Abstract
Aim of work
To evaluate the efficacy of transvaginal ultrasonography (TVUS), magnetic resonance imaging (MRI) and diffusion weighted imaging (DWI) in presurgical staging of endometrial cancer.
Methodology
This work included 35 female patients. Thirty patients were diagnosed to have endometrial carcinoma.
Results
The sensitivity, specificity, predictive values, accuracy of transvaginal ultrasound in detection of invasion of myometrial cavity were 67.25%, 75.0%, 90.00%, 30.00% and in distant metastasis were 77.78%, 80.95%, 63.64%, 89.47% and %80. These variables for MRI were 88.89%, 100.0%, 100%, 66.67% and 91% in myometrial invasion and in distant metastasis were 100.0%, 100.0%, 100.0%, 100% and 100.0%. There was an inversely proportional relationship between ADC values and the tumor grading. Apparent diffusion coefficient (ADC) magnitude of 0.77 ± 0.21 × 10−3 mm2/s was associated with endometrial cancer while normal endometrial cavity showed ADC value of 1.31 ± 0.11 × 10−3 mm2/s).
Conclusion
Conventional MRI, diffusion weighted imaging and contrast enhanced MR images are superior to TVUS in patients with endometrial cancer and ADC values help to differentiate between normal and endometrial cancer which may replace MR contrast enhanced images.
1 Introduction
Carcinoma involving the epithelial lining of the uterine corpus is the most frequent malignant lesion of the female reproductive organ.Citation1
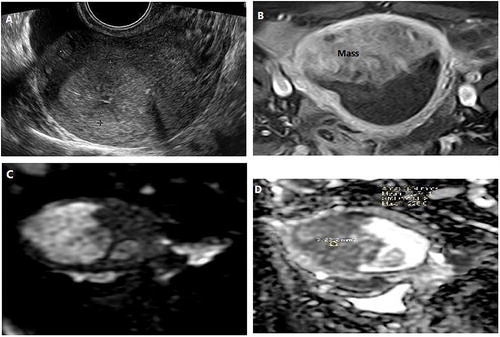
Fig. 2 Well differentiated carcinoma in 55-year-old woman presenting with intermittent postmenopausal bleeding. (A) TVUS image showed thickening of the endometrium reaching 20 mm in its maximum thickness more noted within the uterine fundus with heterogeneous echogenicity (B) Coronal axial T1WI with contrast showed large enhanced heterogeneous mass within the fundal region. (C) DWI & (D) ADC map showed the endometrial mass with restricted Diffusion.
Early diagnosis and proper preoperative evaluation of myometrial invasion are necessary to improve the prognosis. Invasion of inner lining of the uterus (myometrium) and extension of malignancy to the cervical canal cannot be estimated by clinical examination. The line of treatment and the progressive course of endometrial carcinoma depend on deep myometrial and lymphatic infiltration, so accurate detection of infiltration of the deep myometrial cavity is needed to prevent unwanted lymphadenectomy or unnecessary surgical procedures.Citation2
New imaging guidelines for grading and follow of endometrial cancer (EC) were provided as follows: 1- Detection of deep infiltration of myometrial cavity is most important predictive element 2- Detection of cervical canal infiltration which may change the decision of surgical technique 3- identification of suspicious lymph node 4- detection of advanced disease.Citation3
Ultrasonography, especially with transvaginal approach still the best and first imaging technique in female patients with suspicion of endometrial carcinoma.Citation4 Transvaginal ultrasonography (TVU) is widely available in many regions of the world, it is relatively inexpensive, noninvasive and doesn't use ionizing radiation. It has high diagnostic value in detection of myometrial infiltration and cervical invasion.Citation5
Color Doppler ultrasonography shows good predictive value in diagnosis of endometrial carcinoma especially in female patients with post-menopausal bleeding. Good correlations were observed between ultrasound images and pathological type of endometrial cancer, which could provide more evidence-basis for clinical treatment.Citation6
Magnetic resonance imaging (MRI) nowadays is considered the most appropriate technique in grading of endometrial carcinoma, detection of recurrence and response to therapy. MRI has the capacity to study the anatomical structure of the uterus and the surrounding pelvic organs.Citation7
Various pelvic MR imaging sequences used in evaluation of patients with uterine carcinoma including T1- and T2-weighted images, diffusion-weighted imaging, dynamic contrast enhanced images.Citation8
Preoperative MRI may be useful in assessing the severity of endometrial carcinoma, replacing surgical staging and recognizing patients with suspected nodal metastasis. The 2009 International Federation of Gynecology and Obstetrics (FIGO staging system) uses no or <50% myometrium invasion to separate stages IA and IB while stage II is defined by cervical stromal invasion. Therefore, the use of the 2009 FIGO classification rather than the 1998 classification increases the accuracy of an MRI for staging patients because there are fewer staging categories.Citation9
As regards the American College of Radiology (ACR report), contrast enhanced MRI and diffusion images are the preferred modalities for tumor grading and therapy strategy, trans abdominal and trans vaginal ultrasound remain important but they still complementary modality.Citation3
The aim of this work was to assess the diagnostic accuracy of transvaginal ultrasound, Magnetic resonance imaging and diffusion weighted image in female patients with endometrial carcinoma.
2 Patients & methods
2.1 Patients
Thirty-five patients with peri-menpausal vaginal bleeding and suspected endometrial carcinoma by trans-vaginal ultrasound were included in this retrospective study.
Exclusion criteria:
| • | Patients with previous pelvic radiation therapy or any gynecological tumors. | ||||
| • | Patients with MRI related contraindications (claustrophobia or metallic implants). | ||||
| • | Patients with renal impairment excluded from contrast agent administration. | ||||
The medical ethics was considered; the patient was aware of the examination, patient approval was obtained, the economic status of the patient was considered and the patient got benefit from the examination.
2.2 Methods
2.2.1 Ultrasound examination
The equipment we used was ultrasound machine with curved tranabdominal probe. A frequency from 2 to 5 Mhz and transvaginal probe from 5 to 7.5 Mhz probe with colour and power Doppler unit was used. The patient with empty bladder was examined by trans-vaginal ultrasound probe in lithotomy position. The uterus was examined in a longitudinal median section to see the endometrial cavity as a hyperechogenic stripe surrounded by myometrium of less echogencity. Then the probe was tilted from the lateral uterine border to the other contralateral border.Citation10
The uterus was examined in two planes, sagittal plane to examine the uterus from one cornu to the other and in transverse oblique plane starting from the cervix to the uterine fundus by rotating the probe by 90°. This plane helped in evaluation of the whole uterus. The thickness of endometrial cavity was measured mandatory in all patients at its thickest point in the sagittal plane of the uterus. The largest endometrial thickness was about 40 mm and the largest diameter was 21 mm with mean diameter 30 mm. In each patient we assessed size, echogencity of endometrial mass. Endometrial /myometrial interface (regular or irregular) and other uterine or endometrial lesions (fibroids, polyp) were assessed.Citation11 The echogenicity of the mass was analyzed by (2D) ultrasound examination and was defined as hyperechoic, isoechoic or hypoechoic in comparison with the echogenicity of the normal surrounding myometrial tissue. When different echogenic patterns were observed, the tumor echogenicity was classified as heterogeneous. Most of the patients showed hyperechoic mass while less patients showed heterogeneous pattern. Tumor vascularization was subjectively classified using a ‘color score’ into absent, minimal, moderate or high. Vascular morphology was assessed using saved 2D images using both color and spectral Doppler. Five out of 35 patients showed benign lesions.
2.2.2 Magnetic resonance imaging of the pelvis
Pelvic MRI, Diffusion weighted and contrast enhanced images were obtained for 30 female patients included in this study.
Technique of examination
All patients were examined by a 1.5 Tesla MRI (Philips scanner with a pelvic phased-array coil. MRI study included: axial T1, T2 weighted images, sagittal T2 weighted (TSE) images. The patient was asked to void approximately 1 h before the examination to ensure that the bladder is only partially filled since a full bladder may degrade T2-weighted MR images. Contrast enhanced images were performed in axial oblique scan Post contrast fat saturated images were obtained. Diffusion Weighted images were obtained and B-values measured: 0–1000 s/mm2 were used. Apparent diffusion coefficient (ADC) was measured in different areas then we took the lowest mean value. The region of interest (ROI) was put in the site of the lesion. In suspected patients of distant metastasis we obtained additional images of the abdomen.
2.3 References standard
Histopathological confirmation was our reference standard Mucinous adenocarcinoma and endometrioid tumors were divided into three grades (Grade 1: when the tumor is well differentiated, Grade 2: when the tumor showed moderate differentiation and Grade 3 in poorly differentiated tumor) Carcinosarcoma, clear cell cancer and serous or seropapillary cancer are considered Grade 3. Other histotypes and cancer with myometrial invasion >50% or cervical stroma invasion classified as grade 3.Citation12 The final diagnosis of distant metastasis and recurrence made after the histoplathological examination, clinical follow up and radiological imaging.
2.4 Statistical analysis
All statistical calculations and analysis of the present study were conducted by using computer programs Microsoft Excel 2007 (Microsoft Corporation NY, USA) and SPSS version 15 (Statistical Package For Social Science, SPSS Inc., Chicago, IL, USA) for Microsoft Windows, the data about age and Apparent Diffusion Coefficient (ADC) were expressed as mean and Standard Deviation (SD). We calculated: sensitivity, specificity, positive and negative predictive values and accuracy for transvaginal ultrasound and MRI in detection myometrial invasion and distant metastasis. A p value 0.0001 was statistically significant.
3 Results
This study included 35 female patients complaining of abnormal vaginal bleeding with thickened endometrium and suspected to have endometrial cancer (we excluded 5 patients with benign lesions; 3 patients showed endometrial hyperplasia and 2 patients showed endometrial polyps which required only follow up).
Ages of the patients ranged from 38 to 72 years (mean age 57.27) with median age 60 years old, 23.3% of patients aged less than 50 showed evidence of endometria carcinoma ().
Table 1 Prevalence of ages of the studied cases (n = 30).
The degree of myometrial infiltration was classified as either no invasion, <50% invasion (superficial invasion) and >50% invasion (deep invasion). Both ultrasound & MRI showed no invasion in 26.7% of patients. Ultrasound showed superficial invasion in 33.33% of patients while MRI showed superficial invasion only in 20.0%. MRI was superior to ultrasound in detection of deep invasion (53.3% versus 40%) for ultrasound. The histopathological examination of the studied patients showed that only (13.3%) had no evidence of myometrial invasion, (26.7%) showed evidence superficial myometrial invasion and (60.0%) showed deep myometrial infiltration ().
Table 2 US and MRI detection of the depth and degree of invasion of myometrial cavity in 30 patients.
Ultrasound showed sensitivity of 66.25%, specificity of 75.0%, positive predictive value of 90.00%, negative predictive value of 30.00% and accuracy of 68.0% in diagnosing myometrial invasion. MRI showed sensitivity of 88.89%, specificity of 100.0%, positive predictive value 100% and negative predictive value 66.67%. Thus MRI accuracy in detecting invasion of myometrial cavity in patients with endometrial cancer was about 90.9% ().
Table 3 Diagnostic accuracy of transvaginal ultrasound versus magnetic resonance imaging in detecting myometrial invasion in 30 patients with endometrial carcinoma.
In the studied patients, there were 21 patients without distant metastasis, 6 patients with omental deposits and 3 patients with adnexal masses. Ultrasound showed no distant metastasis in 19 patients, omental deposits in 4 patients and adnexal mass in 7 patients. Ultrasound showed sensitivity, specificity, PPV and NPV of 77.78%, 80.95%, 63.64% and 89.47% and %80 respectively. MRI showed no distant metastasis in 21 patients and 6 patients with omental deposits and 3 patients with adnxial deposits. MRI showed sensitivity, specificity, PPV and NPV of 100.0%, 100.0%, 100.0%, 100% and 100.0% respectively (…).
Table 4 US and MRI in assessment of distant metastasis in studied cases (n = 30).
Table 5 Performance of US and MRI in predicting distant metastasis in endometrial cancer.
The mean ADC value of normal endometrium and in endometrial carcinoma listed in . We found that ADC values decreased with increasing tumor aggressiveness. It was found that ADC values of normal endometrium ranges from 1.22 × 10–10−3 mm2/S to 1.52 × 10−3 mm2/S. It measured from 0.57, 0.30 × 10−3 mm2/S to 0.77, 0.31 × 10−3 mm2/S in patients with endometrial carcinoma. (P = 0.0001) ().
Table 6 ADC value in normal endometrial cavity and in patients with endometrial carcinoma.
In the endometrial cancer group, the mean ADC value for each histologic grade was 0.79 ± 0.08 10–3 mm2/S (G1), 0.76 ± 0.14 10–3 mm2/S (G2) and 0.75 ± 0.12 10–3 mm2/S (G3), respectively. No significant correlation between ADC values and tumor grade (P = 0.67).
– demonstrate samples of selected cases of our study; each figure represents one case.
Fig. 1 Myometrial infiltration by well differentiated carcinoma of the endometrial cavity in a female patient aged 67 years presenting with intermittent postmenopausal bleeding. (A) Color Doppler TVUS showed inhomogeneous isoechoic mass with moderate diffuse internal vascularity. (B) Sagittal contrast enhanced T1WI showed enhancing endometrial mass with myometrial invasion (blue arrow) Red arrow represented the normal endometrial cavity above the mass (C) & (D) Coronal DWI showed endometrial mass with restricted diffusion in ADC map.
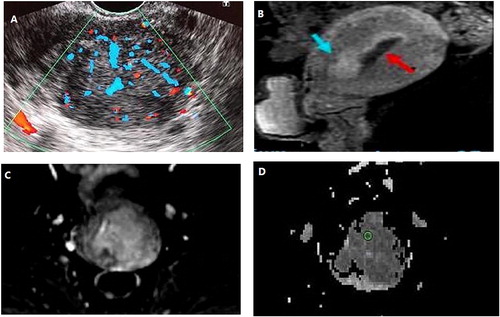
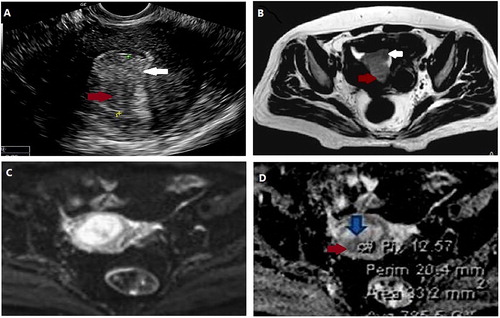
Fig. 3 Concurrent well differentiated endometrial carcinoma with myometrial invasion and a polyp in 46-year-old woman presenting with disturbed menstruation. (A) TVUS image showed thickened heterogeneous endometrium measuring 21 mm in its maximum thickness. The mass was hypoechogenic to the myometrium (red arrow) extending beyond the endometrial/myometrial interface. A polyp (white arrow) is hyperechogenic to myometrium confined to the endometrial cavity. (B) Axial T2WI both the mass (red arrow) and the polyp (white arrow) are hyperintense to the myometrial cavity. (C) Axial DWI shows both lesions hyperintense. (f) ADC map the mass is hypointense (red arrow) with restricted diffusion while the polyp still hyperintense (blue arrow) with no restricted diffusion.
4 Discussion
Cancer of endometrial cavity (uterine carcinoma) is considered the most prevalent cancer of the female reproductive system. Many factors affect the prediction and management of uterine carcinoma including behavior of carcinoma, the degree of infiltration of myometrium and presence of lymphatic or hematogenous dissemination.Citation13
This study was done to detect the diagnostic performance of transvaginal ultrasonography and MRI with diffusion weighted image in evaluation of patients with endometrial carcinoma.
Thirty-Five female patients were included in this research. Thirty patients showed endometrial cancer while the remaining 5 patients were benign conditions. Three patients showed endometrial hyperplasia and 2 patients showed endometrial polyps which required only follow up.
The youngest patient in the current study was 38 years old and the oldest was 72 years old. The mean age of female patients included in this study was 60 years (50–70 years) which matched with Sala et al.Citation14 results which reported that the peak incidence of endometrial cancer was between ages 55 and 65. SalaCitation14 explained the cause of increased the rate of endometrial carcinoma in postmenopausal women, the changes occurs in reproductive behavior as infertility and obesity. Another cause may be hormonal replacement therapy uses in many countries. He stated that use of oral contraceptive pills may be helpful to decrease the rate of this cancer in women aged below 55 years.
In this study, the invasion of myometrial cavity were classified into 3 groups: 1ST group: no evidence of myometrial invasion and tumor located only within the endometrial cavity. 2nd group: the tumor involved only half of the myometrial cavity (superficial invasion) and 3rd group: the tumor involved more than one half of the myometrial thickness (deep invasion).
Histo-pathological analysis showed infiltration of myometrial cavity was found in 26 patients (8 superficial and 18 deep invasion). By transvaginal ultrasound: superficial myometrial invasion found in 10 patients. Two patients showed false positive results. Deep invasion found only in 12 patients (6 patients were underestimated).
MRI with contrast showed 6 patients had evidence of superficial myometrial infiltration (2 patients showed false negative results) while 16 patients showed deep myometrial infiltrations (2 patients were underestimated).
The accuracy of TVUS versus MRI in the assessment of the degree of myometrial invasion were 68% and 91% respectively and this agreed with the studies carried out by Antonsen et al.Citation15 and Ørtoft et al.Citation16 which were done to evaluate the concordance between myometrial infiltration detected by TVUS and definitive histology-pathological examination. Preoperative overall diagnostic sensitivity, specificity of TVUS in evaluation of myometrial invasion was 69% and 74% in Antonsen et al.Citation15 study and 73% and 72% in Ørtoft et al.Citation16 study. AntonsenCitation15 in his study which included 318 consecutive women with EC and compared the diagnostic performance of different modalities including transvaginal ultrasound in the preoperative evaluation of patients with (EC) and concluded that transvaginal ultrasound less sensitive than PET/CT and MRI although ultrasound was done by specialist. ØrtoftCitation16 in his study which compared tranvsvaginal ultrasound, MRI and hysterscope in preoperative staging of endometrial carcinoma and found that deep myometrial invasion was better evaluated with increased accuracy by MRI (82%) than TVS (74%). He concluded that if transvaginal ultrasound performed by efficient sonographer it will be economic modality with high accuracy when compared to that of MRI in the preoperative evaluation of endometrial cancer.
Our results regarding the accuracy of TVUS in the assessment the degree of myometrial invasion in patients with endometrial carcinoma were different from Akbayir et al.Citation17 and Aleksandra et al.Citation18 results which included 298 and 62 patients respectively. The sensitivity, specificity, predictive values (positive and negative) and diagnostic accuracy of TVUS in assessment the degree of myometrial infiltration in patients with endometrial carcinoma were 68.4%, 82%, 65.1%, 84.1% and 77.5% for Akbayir et al.Citation17 study and 77.59%, 100.00%, 100.00%, 23.53 and % 79.0% for Aleksandra et al.Citation18 study.
This controversial higher results of Akbayir et al.Citation17 and Aleksandra et al.Citation18 results might be attributed to the different number of patients included in their study and because ultrasonography is highly operator dependent.
Although ultrasound is more available with decreased cost to the patient with no radiation or intravenous contrast, some factors decreased its accuracy like the skill of the operator and the patient. Obesity and overweight affect the image quality, when the endometrial carcinoma presented by large bulky mass causing dilation and myometrial thinning giving false positive results regarding myometrial infiltration also when the endometrial mass infiltrating the myometrial cavity through thin roots, sometimes become difficult be differentiated from the surrounding endometrium causing underestimation.Citation19
MRI of patients with EC showed 2 false results giving wrong impression of intact junctional zone which was proven to be superficial myometrial invasion in histopathology. There were also 2 underestimated patients showed superficial myometrial invasion on MRI were later on proven to be deep invasion. Underestimation was less common with MRI than TVUS and probably due to thin neoplastic roots invading the myometrium, hardly distinguishable from the surrounding endometrium.
MRI showed sensitivity, specificity, PPV, NPV 88.89%, 100.0%, 100.0% and 66.67% respectively with 90.00% accuracy in assessing endometrial invasion in this study. Our results agreed with Beddy et al.Citation20 and Zandrino et al.Citation21 studies. Beddy et al.Citation20 study which included 48 women with endometrial cancer. MRI sensitivity, specificity and accuracy in detection infiltration of myometrial cavity were 84%, 100% and 90%. In Zandrino et al.Citation21 study which was done on 34 female patients diagnosed to have uterine carcinoma, he found that MRI with contrast- enhanced images showed diagnostic performance of 100% for sensitivity and for NPV, 94% for specificity, 75% for PPV and 95% for accuracy in assessment of myometrial invasion.
In our study, there were 21 patients without distant metastasis and 6 patients with omental deposits and 3 patients with adnxial masses. Ultrasound showed no distant metastasis in 19 patients, omental deposits in 4 patients and adnxial mass in 7 patients. Ultrasound showed sensitivity, specificity, PPV and NPV of 77.78%, 80.95%, 63.64% and 89.47% respectively in detection distant metastasis. Our results showed high accuracy of ultrasound in detection of distant pelvic metastasis that agreed with Fisherova et al.Citation22 study which reported that ultrasound shows good performance in detection the extend of endometrial carcinoma to neighbor's pelvic and distant abdominal structures.
Regarding this study, MRI showed no distant metastasis in 21 patients and 6 patients with omental deposits and 3 patients with adnexal deposits. MRI showed sensitivity, specificity, PPV and NPV 100.0%, 100.0%, 100.0% and 100.0% respectively. we found that MRI was more accurate than ultrasound in assessing distant peritoneal metastasis in endometrial cancer patients that agreed with Torkzad et al.Citation23 result which stated that MRI and CT are equal in imaging peritoneal deposits with better results while ultrasound have less accurate results.
It was reported that the addition of diffusion weighted images in patients with endometrial carcinoma has a good significance and improve the chance to detect uterine malignancy in female patients.Citation24
Beddy et al.Citation20 in his study which compared the diagnostic accuracy of diffusion-weighted magnetic resonance imaging with that of dynamic post contrast MR imaging in assessment of myometrial invasion in patients with endometrial cancer. He concluded that diffusion MR imaging is superior and more accurate than post contrast MR imaging in assessing the overall stage of endometrial cancer.
In this study: there was difference between the value ADC of normal looking endometrial cavity and of that involved by endometrial carcinoma.
We found that ADC values decreased with increasing tumor aggressiveness with significant difference (P = 0.0001). It was found that ADC values of normal endometrium ranged from 1.22 × 10–10−3 mm2/S to 1.52 × 10−3 mm2/S. In patients with endometrial carcinoma, it measured from 0.57, 0.30 × 10−3 mm2/S to 0.77, 0.31 × 10−3 mm2/S but there was no significant statically correlation between values of ADC and the grade of carcinoma (P = 0.76). In the endometrial cancer group, the mean ADC value for each histologic grade was 0.79 ± 0.08 10–3 mm2/S (G1), 0.76 ± 0.14 10–3 mm2/S (G2) and 0.75 ± 0.12 10–3 mm2/S (G3), respectively.
Our results agreed with Rechichi et al.Citation24 and Jiang et al.Citation13 studies. In Rechichi et al.Citation24 study, the mean value of ADC in patients with endometrial carcinoma was (0.77 ± 0.12) and in patients with normal looking endometrium and myometrium was (1.52 ± 0.21, p < 0.0001). He found that lower ADC value in patients with EC than in normal endometrium and myometrium. This may be due to enlarged diameter of malignant cell and increased its cellularity than cells in normal tissue and benign conditions which restrict water diffusion within the malignant cell. He advised that MRI may an option in patients in whom transvaginal ultrasound biopsy or curettage is difficult.
Jiang et al.Citation21 in his study which included 52 patients with invasive endometrial carcinoma. The mean ADC value in patients with EC were significantly lower than normal endometrial tissue, he explains that difference due to different microenvironment of malignant cells with hypercellularity, decreased the extracellular space, abnormal contour of the enlarged nucleus which deceased the motion of water molecule within malignant tissue.
From this study, we can conclude the following:
All MR imaging modalities including contrast enhanced images in addition to diffusion weighted images and ADC map were useful in diagnosis and surgical planning in patients with endometrial carcinoma. TVUS is practically was an important modality for measurement of endometrial thickness. It was the first choice for screening of suspicious patients, escipally when performed by good radiologist. TVUS was a practical, inexpensive and easy imaging procedure. MRI was more reliable than TVUS in staging, treatment strategy and it was helpful in detection of distant metastasis. DWI was appropriate tool in detecting patients with EC with significantly lower ADC values than normal endometrial tissue.
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 14 December 2018
References
- W.J.KohB.E.GreerN.R.Abu-RustumUterine neoplasmNatl Compr Cancer Netw Guidelines Oncol2014
- D.DoganN.InanH.T.SariosyPreoperative evaluation of myometrial invasion in endometrial carcinoma: diagnostic performance of 3T MRIAbdom Imaging382013388396
- O’Malley Ryan DigheInvited commentary on american college of radiology appropriateness criteria endometrial carcinomaOff J Radiol Ultrasound Ultrasound Quart3020142931
- Lalwani Neeraj DubinskyACR Appropriateness Criteria® Pretreatment Evaluation and Follow-Up of Endometrial CancerUltrasound Quarterly3020142128
- J.H.LeeM.K.DigheT.J.DubniskyPostmenopausal endometrial bleedingUltrasound Clinics Top Obstet Gynecol Ultrasound72012123132
- S.L.AntonsenL.N.JensonA.LoftMRI, PET/CT and ultrasound in the preoperative staging of endometrial cancerSci Direct J Gynecol Oncol1282013300308
- S.BatoolS.RazaS.ManzurAccuracy of Doppler ultrasound in diagnosis of endometrial carcinomaJ Pakistan Med Assoc6320132831
- Z.H.QinY.YuanL.HuiThe relationship between the contrastive analysis of pathology and sonogram of endometrial carcinoma and the surgical stagingMed J West China420133337
- E.SalaA.G.RockallS.J.FreemanThe added role of MR imaging in treatment stratification of patients with gynecologic malignanciesRSNA Radiol, Pubmed2662013717740
- L.SavelliM.CeddariniM.LudovisiPreoperative local staging of endometrial cancer: transvaginal sonography vs. magnetic resonance imagingUltrasound Obstet Gynecol312008560566
- F.MasciliniA.C.TestaV.c.HolsbekeEvaluating myometrial and cervical invasion in women with endometrial cancer: comparing subjective assessment with objective measurement techniquesUltrasound Obstet Gynecol422013353358
- J.L.BenedetH.BenderH.Jones3rdH.Y.NganS.PecorelliFIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic OncologyInt J Gynaecol Obstet702000209262
- Jiang J, Zhao JL, Qing JF et al. Endometrial carcinoma: diffusion-weighted imaging diagnostic accuracy and correlation with Ki-67 expression 2018; 4: 413.e1– 413.e6.
- E.SalaA.Andrea RockallR.A.Kubik-Huchadvances in magnetic resonance imaging of endometrial cancerEur Radiol J Eur Soc Radiol212011468473
- S.L.AntonsenL.N.JensenA.LoftMRI, PET/CT and ultrasound in the preoperative staging of endometrial cancer–a multicenter prospective comparative studyGynecol Oncol1282013300308
- G.ØrtoftM.DueholmO.MathiesenPreoperative staging of endometrial cancer using TVS, MRI, and hysteroscopyActa Obstet Gynecol Scand922013536545
- O.AkbayirA.CorbaciogluC.NumanogluPreoperative assessment of myometrial and cervical invasion in endometrial carcinoma by transvaginal ultrasoundGynecol Oncol12232011600603
- P.AleksandraS.DraganL.VekoslavUltrasound diagnostics in patients with endometrial carcinomaJ Analyt Oncol120121931
- D.ArkoI.TakacHigh frequency transvaginal ultrasonography in preoperative assessment of myometrial invasion in endometrial cancerJ Ultrasound Med1992000639643
- P.BeddyP.MoyleM.KataokaEvaluation of depth of myometrial invasion and overall staging in endometrial cancer: comparison of diffusion-weighted and dynamic contrast-enhanced MR imagingRadiology26222012530537
- F.ZandrinoE.L.PagliaF.MusanteMagnetic resonance imaging in local staging of endometrial carcinoma: diagnostic performance, pitfalls, and literature reviewTumori962010601608
- D.FischerovaUltrasound scanning of the pelvis and abdomen for staging of gynecological tumors: a reviewUltrasound Obstet Gynecol, Weley Online Library382011246266
- M.R.TorkzadN.CastaA.A.BergmanComparison between MRI and CT in prediction of peritoneal carcinomatosis index (PCI) in patients undergoing cytoreductive surgery in relation to the experience of the radiologistJ Surg Oncol1112015746751
- G.RechichiS.GalimbertiM.SignorelliEndometrial cancer: correlation of apparent diffusion coeffient with tumor grade and depth of myometrial invasion and presence of lymph node metastasesAm J Reotgenreol1972011256262
