Abstract
Objective:
To compare the outcome of a modified onlay island flap (MOIF) with that of the Mathieu urethroplasty for distal hypospadias repair.
Patients and methods:
In a prospective randomised study, 60 patients with coronal, subcoronal and distal penile hypospadias, with a urethral plate width of ⩽6 mm, and minimal or no chordee, underwent either MOIF using a midline longitudinal outer preputial skin flap passed ventrally by penile buttonholing through dartos fascia incision, or a Mathieu urethroplasty. Closed envelopes were used for randomly selecting patients for each procedure. The operative duration, complications, cosmetic outcome, urinary stream and relatives’ satisfaction were reported for each procedure.
Results:
Preoperative data (patients’ age and site of urethral meatus) and operative duration were insignificantly different between the groups (P = 0.653, 0.786 and 0.710, respectively). There were no intraoperative complications in either group. The duration of follow-up was insignificantly different between the groups. Patients treated with the MOIF had a statistically significant lower complication rate (P = 0.036), and a better cosmetic outcome, urinary stream and relatives’ satisfaction (P < 0.001 for all).
Conclusions:
The MOIF urethroplasty seemed to be better than the Mathieu urethroplasty in patients with distal hypospadias and narrow urethral plates. Further studies including more patients, and a longer follow-up with an objective evaluation of functional outcome should be encouraged to confirm these early results.
Introduction
Hypospadias is among the most common congenital anomalies affecting males [Citation1], with distal hypospadias accounting for more than half of all cases [Citation2]. Several techniques have been attempted for its correction [Citation3]. The multiplicity of repair techniques reflects that none is totally satisfactory [Citation4]. Complications after hypospadias repair are common [Citation5]. Hence, new modifications of repair techniques are usually attempted with the aim of obtaining better results and fewer complications [Citation6].
The aim of the present study was to compare the outcome of a modified onlay island flap (MOIF) with the Mathieu urethroplasty for the repair of distal hypospadias.
Patients and methods
Between February 2011 and January 2013, this prospective randomised study included 60 patients with coronal, subcoronal and distal penile hypospadias, with a urethral plate (UP) of ⩽6 mm width, and minimal or no chordee. Patients with previous penile surgery (previous urethroplasty or circumcision) were excluded. The width of the UP was measured precisely in the operating room under anaesthesia. Using closed envelopes, patients were randomly divided into two equal groups. Patients in group 1 underwent the MOIF urethroplasty similar to the Hodgson II procedure [Citation7], with excision of the preputial skin lateral to the flap, unlike in the Hodgson II procedure.
Patients in group 2 underwent a perimeatal-based skin-flap urethroplasty according to the description by Mathieu in 1932, as described below. All patients were operated by the author under combined general and caudal epidural anaesthesia. Informed written consent was obtained from patients’ parent(s) or relative(s) before enrolment in the study, with guarantees of confidentiality. Study approval was obtained from the institutional scientific board and ethics committee.
The operative steps of MOIF urethroplasty ( and )
The first step was to place a traction suture at the dorsum of the glans penis distally, then place a suitably sized Nelaton catheter. The technique began with three incisions: (1) a U-shaped incision delineating the UP laterally and proximally, passing superficial to the distal urethral end; (2) a circumferential incision 1 cm proximal to the coronal sulcus (CS), made on the inner prepuce and deepened to the plane between the dartos layer and Buck’s fascia (proximally to the middle of the penis); and (3) a circumferential incision (corresponding to the circumcision incision) made on the penile skin and deepened to the plane between the skin and dartos layer proximally for ≈5 mm. The flap was fashioned using two longitudinal incisions made on the skin surface, beginning proximally at the circumferential skin incision and extending distally to the muco-cutaneous junction and deepened to the plane superficial to dartos fascia, and separated by a distance corresponding to the required flap width to create the neo-urethral floor ( and ).
Fig. 1 Operative steps of the MOIF urethroplasty; (A) skin incisions delineating the flap. (B) Excision of skin lateral to the flap. (C) Excision of the preputial mucosa with preservation of the dartos fascia. (D) Longitudinal incision of the dartos fascia. (E) Meatoplasty by excising excess preputial skin flush with the glans penis.
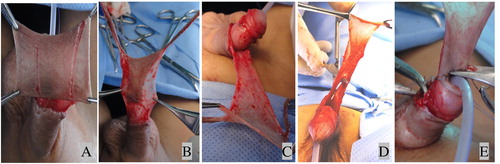
Fig. 2 Line drawings of the MOIF urethroplasty; operative steps. (A) Dorsal preputial skin incisions. (B) Excised skin lateral to the flap and dartos incision (dashed line). (C) Excision of the inner preputial layer and dorsal button-holing of the penis. (D) Suturing of the flap to the edges of the UP. (E) Dartos pedicles cover the suture lines. (F) Final appearance and the outer suture line.
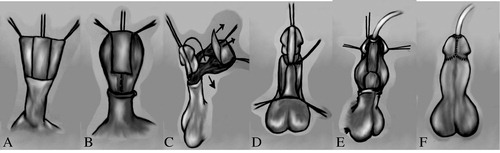
This was followed by excision of the preputial skin lateral to the flap ( and ), which is the main difference between the current MOIF and the Hodgson II procedure. The whole inner mucosal layer is excised with preservation with the whole dartos layer ( and ).
The dartos fascia (proximal to the flap) was longitudinally incised in the midline () and widened proximally, sparing the distal 2–3 mm of dartos layer, so as to allow easy passage of the penis dorsally by button-holing. The ventrally placed longitudinal rectangular skin flap was then sutured to the edges of the U-shaped incision, beginning at the transverse incision () followed by the two lateral incisions, beginning proximally and extending distally, using continuous 6–0 polyglactin running sutures. The glanular parts of the U-shaped incision were deepened to create generous glanular wings. The lateral pedicles and the transverse dartos fascia spared proximal to the flap (obligatory covering of the suture lines; ) were sutured in place using a few interrupted 6–0 polyglactin stitches.
The glanuloplasty was done by suturing the edges of the generous glanular wings together from the CS distally to a mid-glanular position. The muco-cutaneous incision was circumferentially sutured using a 6–0 polyglactin interrupted suture. The meatoplasty was done by excising the excess length of the flap flush with the glans penis (). Each side of the resultant V-shaped end of the flap was sutured to the corresponding glanular wing. A small Nelaton catheter (6 or 8 F) was left for bladder drainage. The final penile appearance and the outer suture line are shown in .
Operative steps of the Mathieu urethroplasty
After inserting a glanular fixing suture and a suitably sized Nelaton catheter, incisions were made as follows: (1) two incisions just lateral to the UP and extending proximal to the urethral meatus (UM) for a distance corresponding to required flap length. Those incisions were deepened at their glanular parts to create generous glanular wings. (2) a transverse incision connecting the proximal ends of the two longitudinal incisions. (3) another circumferential incision 5 mm proximal to the CS, with penile degloving. The urethroplasty was done by suturing the corresponding skin flaps and UP edges using a 6–0 polyglactin running subcuticular suture. No dartos layer was applied. The glanular wings were sutured using interrupted 6–0 polyglactin sutures. A midline incision of the prepuce was made, and Bayer’s flaps created for ventral skin coverage, with excision of the rest of the prepuce. A smaller catheter was left for bladder drainage.
Postoperative care (in both groups)
All patients had prophylactic antibiotic therapy for 7 days. Mildly compressive, paraffin-impregnated dressings, applied at the end of the procedure, were removed 3 days after surgery, and the catheters were removed 7 days after surgery. Follow-up visits were scheduled at 1 and 3 months, and every 3 months thereafter.
The preoperative patients’ data, operative data (duration and complications), postoperative results (penile cosmetic appearance, PCA), urinary stream, patients’ or relatives’ satisfaction, and complications, were reported. The cosmetic results were evaluated by urologists who were unaware of the type of repair. In a trial to develop an objective evaluation, a postoperative cosmetic evaluation score () was suggested, whereby urologists were asked to grade the external UM with scores of 1–3 (where 1, 2 and 3 are rounded or disfigured, irregular vertical slit-like and regular vertical slit-like meatus, respectively), CS and the penile shaft (PS) with scores of 1–3 (where 1, 2 and 3 are unsatisfactory, satisfactory and excellent, respectively). The sum of grades represents the PCA score, of 3–9 (where 3–4, 5–7 and 8–9 are considered unsatisfactory, satisfactory and excellent, respectively). The urinary stream was judged according to the caregiver in children who were not toilet-trained, and by the urologists in toilet-trained children. Abdominal ultrasonography, with evaluation of the postvoid residual urine volume, was offered to all patients at every visit.
Table 1 The suggested postoperative cosmetic evaluation score.
Data were analysed statistically, comparing groups using Pearson’s chi-squared test for categorical data and an independent sample t-test for quantitative data, with P < 0.05 considered to indicate significant differences.
Results
The patients’ age, site of native UM and the operative duration () were not significantly different between the groups (P = 0.653, 0.786 and 0.710, respectively). There were no intraoperative complications in either group. The mean (SD, range) follow-up in group 1 was 12.7 (4.3, 6–22) months and in group 2 was 11.7 (3.5, 6–19) months, and was not significantly different between the groups (P = 0.282). There were significantly fewer postoperative complications in the MOIF group (P = 0.036). The MOIF group had a highly statistically significantly better cosmetic appearance, shape of urinary stream and relatives’ satisfaction rating (P < 0.001 for all). shows the postoperative cosmetic results after MOIF urethroplasty. No patient in either group had a significant postvoid residual urine volume on abdominal ultrasonography.
Fig. 3 Cosmetic results of the MOIF urethroplasty show: (A) a vertical slit-like UM (score 3). (B) A disfigured UM, excellent CS and PS (score = 1 + 3 + 3 = 7; satisfactory PCA).
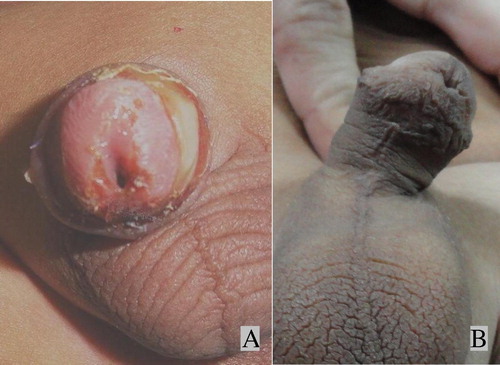
Table 2 Preoperative patient data, operative duration and postoperative data (complications, cosmetic appearance, shape of urinary stream and satisfaction of relatives).
Discussion
Hypospadias has challenged generations of reconstructive surgeons to restore as much normal function and appearance as possible [Citation8]. Although many techniques to repair hypospadias have been reported, no consensus has yet been defined on the best repair [Citation3]. Hence, surgical techniques for hypospadias repair are continuously being developed, aiming to overcome the shortcomings of the available methods [Citation4,Citation6].
Although the tubularised incised-plate (TIP) might be the most common procedure to repair distal hypospadias, because it is reportedly simple and gives better cosmetic outcomes than flap repairs [Citation8], in the TIP procedure some features of the UP, especially a flat and narrow plate, potentially increase the risk of complications, i.e., meatal stenosis and urethro-cutaneous fistula [Citation9]. In the present study patients had a narrow UP (⩽6 mm) and hence the TIP procedure was not an ideal treatment option.
An advantage of the MOIF technique is the use of preputial skin, which is often available, is hairless and large enough to construct the defective urethral floor, and is often otherwise discarded.
In the present study the Mathieu urethroplasty group had complications in six patients, with a urethro-cutaneous fistula occurring in four (13%). These results are in accordance with those of others, who reported a similar fistula rate (2–21%) in their study [Citation10]. In the Mathieu technique a longer flap is associated with a greater possibility of a decreased blood supply to the distal-based flap, resulting in a higher incidence of fistula [Citation11].
However, no urethro-cutaneous fistula was detected in patients who underwent the MOIF technique. This might be because: (i) the whole skin flap is well vascularised, as it depends on the longitudinally incised and minimally interrupted dartos layer, and hence the flap length might not influence the fistula rate; (ii) the ample width of the flap ensures tension-free suturing of the flap; and (iii) the interposition of a full-thickness, well-vascularised dartos fascia between the suture lines.
Although the benefit of using the dartos layer as a second covering layer interposed between the inner and outer suture lines in reducing the incidence of urethro-cutaneous fistula is questionable [Citation12–Citation14], in the MOIF procedure, the dartos fascia lateral to the flap and the preserved distal end of dartos fascia just proximal to the flap inevitably cover all the inner suture line, acting as a second layer interposed between it and the outer suture line.
After hypospadias repair the functional and cosmetic outcomes are generally assessed subjectively, and a standardised evaluation of these outcomes is urgently needed [Citation15]. In the present study, trying to be more objective, a scoring system was developed to assess the cosmetic outcome. Holland et al. [Citation16] evaluated a ‘hypospadias objective scoring evaluation’ (HOSE) for assessing the results of hypospadias surgery. Although the HOSE system evaluated the postoperative results for meatal location and shape, the urinary stream, the presence of curvature and the presence of fistula, the present suggested scoring system is simpler and more specific in evaluating the cosmetic outcome, as it does not overlook features that are important in the cosmetic appearance of the penis, e.g., the cosmetic appearance of the CS and PS.
In the present study the MOIF technique gave a significantly better cosmetic appearance of the UM, CS and PS, and consequently a better PCA than did the Mathieu urethroplasty. The Mathieu technique is usually criticised for its unsatisfactory cosmetic outcome, especially the meatal configuration [Citation17]. The better cosmetic outcome of the MOIF procedure might be attributed to several causes: (i) the meatoplasty was made by excising the excess length of the well-vascularised flap flush with the glans penis, and suturing each side of the resultant V-shaped end of the flap to the corresponding glanular wing, with the consequent creation of a slit-like meatus in all cases. (ii) Leaving the ventral PS skin uninterrupted logically results in a better cosmetic outcome. (iii) In the MOIF technique the CS had a better cosmetic appearance than in the Mathieu procedure, and this might be attributed to the simple suturing of the preserved inner preputial mucosa to the penile skin, as in circumcision, in the former rather than suturing it to Bayer’s flap in the latter.
Theoretically, although a transverse onlay island flap obtained from the inner preputial mucosa might offer the advantages of the longitudinal cutaneous flap obtained in MOIF technique, an asymmetric rotational dartos (in the former procedure) might cause penile rotation, as the flap rotates around one side of the PS [Citation18]. In the MOIF technique, midline splitting of the pedicle (to permit dorsal penile buttonholing) did not cause postoperative penile rotation in any case.
Closely similar modifications of the onlay island flap have been attempted [Citation7,Citation19–Citation21]. A few but critical differences between the present MOIF and these modifications can be clarified. In the present study the UP was preserved in all cases, forming the urethral roof. However, in previous modifications [Citation19–Citation21] the UP was often excised, with tubularisation of the flap or reconstructing the roof using a buccal mucosa graft. Although preputial skin lateral to the flap was preserved and rotated ventrally to share in PS coverage in the previous techniques [Citation7,Citation19–Citation21], it was excised with circumferential suturing of the penile skin to the remaining part of the inner prepuce (as in circumcision) in the present technique. This might improve the cosmetic appearance of the CS and PS, and consequently the PCA.
The mean operative duration in present MOIF group was 156.5 min; this is in agreement with the results of Scuderi et al. [Citation20], who reported a mean operative duration of 115–210 min. They noted that the mean time decreased rapidly after the early cases.
No postoperative complications were detected in the present MOIF group. This is not in accordance with the results of closely similar techniques. Scuderi et al. [Citation20] reported early postoperative complications in 8.6% of cases, that decreased to 2% during the follow-up, with conservative or non-surgical interventions. Also, Djordjevic et al. [Citation21] reported the development of postoperative complications in three of 17 patients (18%). These differences might be attributed to the different inclusion criteria, where previous studies included more severe degrees of hypospadias. Preservation of the UP in the present study, rather than plate excision with tubularisation of the flap, as practised by Scuderi et al. [Citation20], or plate excision with replacement with buccal mucosa, as done by Djordjevic et al. [Citation21] might have a role in reducing the complication rate.
The limitations of the present study include the relatively short follow-up. However, in a recent study, Snodgrass et al. [Citation22] found that most complications of urethroplasty are diagnosed within the first year after hypospadias repair. Although the penile cosmetic scoring system might minimise intra- and inter-observer variations, it should be validated. Another limitation is the subjective evaluation of the functional outcome. Uroflowmetry before and after surgery is recommended to ensure an objective evaluation.
In conclusion, the MOIF urethroplasty seems to be better than the Mathieu repair in patients with distal hypospadias associated with narrow UPs. Further studies including more patients and a longer follow-up, with an objective evaluation of the functional outcome, are recommended to confirm these early results. Evaluation of the technique in patients with a hypoplastic distal urethra and in those with mid and proximal penile hypospadias and moderate chordee might extend its indications to these areas.
Conflict of interest
None.
Source of funding
None.
Acknowledgements
I thank Dr. Abdelhafez MF for his effort and time in making the statistical analysis of the results. I also thank Dr. Abdelrahman MA for his perseverance and time in making the line drawings of the operative steps, and assistance in development of the line drawings of the postoperative cosmetic evaluation score. I acknowledge the team of my department who helped in the development of this work. I also wish to thank my patients, who accepted to share in this study.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- H.FischG.HyunT.W.HensleRising hypospadias rates: disproving a mythJ Pediatr Urol620103739
- S.CanonB.MosleyJ.ChipolliniJ.A.PurifoyC.HobbsEpidemiological assessment of hypospadias by degree of severityJ Urol188201223622366
- A.MacedoJr.A.RondonV.OrtizHypospadiasCurr Opin Urol222012447452
- A.M.GhaliHypospadias repair by skin flaps. A comparison of onlay preputial island flaps with either Mathieu’s meatal-based or Duckett’s tubularized preputial flapsBJU Int831999102110
- A.RickwoodP.AndersonOne-stage hypospadias repair. Experience of 367 casesBr J Urol671991424428
- A.KissP.NyirádyL.PirótM.MerkszCombined use of perimeatal-based flap urethroplasty (Mathieu) with midline incision or urethral plate in hypospadias repairEur J Pediatr Surg132003383385
- N.B.HodgsonHypospadias and urethral duplicationsJ.H.HarrisonR.F.GittesA.D.PerlmutterT.A.StameyP.C.WalshCampbell’s Urologyvol. 21979WB Saunders CoPhiladelphia15791580
- W.T.SnodgrassHypospadiasA.J.WeinL.R.KavoussiA.C.Novicket alCampbell-Walsh Urology, 10th ed.vol. 82012Elsevier, SaundersPhiladelphia35033514
- O.SarhanM.SaadT.HelmyA.HafezEffect of suturing technique and urethral plate characteristics on complication rate following hypospadias repair: a prospective randomized studyJ Urol1822009682686
- E.YesildagG.TekantN.SarimuratS.N.BuyukunalDo patch procedures prevent complications of the Mathieu technique?J Urol171200426232625
- S.A.BoddyM.SamuelA natural glanular meatus after ‘Mathieu and a V incision sutured’: MAVISBJU Int862000394397
- B.A.KamalDouble dartos flaps in tubularized incised plate hypospadias repairUrology66200510951098
- W.T.SnodgrassM.A.KoyleL.S.BaskinA.A.CaldamoneForeskin preservation in penile surgeryJ Urol1762006711714
- M.SuoubS.DaveY.El-HoutL.H.BragaW.A.FarhatDistal hypospadias repair with or without foreskin reconstruction: a single-surgeon experienceJ Pediatr Urol42008377380
- A.GiannantoniHypospadias classification and repair: the riddle of the SphinxEur Urol60201111901191
- A.J.HollandG.H.SmithF.I.RossD.T.CassHOSE: an objective scoring system for evaluating the results of hypospadias surgeryBJU Int882001255258
- M.SamuelS.CappsA.WorthyDistal hypospadias: which repair?BJU Int9020028891
- M.L.DjordjevicS.V.PerovicZ.SlavkovicN.DjakovicLongitudinal dorsal dartos flap for prevention of fistula after a Snodgrass hypospadias procedureEur Urol5020065357
- S.V.PerovicV.VukadinovicOnlay island flap urethroplasty for severe hypospadias. A variant of the techniqueJ Urol1511994711714
- N.ScuderiS.ChiummarielloF.De GadoCorrection of hypospadias with a vertical prepucial island flap: a 23 years experienceJ Urol175200510831087
- M.L.DjordjevicM.MajstorovicD.StanojevicM.BizicV.KojovicV.Vukadinovicet alCombined buccal mucosa graft and dorsal skin flap for repair of severe hypospadiasUrology712008821825
- W.SnodgrassC.VillanuevaN.C.BushDuration of follow-up to diagnose hypospadias urethroplasty complicationsJ Pediatr Urol102014208211
