Abstract
Objectives:
To assess the practice of testicular prosthesis insertion (TPI) related to orchidectomy in one geographical region and to identify the difference in the rates of insertion among different age groups.
Patients and methods:
Males who underwent orchidectomy between 1989 and 2009 were identified from data collected from Scottish Morbidity Records. Patients were classified into six age groups. The TPI rate and relation to original orchidectomy were analysed according to different age groups.
Results:
In all, 3364 patients underwent orchidectomy in the 20-year period of the study. The most common indications for orchidectomy were atrophy, undescended testes, torsion, and tumour. In the same period, 530 patients had a TPI, with 59.4% of them (316 patients) having TPI at initial surgery, 17.3% (92) as a second surgical procedure, and 22.8% (122) having the TPI without prior history of orchidectomy. Among patients who underwent TPI, postpubertal males were more likely to have simultaneous insertion at the time of orchidectomy than prepubertal males (83% vs 32%; odds ratio 10.44, 95% confidence interval 5.23–20.82; P < 0.01).
Conclusion:
Younger males are more likely to have TPI at a later date. Paediatric urologists should be mindful of the possibility of concurrent TPI at the time of initial scrotal/groin exploration.
Introduction
The presence of normal testes bilaterally plays an important role in the normal psychological development of young males and absence of a testis can have potential consequences as a result of loss of body image or masculinity [Citation1,Citation2]. Absence of an intrascrotal testis can be found in male patients at different ages, and this can be caused by agenesis, failure of normal testicular descent, or surgical removal. Orchidectomy is a common urological procedure and indications vary from benign conditions such as trauma or infection to testicular cancers.
In patients with absent testis, testicular prosthesis insertion (TPI) may be offered for cosmetic or psychological purposes. In appropriately sized patients, TPI can be done at the time of orchidectomy or as a subsequent elective procedure. Most patients report high levels of satisfaction after TPI [Citation3,Citation4]. In younger prepubertal boys, TPI at the time of surgery may not be appropriate due to difficulty in choosing the appropriate size of prosthesis and issues of informed consent.
In the present study, we aimed to identify the past and current indications for orchidectomy and the practice of TPI in one geographical region of the UK represented by the West of Scotland.
Patients and methods
This is a population-based retrospective study using a cohort of male patients who underwent orchidectomy in the City of Glasgow, Scotland over a 20-year period (1989–2009). This cohort was identified from the Scottish Morbidity Records (SMR) [Citation5]. The SMR capture all episodes relating to inpatients and day-case patients discharged from non-psychiatric and non-obstetric wards in Scottish hospitals. Patients are provided with a unique identifying number that is used for clinical and research purposes.
From this cohort we identified males who underwent TPI using the SMR over the specified period using the unique identifying number. Data on the indications of orchidectomy and TPI were extracted from case notes review. This study has received approval from the Research Ethics Board and was conducted with accordance to the regulations of our local Audit Department.
The main outcomes for this study were the indications for orchidectomy in different age groups and the uptake of TPI in each of these groups.
Statistical analysis was performed using Statistical Package for the Social Sciences software SPSS Inc. (2007) Version 16.0. Chicago. We used the chi-squared test for the groups to determine the odds ratios (ORs).
Results
In all, 3364 patients were identified who had orchidectomy over the 20-year period. Those patients were subsequently divided into six age groups for statistical analysis as follows: 1, <13; 2, 13–15; 3, 16–20; 4, 21–30; 5, 31–40; and 6, >40 years.
This age thresholds have been used to distinguish between the paediatric age group, adolescents, and young adults. The distribution of orchidectomy across different age groups is shown in . The most frequent indications for orchidectomy are summarised in . The most common indications in pre- and peripubertal boys were atrophy, undescended testis and torsion, with malignancy becoming more common after the age of 16 years. Bilateral orchidectomy for hormonal manipulation in prostatic cancer was exclusive to the older age groups.
Table 1 The practice of orchidectomy across all age groups.
Table 2 Age distribution of the common indications for orchidectomy.
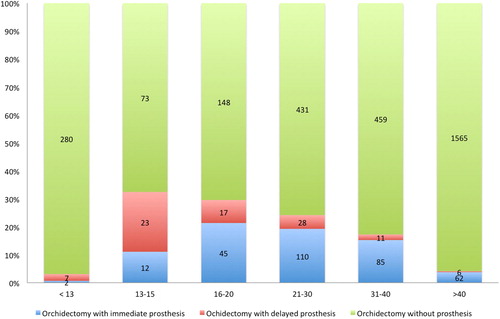
From this cohort we identified 530 patients who underwent TPI. The procedure was performed concurrently with orchidectomy in 316 patients (59.4%), while 92 (17.3%) had TPI performed at a later stage. In 122 patients (22.8%), TPI was undertaken without a previous record of orchidectomy. The rate of TPI and the timing related to orchidectomy were determined and are shown in .
Universally, the uptake of TPI was low and was performed (immediately or at a later stage) in only 15.76% of those patients undergoing orchidectomy. TPI particularly at the time of orchidectomy was more common in the older age groups (except the advanced age group). For patients who had TPI, those aged >16 years were more likely to have TPI at the same time as the original orchidectomy [302/364 (83%)] than patients aged <16 years [14/44 (32%)], OR 10.44 (95% CI 5.23–20.82; P < 0.01).
Discussion
The present study represents one of the largest orchidectomy and TPI cohorts in the literature. We considered all males undergoing orchidectomy in a single geographical region over a 20-year period and found a universally low rate of TPI, which is more marked in children and adolescents. Several surveys have considered the impact of loss of testis on the psychological wellbeing of affected males. Skoogh et al. [Citation6] from the Swedish-Norwegian Testicular Cancer Group reported a significant proportion of men that underwent orchidectomy for non-seminomatous germ cell testicular cancer had feelings of loss and long-lasting shame, as well as loss of sexual desire as a result of orchidectomy. Testicular prosthesis or implants were introduced to give a sense of fullness in the scrotum and avoid psychological trauma. Modern day testicular prostheses are available in different sizes and made of silicone filled with gel or saline [Citation7,Citation8]. High satisfaction rates of patients after TPI are well documented and counselling patients for about TPI is an essential part in consenting patients undergoing orchidectomy [Citation9–Citation11].
The indications for orchidectomy in our present cohort were consistent with other reports [Citation12,Citation13]. While testicular atrophy was the leading indication for orchidectomy in the age groups <15 years, undescended testes is still a significant indication for orchidectomy, particularly in those aged 16–20 years. This may be explained by the fact that missed undescended testis usually presents at a later stage and surgery is usually advised due to the high risk of testicular cancer. Zaidi et al. [Citation14] reached similar conclusions in their systematic review of orchidectomy and TPI in the paediatric population. In the older groups, orchidectomy for tumours accounts for a substantial proportion of procedures, with the highest incidence in the 31–40 year age group. Bilateral orchidectomy for the management of metastatic prostate cancer was prevalent in those aged >40 years, although there has been a general decline in this procedure as a result of the introduction of medical castration [Citation15]. However, recent guidelines are in favour of bilateral orchidectomy as a result of proven efficacy and better cost-effectiveness, especially when castrate levels of testosterone are urgently required [Citation16].
During the present study period, only 530 patients underwent TPI. The highest rate of TPI was seen in the males aged 13–30 years, perhaps reflecting the consciousness about self-image that is most prominent in this age group. However there are a large number of males with prior orchidectomy who did not undergo TPI. Given the retrospective nature of the present study, it is not possible to determine if testicular prosthesis was offered by the treating physician and declined by the patients, or whether no offer was made. Moynihan [Citation17] interviewed 102 patients with testicular prosthesis and found that only 28% were offered TPI as part of their counselling for orchidectomy and only 18% of those agreed to have one. On reflection, patients not offered TPI did not report concerns about loss of body image. Men who are in stable relationships are less likely to request a prosthesis after orchidectomy for cancer, with >50% of married men reporting satisfaction with body image without a prosthesis [Citation18]. Our present study also identified 122 men (23%) who had TPI with no previous history of orchidectomy. This may be due to inconsistencies in reporting, previous surgery being undertaken outside the region, previous testicular trauma without surgery, or testicular agenesis/atrophy. An improvement in surgical coding is required to ensure accurate data entry for future research purposes.
Our present findings further confirmed that a number of prepubertal males requested TPI at a later stage following their orchidectomy (30/397, 8%). This implies increased awareness of body image later during puberty and adulthood, but the uptake remains low. Our present data may underestimate the number of young boys undergoing TPI after orchidectomy in early childhood, as some of those patients may wish to have TPI at a later stage of life or when they are sexually active. Many of these boys will have been discharged from paediatric services and will require referral to adult urologists, and GPs should be aware of this option. The pathway by which men presented for TPI at a later date is not clear, but the anecdotal experience of the authors suggests that these boys/men often self-present for referral to specialist services. There may be a disinclination to self-present related to embarrassment or reluctance to undergo another general anaesthetic. TPI at the time of original orchidectomy may increase the rate of uptake.
There is a general belief that younger men should not be offered TPI at the time of surgery because of an underdeveloped scrotum [Citation19]. Zilberman et al. [Citation20] interviewed 19 young adults who had TPI at early childhood and demonstrated good satisfaction rates in 62% of them. They concluded that the procedure can safely be performed at a young age. The pathology leading to orchidectomy may well influence the concurrent TPI. Younger boys were more likely to undergo an orchidectomy due to torsion or other inflammatory conditions and it would be unadvisable to perform TPI in this setting. A robust follow-up service is required to ensure that patients and families are aware of the possibility of TPI to optimise uptake.
Limitations of the present study include the retrospective nature of data collection, which could affect the results, especially as there were no local guidelines at the time of writing of the manuscript that govern TPI. Another limitation of the present study is the lack of data on patients’ satisfaction, the marital status of the patient, type of prosthesis, and complications after insertion.
Conclusions
The present study provides a ‘snapshot’ on the practice of TPI in the male population in the West of Scotland. It has shown inconsistencies in the rate of TPI, although it is not clear whether this is caused by failure of adequate counselling of patients or patient choice. Adequate mechanisms should be available for paediatric and prepubertal males after orchidectomy to offer TPI at a later stage. We hope that the present study will raise awareness and lead to robust systems in paediatric hospitals or GP surgeries to ensure adult patients with previous orchidectomy are counselled about TPI and to arrange referrals to adult urologists if necessary.
Conflicts of interest
None of the authors of this paper have any conflict of interests.
Source of funding
None.
Acknowledgement
The authors received no financial support for study design, data extraction, and dissemination of results through national and international conferences or writing the manuscript.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- R.M.FriedmanThe role of the testicles in male psychological developmentJ Am Psychoanal Assoc441996201253
- M.GurevichS.BishopJ.BowerM.MalkaJ.Nyhof-Young(Dis)embodying gender and sexuality in testicular cancerSoc Sci Med58200415971607
- L.IncrocciJ.L.BoschA.K.SlobTesticular prostheses: body image and sexual functioningBJU Int84199910431045
- M.J.LynchJ.P.PryorTesticular prostheses: the patient’s perceptionBr J Urol701992420422
- K.HarleyC.JonesQuality of Scottish Morbidity Record (SMR) dataHealth Bull (Edinb)541996410417
- J.SkooghG.SteineckE.Cavallin-StahlU.WilderängU.K.HåkanssonB.Johanssonet alFeelings of loss and uneasiness or shame after removal of a testicle by orchidectomy: a population-based long-term follow-up of testicular cancer survivorsInt J Androl342011183192
- D.BodiwalaD.J.SummertonT.R.TerryTesticular prostheses: development and modern usageAnn R Coll Surg Engl892007349353
- P.J.TurekV.A.MasterTesticular Prosthesis Study G. Safety and effectiveness of a new saline filled testicular prosthesisJ Urol172200414271430
- J.MoneyR.SollodBody image, plastic surgery (prosthetic testes) and Kallmann’s syndromeBr J Med Psychol5119789194
- R.RobinsonC.TaitN.ClarkeV.RamaniIs it safe to insert a testicular prosthesis at the time of radical orchidectomy for testis cancer: an audit of 904 men undergoing radical orchidectomyBJU Int2014 10.1111/bju.12920 [Epub ahead of print]
- E.XylinasG.MartinacheV.AzancotD.Amsellem-OuazanaD.SaighiT.Flamet alTesticular implants, patient’s and partner’s satisfaction: a questionnaire-based study of men after orchidectomyProg Urol18200810821086
- P.AlbersW.AlbrechtF.AlgabaC.BokemeyerG.Cohn-CedermarkK.Fizaziet alEAU guidelines on testicular cancer: 2011 update. European Association of UrologyActas Urol Esp362012127145
- J.M.MansbachP.ForbesC.PetersTesticular torsion and risk factors for orchiectomyArch Pediatr Adolesc Med159200511671171
- T.ZaidiL.HendersonA.AzizA.MorabitoA.DicksonTesticular Prosthesis, First Systematic Review In Paediatric PopulationJ Pediatr Urol5Suppl. 12009S80
- L.J.Melton3rdK.I.AlothmanS.J.AchenbachW.M.O’FallonH.ZinckeDecline in bilateral orchiectomy for prostate cancer in Olmsted county, Minnesota, 1956–2000Mayo Clin Proc76200111991203
- V.RohdeK.GrabeinF.HesselU.SiebertJ.WasemOrchiectomy versus medical therapy with LH-RH analogues for the treatment of advanced prostatic carcinomaGMS Health Technol Assess22006Doc13
- C.MoynihanTesticular cancer: the psychosocial problems of patients and their relativesCancer Surv61987477510
- E.R.GritzD.K.WellischH.J.WangJ.SiauJ.A.LandsverkM.D.CosgroveLong-term effects of testicular cancer on sexual functioning in married couplesCancer64198915601567
- J.S.ElderM.A.KeatingJ.W.DuckettInfant testicular prosthesesJ Urol141198914131415
- D.ZilbermanH.WinklerN.KleinmannG.RavivB.ChertinJ.Ramonet alTesticular prosthesis insertion following testicular loss or atrophy during early childhood – technical aspects and evaluation of patient satisfactionJ Pediatr Urol32007461465