered that OF and FD were either the same lesion or variants of the same entity,Citation11 but osteocalcin staining by Toyosawa et al. Citation5 suggested that they were distinct lesions. In Toyosawa’sCitation5 report, both OF and FD showed similar expression for all immunohistochemical markers used including that for Runx2 (which determines osteogenic differentiation from mesenchymal stem cells) but FOLs with moderate to strong expression of osteocalcin showed mutations of the GNAS-1 gene found in FD. While on the other hand the FOLs with weak expression or no expression of osteocalcin, also had no mutations of the GNAS-1 gene, and were categorized as OF.
We thus validated or revised previous H/E diagnosis of FOLs in our study based on the expression of osteocalcin, and from the number of cases that needed re-categorization, it was evident that the diagnosis of OF and FD still poses a significant challenge for clinicians and pathologist using only the clinical features and H/E method for diagnosis. The level of agreement between histology diagnosis and immunohistochemical diagnosis from our analysis was very poor indeed and thus we can categorically state that histology criteria is certainly not sufficient to make accurate diagnosis any longer. However, even though we found that the likelihood of making a correct diagnosis of OF by H/E was higher than that for FD, we still suggest that the use of further ancillary tests be incorporated as minimum standard in the diagnosis of FOLs.
Oxytalan fibres (so called because they are resistant to acid hydrolysis), have been reportedly seen in FOLs and they were found more in OF than FD.Citation12 In our study, Toluidine blue, which is acidophilic, was found to strongly stain 42.3% of OF and 14.2% of FD, this difference was statistically significant. Thus, we suggest that strong Toluidine blue staining of the fibrous connective tissue stroma of FOLs may most likely indicate an OF. A study by Gulati et al.,Citation10 using both trichrome and modified Halmi staining in FOLs, showed more oxytalan fibres in OF by the strong purple coloration observed compared to FD cases. They also suggested that the use of such histomorphometric tests might be a solution to the misdiagnosis of these two FOLs, as well as a pointer to their origin. From our study and that by Gulati et al.,Citation10 we advise that in facilities where genetic analysis or immunohistochemical processing may be challenging, a minimum of metachromatic or trichrome staining as suggested above may be useful to help resolve diagnosis of OF and FD.
Azan as earlier stated is a trichrome stain that uses three anionic dyes to mark different tissues histologically. It is an improvement over the traditional Mallory’s method and stains muscle fibers red and cartilage/bone matrix blue.Citation8 A study on its use in ameloblastoma has demonstrated that it could differentiate the fibrous connective tissue from the stellate reticulum in all the variants of ameloblastoma stained. This is an improvement over the routine H and E staining.Citation13
However, in the present study, the pattern of Azan peripheral and core bone staining was inconsistent for both OF and FD and currently we feel it is not useful to differentiate one lesion from the other. This is a lesson that not all trichrome staining methods may be useful for differentiating these lesions and as such further research is needed to test applicable methods.
5 Conclusion
From our experience and other reports noted, the diagnosis of OF and FD by H/E alone is mostly incorrect and thus should be supported by relatively simple histomorphometric analysis such as Toluidine blue staining in the absence of more advanced techniques like immunohistochemistry and genetic analysis.
Acknowledgements
The authors wish to thank Mrs. Verena Hoffmann and Mr. Babajide Okedere for all the technical assistance provided during the course of this study.
Competing interests
None.
Funding
Authors personal funds.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 13 February 2018
References
- M.E.KouryJ.A.RegeziD.H.PerrottL.B.Kaban“Atypical” fibro-osseous lesions: diagnostic challenges and treatment conceptsInt J Oral Maxillofac Surg241995162169
- S.PrabhuS.SharanyaP.M.NaikFibro-osseous lesions of the oral and maxilla-facial region: retrospective analysis for 20 yearsJ Oral Maxillofac Pathol17120133640
- E.F.McCarthyFibro-osseous lesions of the maxillofacial bonesHead Neck Pathol712013510
- T.ShmulyD.M.AllonM.VeredG.ChaushuB.ShlomiI.KaplanCan differences in vascularity serve as a diagnostic aid in fibro-osseous lesions of the jaw?J Oral Maxillofac Surg756201712011208
- S.ToyosawaM.YukiM.KishinoOssifying fibroma versus fibrous dysplasia of the jaw: molecular and immunological characterizationMod Pathol202007389396
- F.J.PimentaL.F.Gontijo SilveiraG.C.TavaresHRPT2 gene alterations in ossifying fibroma of the jawsOral Oncol4272006735739
- P.DucyC.DesboisB.BoyceIncreased bone formation in osteocalcin-deficient miceNature3821996448452
- Kiernan JA. Histological and Histochemical Methods. Theory and Practice. 4th ed. Bloxham, UK: Scion. ISBN 978-1-904842-42-2.
- J.B.EpsteinC.ScullyJ.SpinelliToluidine blue and Lugol's iodine application in the assessment of oral malignant disease and lesions at risk of malignancyJ Oral Pathol Med211992160163
- A.GulatiN.N.RaoR.A.RadhakrishnanFibrous Dysplasia and Ossifying Fibroma – an advent in their diagnosisJ Clin Exp Dent342011e297e302
- D.J.ComminsN.S.TolleyC.A.MilfordFibrous dysplasia and ossifying fibroma of the paranasal sinusesJ Laryngol Otol1121998964968
- J.E.HamnerH.M.FullmerBethesdaOxytalan fibers in benign fibro-osseous jaw lesionsArch Path8219663539
- A.O.AdisaS.E.UdeaborA.KubeschM.BarbeckS.GhanaatiThe utility of azan trichrome staining in ameloblastomaNiger Postgrad Med J23120164446
