Abstract
Objective:
To determine the accuracy of three-dimensional bladder ultrasonography (US, using the BVI 3000, Verathon, WA, USA) for determining the residual urinary volume, compared with the conventional catheterisation method.
Patients and methods:
We conducted a cross-sectional study at day-care unit of a University hospital after obtaining approval from the Ethics Review Committee of the hospital. Thirty-four patients with lower urinary tract symptoms requiring cystometrography were included. The postvoid volume was measured by bladder US, with three readings taken, and then patient was catheterised using a 12-F Nelaton catheter to measure the urinary volume. The mean of the three readings was compared with the catheterisation volume.
Results:
The mean (SD) urinary volumes by US and catheterisation were 261 (186) and 260 (175) mL, respectively, and the correlation (r2) was 0.97. There was no effect of age, gender or body mass index on the accuracy of bladder US, which was accurate even when the urinary volume was ⩽100 mL.
Conclusion:
The bladder US estimate is as accurate as catheterisation for determining the postvoid residual urinary volume. Its accuracy was also comparable when the urinary volume is <100 mL, and there was no significant effect of age, gender and body mass index. This system could replace the more invasive catheterisation, and with excellent accuracy.
Introduction
LUTS in both in men and women are evaluated using an objective assessment, e.g., by using the IPSS for men and the Female LUTS instrument in women [Citation1]. The subsequent systematic diagnostic evaluation includes a physical examination, urine analysis, blood analysis, ultrasonography (US) of the prostate, bladder and kidneys, uroflowmetry, a measurement of postvoid residual urine (PVR) volume by US, and a bladder diary in patients with urinary frequency or nocturia [Citation2]. Uroflowmetry is an important and basic urodynamic investigation, which is used in patients with LUTS [Citation3], but the indications for more invasive assessment are limited, and warranted only in specific situations [Citation4]. A non-invasive estimate of bladder pressure, with an estimate of the free flow rate, gives useful information in the assessment of men with LUTS. Determinations of bladder voiding efficiency [Citation5] or residual fraction [Citation6] using the volume before and after voiding are other non-invasive methods.
The PVR volume can be measured using different methods, and although catheterisation is the standard method it is invasive and can result in morbidity. Other methods include B-mode US and a bladder US system. US is also time-consuming, costly and requires training. Bladder US systems were first introduced in 1994 and the initial models were all two-dimensional because they only measured the width and length and did not assess the depth of the bladder. Currently, a three-dimensional bladder scanner (BVI 3000™, Verathon, WA, USA) was suggested to be more accurate than other systems [Citation7,Citation8]. However, there are no reports comparing the BVI 3000 with the standard method and determining its efficacy at extremes of volume; in the present study we evaluated these points.
Patients and methods
The study was conducted in the urodynamic suite of a University hospital. The patients comprised those undergoing cystometrography (CMG), and included those aged >18 years who had a suspected neurogenic bladder and who were referred for urodynamic studies. We excluded patients with a reduced bladder capacity due to diseases like tuberculosis or interstitial cystitis, with impaired cognitive function, pregnant woman, any with a lower abdominal surgical scar (which could potentially affect the bladder scan), those who could not lie supine, and those with previous bladder augmentation surgery. Patients had a previous US evaluation to exclude diverticulae, and patients with bladder wall deformities, including a thick-walled bladder, were also excluded. As a matter of protocol, patients with significant faecal loading noted during urodynamic catheter insertion or a DRE had the assessment cancelled were also excluded from the study.
The level of significance was set at 0.05, with 80% power, and the minimum sample size, calculated using PASS 12™ software (NCSS, Kaysville, Utah, USA), was 34. We assumed a coefficient of correlation between A and B of 0.97. The normality of the distribution of the data was evaluated and whether outcome frequencies followed a specified distribution (using Pearson’s chi-squared test).
Continuous variables are given as the mean (SD) and the correlation coefficient was calculated for urinary volumes estimated by the two methods. Categorical variables were analysed as a proportion with percentages. A paired t-test was used to compare the volumes, with P < 0.05 considered to indicate a significant difference.
The correlation between bladder US volumes and catheterisation volumes, with adjustment for confounding factors, i.e., age, body mass index (BMI) and gender, was assessed using multiple linear regression analysis.
Patients initially had uroflowmetry, after which they were asked to lie supine and had their bladder scanned using the BVI 3000, using three scans, with the mean of the three taken as the final value. The nurse in the urodynamic suite (not part of the study team) performed the bladder scan. Immediately after scanning the patients were catheterised (by a resident, on rotation through the urodynamic and flexible cystoscopy suite) to determine the PVR volume. A Nelaton catheter (a stiff straight catheter) was used to empty the bladder before starting CMG.
Approval was obtained from the Ethics Review Committee for the study (approval #1721-SUR-ERC-10). Neither the institution nor the investigators had any support, financial, technical or otherwise, from the manufacturer during the conduct of this study.
Results
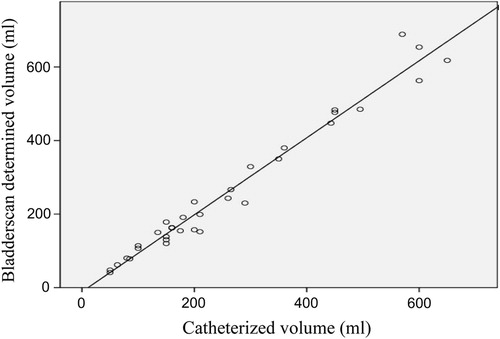
Thirty-four patients were included in the study (19 male) with a mean (SD) age at presentation of 50.2 (20.2) years and a mean (SD, range) BMI of 26.2 (5.9, 17.6–40.3) kg/m2. The respective mean (SD) volumes for the BVI 3000 and catheterisation methods were 261 (186) and 260 (175) mL, and the respective median (range) volumes were 184 (41–869) and 200 (50–680) mL; there was no statistically significant difference between the groups (paired t-test). The correlation coefficient between the methods was 0.97.
There was an excellent correlation () at all volumes, and in particular for volumes of <200 mL. For volumes of >600 mL, there was some divergence but this was not statistically significant and there were few patients in this subgroup. There were seven patients who had smaller bladder volumes, of <100 mL, but they were assessed separately and there was a significant correlation between the two methods. When the patients were sub-stratified into two groups depending on age (<50 and >50 years) or BMI (<25 and >25 kg/m2) there was no difference between the groups in the estimates of bladder volume by the bladder scan.
Discussion
The measurement of PVR volume is an important diagnostic step in evaluating patients with LUTS, and thus the accurate measurement of this volume is important in the diagnostic and management algorithm. Urethral catheterisation has long been considered the standard method for measuring the PVR volume but it is frequently associated with discomfort and carries a risk of UTI and trauma [Citation9]. To avoid an invasive catheterisation, US is being increasingly used for this purpose [Citation10]. US is not only reliable but is also reproducible. However, there are some shortcomings, including cost and the availability of a radiologist and equipment. Currently, the PVR volume can be measured by healthcare personnel (with no specialised training) using a portable, self-calculating US system, e.g. the bladder scanner. Such a portable bladder scanner has several advantages over real-time US, in that it is user-friendly and requires only basic training. It can be used at the bedside, obviating the need to use the resources of the radiology department.
The correlation coefficient between the methods in the present study was 0.97. Park et al. [Citation11] assessed a bladder scanner which had real-time pre-scan imaging (RPI), finding it better than a conventional bladder scanner for measuring the PVR volume. They reported that the ability to point the scanner exactly at the bladder before measuring the bladder volume with RPI seemed to reduce the variability of the measured values.
One of the disadvantages of the conventional bladder scanner, i.e., one with no RPI, is that it does not allow the operator to visualise the bladder directly [Citation11]. This could have serious diagnostic consequences. In patients with neurogenic bladder problems, studies show that portable bladder US systems are an acceptable alternative to catheterisation, although they are not as accurate as catheterisation for estimating bladder volumes [Citation12].
The BVI 3000 system calculates the bladder volume using VMODE® technology; measurements made with this technology are more accurate than those from conventional two-dimensional US, being are based on a more detailed three-dimensional image of the bladder. The technique is easy to use and more comfortable for the patient. When the system is actuated this technology quickly assesses the echoes from several planes in the body and constructs a three-dimensional image, from which the system can calculate the bladder volume, and display several B-mode images.
There are many conditions which can confound the estimate of volume, i.e., cystic ovarian pathologies might be construed as a significant PVR volume [Citation13]. In the present study there was an excellent correlation for all volumes, but there are other conditions that can potentially affect the volume estimate.
Choe et al. [Citation14] reported six patients in whom a follow-up assessment of a high PVR volume measured on US studies gave lower catheterised volumes, with a range of differences of 66–275.5 mL. These patients were later diagnosed with an ovarian cyst, uterine myoma, or uterine adenomyosis on pelvic US.
There are also reports showing poor repeatability and accuracy in bladder volume measurements using the BladderScan (Verathon) when compared with real-time US [Citation15]. These authors reported that the BladderScan method does not appear to be reliable for assessing bladder volumes in children aged 0–24 months before bladder instrumentation. Koomen et al. [Citation16] also found that the BladderScan underestimated the urinary bladder volume in children.
Alnaif and Drutz [Citation17] reported that the bladder was not fully imaged if the scanning heads were aimed incorrectly, and that partial bladder volumes resulted if the lateral borders were omitted, producing measurements that underestimated PVR volumes. These authors concluded that PVR volumes from portable bladder US machines should be interpreted cautiously, and that catheterisation might be the better method if an accurate estimate of PVR volume was needed.
The efficacy of a bladder scanner in morbidly obese patients is lower [Citation18], but we found no difference related to the BMI in the present study. This could possibly be because there were relatively few patients with a BMI of >35 kg/m2. An inaccurate estimate could also be possible in patients with ascites. Elsamra et al. [Citation19] reported on two adolescent females with LUTS who had falsely elevated PVR volumes by bladder scanning, and who subsequently underwent formal imaging to identify ovarian cystic pathology.
The utility of the bladder scan was assessed in various clinical situations. Bozsa et al. [Citation20] assessed its utility for estimating the PVR volume after radical hysterectomy, comparing the US-estimated volume with that from catheterisation. They reported that both non-invasive three-dimensional US methods are appropriate for the correct volume determination of PVR after radical hysterectomy. This obviates the need for catheterisation, with its risks of UTI in patients with an insignificant PVR volume. Beckers et al. [Citation21] reported that the BVI 6200 was not reliable enough to replace conventional US for measurements of bladder volumes. It is not advisable to use it in a bladder-retraining programme. Goode et al. [Citation22], in a series of 95 ambulatory women with urinary incontinence, reported that US had a sensitivity of 66.7% and a specificity of 96.5% in detecting a PVR volume of ⩾100 mL.
Portable US scanners are quick, easy to use, reasonably sensitive, and very specific for determining an elevated PVR. There are no contraindications for the use of the BladderScan, but informed consent must be obtained and healthcare workers trained in the use of the device. The potential adverse effects of portable bladder US include skin irritation, an allergic reaction to the gel and padding, and pressure-sore formation at the site of sensor placement [Citation23]. Huang et al. [Citation24] reported that the volumes estimated by a bladder scan were less accurate than those from catheterisation, particularly for small PVR volumes. The present results indicate that the bladder scan has a good correlation coefficient at all volumes. However, the major limitation of the present study was the few patients included, which made a subgroup analysis difficult. The other limitation was that the patients were a selected group presenting for an invasive urodynamic evaluation. Future work should be in a multi-institutional/multi-centric study with a larger cohort.
In conclusion, the BVI 3000 was as accurate as catheterisation for determining the PVR volume. The accuracy was also comparable when the urinary volume was <100 mL. There was no significant effect of age, gender or BMI on the bladder scan estimate of PVR volume. This system could replace more invasive catheterisation, and with excellent accuracy.
Conflict of interest
None.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- P.AbramsL.CardozoM.FallD.GriffithsP.RosierU.Ulmstenet alThe standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn212002167178
- M.OelkeA.BachmannA.DescazeaudM.EmbertonS.GravasM.C.Michelet alGuidelines Office. Guidelines on EAU Guidelines, Edition presented at the 25th EAU Annual Congress, Milan2013 978-90-79754-70-0
- M.H.AtherA.MemonUroflowmetry and evaluation of voiding disordersTech Urol41998111117
- C.BlakeP.AbramsNoninvasive techniques for the measurement of isovolumetric bladder pressureJ Urol17120041219
- P.AbramsBladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding functionBJU Int8419991415
- A.MemonM.H.AtherUse of residual fraction instead of residual volume in the evaluation of lower urinary tract symptomsTech Urol620002628
- K.R.GhaniJ.PilcherD.RowlandU.PatelD.NassiriK.AnsonPortable ultrasonography and bladder volume accuracy – a comparative study using three-dimensional ultrasonographyUrology7220082428
- G.Al-ShaikhA.LarochelleC.E.CampbellJ.SchachterK.BakerD.PascaliAccuracy of bladder scanning in the assessment of postvoid residual volumeJ Obstet Gynaecol Can62009526532
- A.J.SchaefferJ.ChmielUrethral meatal colonization in the pathogenesis of catheter-associated bacteriuriaJ Urol130198310961099
- N.SimforooshF.DadkhahS.Y.HosseiniM.A.AsgariA.NasseriM.R.SafarinejadAccuracy of residual urine measurement in men: comparison between real-time ultrasonography and catheterizationJ Urol15819975961
- Y.H.ParkJ.H.KuS.J.OhAccuracy of post-void residual urine volume measurement using a portable ultrasound bladder scanner with real-time pre-scan imagingNeurourol Urodyn302011335338
- Health Quality OntarioPortable bladder ultrasound: an evidence-based analysisOnt Health Technol Assess Series62006151
- M.R.CooperbergS.K.ChambersT.J.RutherfordH.E.FosterJr.Cystic pelvic pathology presenting as falsely elevated post-void residual urine measured by portable ultrasound bladder scanning: report of 3 cases and review of the literatureUrology552000590
- J.H.ChoeJ.Y.LeeK.S.LeeAccuracy and precision of a new portable ultrasound scanner, the BME-150A, in residual urine volume measurement: a comparison with the BladderScan BVI 3000Int Urogynecol J Pelvic Floor Dysfunct182007641644
- C.BevanD.BuntsmaA.StockT.GriffithsS.DonathF.E.BablAssessing bladder volumes in young children prior to instrumentation. Accuracy of an automated ultrasound device compared to real-time ultrasoundAcad Emerg Med182011816821
- E.KoomenE.BoumanP.CallewaerdtG.D.VosM.H.PrinsB.J.Andersonet alEvaluation of a non-invasive bladder volume measurement in childrenScand J Urol Nephrol422008444448
- B.AlnaifH.P.DrutzThe accuracy of portable abdominal ultrasound equipment in measuring postvoid residual volumeInt Urogynecol J101999215218
- E.BrightR.PearcyP.AbramsUltrasound estimated bladder weight in men attending the uroflowmetry clinicNeurourol Urodyn302011583586
- S.E.ElsamraZ.GordonP.I.EllsworthThe pitfalls of BladderScan™ PVR in evaluating bladder volume in adolescent femalesJ Pediatr Urol720119597
- S.BózsaL.PótóJ.BódisL.HalvaxM.KoppánA.Aranyet alAssessment of postoperative postvoid residual bladder volume using three-dimensional ultrasound volumetryUltrasound Med Biol372011522529
- G.M.BeckersH.J.van der HorstJ.FrantzenM.W.HeymansThe BladderScan BVI 6200 (®) is not accurate enough for use in a bladder retraining programJ Pediatr Urol92013904909
- P.S.GoodeJ.L.LocherR.L.BryantD.L.RothK.L.BurgioMeasurement of postvoid residual urine with portable transabdominal bladder ultrasound scanner and urethral catheterizationInt Urogynecol J Pelvic Floor Dysfunct112000296300
- H.A.AntonK.ChambersJ.CliftonJ.TasakaClinical utility of a portable ultrasound device in intermittent catheterizationArch Phys Med Rehabil791998172175
- Y.H.HuangL.I.BihS.L.ChenS.J.TsaiC.H.TengThe accuracy of ultrasonic estimation of bladder volume: a comparison of portable and stationary equipmentArch Phys Med Rehabil852004138141