Abstract
Objective:
To assess the long-term follow-up after ileocaecal continent cutaneous reservoir (ICCR) and to review the late complications.
Patients and methods:
In all, 756 patients underwent an ICCR in our department, with long-term follow-up data available in 50 patients. The inclusion criterion was ICCR regardless of the indication and the exclusion criteria were orthotopic neobladder or other continent urinary diversions not performed with the ileocaecum. Patients were followed to record primary outcomes and late complications. Complications were stratified according to the Clavien–Dindo classification.
Results:
The mean patient age was 44 years and pelvic malignancies were the first indication for urinary diversion. The mean (range) follow-up was 19 (9–36) years. A stoma stenosis was the most frequent outlet-related complication requiring re-intervention, followed by ischaemic outlet degeneration, and stoma incontinence. Six renal units (RUs) developed obstruction at the anastomotic site and were managed by open surgery. Three RUs had to be removed due to deterioration. A dederivation was necessary in three patients (6%).
Conclusion:
The ICCR is a safe and established technique when an orthotopic pouch is impossible. The long-term follow-up shows acceptable complication rates and satisfactory continence conditions. However, large population studies are necessary to confirm this observation.
Introduction
Catheterisable pouches are good alternatives in patients with continent cutaneous urinary diversion when neobladder reconstruction is contraindicated [Citation1]. The natural anti-reflux mechanism of the ileocaecal valve and the peristalsis of the prevalvular ileal segment serve as the continence mechanism [Citation2]. Since 1983, several interesting techniques have been described for the cutaneous Mainz I pouch to simplify the surgery and to decrease long-term complications, with the efferent segment being the most problematic portion of the reservoir [Citation3–Citation6].
Patients and methods
Between January 1976 and January 2012, 756 patients underwent an ileocaecal continent cutaneous urinary diversion in our department for different pathologies. The long-term follow-up survey concerned only 50 patients whom data were available. The inclusion criterion was an ileocaecal continent cutaneous reservoir (ICCR) regardless of the indication and the exclusion criteria were orthotopic neobladder or other continent urinary diversions not performed with ileocaecum.
Operative technique
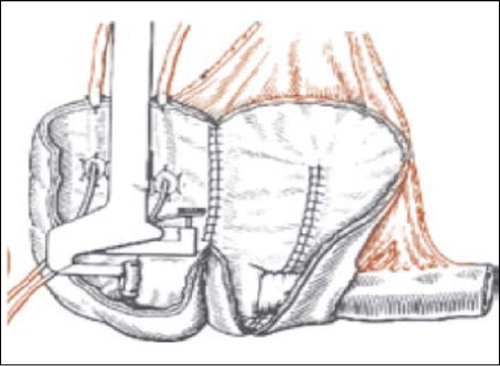
After performing cystectomy, the reservoir was created from 10–15 cm of caecum and right colon, and two adjacent ileal buckles of the same length, followed by antimesenteric opening and spherical reconfiguration of the ileocaecal segment. The ureters were implanted using submucosal tunnels as an anti-reflux mechanism. The intussuscepted terminal ileum, fixed by staples, served as the continence mechanism () [Citation1,Citation7,Citation8].
Patients were followed by clinical examination, biology and imaging once a year to record primary outcome and late complications related to the reservoir (continence, uretero-intestinal anastomosis). Complications were stratified according to the Clavien–Dindo classification of surgical complications [Citation9].
Results
The mean (range) patient age was 44 (22–60) years and the male to female ratio was 2:1. Pelvic malignancies were the main indication for cystectomy and urinary diversion, followed by the bladder dysfunction related to various benign causes (). Two adult patients with a long history of unsatisfactory hypospadias repair and serious urethral and bladder wall damage underwent this procedure, as well as two other patients with complicated section of the urethra (bladder infection and dysfunction related to long-term cystostomy).
Table 1 Indications for the ileocaecal continent cutaneous urinary diversion.
The mean (range) follow-up was 19 (9–36) years and patients were at different time points from the date of surgery to the last follow-up. The complications found particularly concerned the efferent segment (Grade IIIb) (). Treatment consisted of re-interventions for stoma stenosis, the creation of a new outlet for ischaemic degeneration, and reservoir revision for stomal incontinence. For neobladder calculi, two patients were managed by endoscopy (Grade IIIa), while six open interventions were necessary to extract huge stone masses (Grade IIIb). Six renal units (RUs) had urinary obstruction at the anastomotic area and were managed by open surgery (Grade IIIb), and two RUs had to be removed because of renal deterioration (Grade IVa). Renal calculi were found in a total of 12 RUs (). Kidney stones were treated by ESWL (Grade III) (six RUs) or by percutaneous lithotripsy (Grade IIIb; three RUs). Ureteric stones were treated by ESWL (Grade III, one RU), endoscopic stone removal (Grade IIIb, one RU) or by ureterolithotomy (Grade IIIb, one RU). A dederivation was necessary in two cases (4%) due to a severe deterioration in renal function and metabolic disorders (Grade IIIb).
Table 2 Late complications of the Mainz I pouch.
Table 3 Management of stones.
The daytime continence rate was 70% (35/50) (). Five patients (10%) with an ileocaecal reservoir required clean intermittent catheterisation, whereas the other patients were able to void spontaneously with insignificant post-void residual urine volumes. Renal function was preserved in 15 patients (30%), with a mean serum creatinine of 140 μmol/L. While 10 patients (20%) developed moderate chronic renal failure, with a mean serum creatinine of 195 μmol/L, evident from 10 years after the performance of the Mainz Pouch I urinary diversion.
Table 4 Continence rate.
Discussion
Continent cutaneous urinary diversion surgery is based on designing a high-capacity and low-pressure reservoir, with quick and simple clean voiding by periodic self-catheterisation, facilitating renal functional preservation and acceptable continence rates during the day and night [Citation10]. The continent cutaneous ileocaecal reservoir (Mainz pouch, ‘mixed augmentation ileum ‘n zecum’) was performed in 1983 using 10–15 cm of caecum and right colon and two adjacent ileal buckles of the same length [Citation7]. Since then, several modifications have been introduced over the years due to nipple valve problems. Actually, the technique uses a reinforced intact ileocecal valve for the continence mechanism [Citation11]. In a recent review, the pouch-related late complication rate was 37% [Citation12]. Late complications include stomal failure, problems related to ureteric re-implantation, stomal stenosis of the ileal nipple, pouch calculi, and incontinence [Citation11,Citation13].
In a prospective trial reported by Hardt et al. [Citation14] (level of evidence 2), the reported overall patient satisfaction was high for both conduit diversion and continent cutaneous diversion. A similar study was published in 2004 [Citation15], which reported a small increase in ‘mental’ quality of life (QoL) and an insignificant decrease in ‘physical’ QoL, when comparing preoperative with 1-year follow-up data. Similar results, despite differences between groups, have been obtained in five retrospective trials (level of evidence 3) [Citation16–Citation20]. These trials all mentioned that stomal dysfunctions were frequent.
In a large meta-analysis by Madersbacher et al. [Citation21], a follow-up of ⩾5 years duration after ileal conduit diversion was performed (level of evidence 3). In that meta-analysis, 10% of patients developed stenosis of the uretero-intestinal anastomosis, and 20% developed upper tract stones (this number increased to 38% after 10 years). In our present study, stoma stenosis occurred in 30% of the patients. Morphological and functional deterioration developed in 27% of the patients, mostly in the form of hydronephrosis or a reduced cortical kidney index. Renal failure was present in 40% of the patients after 5 years; this increased to 80% after 10 years. Iborra et al. [Citation22] reported impaired renal function in 14% of patients followed for 10 years.
Numerous retrospective studies have reported renal functional and morphological deterioration rates of between 13% and 41% after ileal diversion (levels 2 and 3) [Citation21,Citation23,Citation24]. After continent cutaneous diversion, Kristjansson et al. [Citation25] reported a decrease in renal function in 28% of patients 11 years after caecal reservoir creation. Akerlund et al. [Citation26] reported upper tract dilatation at a mean of 6.6 years after the performance of the Kock pouch (continent ileal reservoir) in five of 17 patients (29%); this was connected with scarring in two cases. Only one patient (6%) had an abnormal creatinine at last follow-up, and other four patients had a low age-adjusted GFR (three of these patients had had a low GFR preoperatively). Thoeny et al. [Citation27] reported a prospective description of renal morphology and function in 76 patients with a median follow-up of 84 months (level 2). Serum creatinine and IVU were performed preoperatively and at precise intervals postoperatively. Among 148 uretero-RUs, 141 (95%) showed no significant change in size or swelling of the parenchyma. In six RUs (4%), renal size and parenchymal thickness decreased, and in one RU there was a decrease in parenchymal thickness.
The prevalence of upper tract calculi in patients with urinary diversions is related to the type of diversion performed. Turk et al. [Citation28] reported no upper tract calculi in continent urinary diversions after a median (range) follow-up of 3.1 (0.5–10.5) years, including 33 patients with Indiana pouches and seven with orthotopic diversions (Hautmann pouch). A defect of that study was the small cohort and limited follow-up. However, with a longer follow-up (median 9 years, range 5 to 16) Pfitzenmaier et al. [Citation29] found renal stones in 13 of 94 (14%) patients after a Mainz I pouch urinary diversion in which the ileocecal valve, as with an Indiana pouch, was used. The resection of the ileocaecal valve causes increased bowel transit time, which leads to a loss of bile acids and small bowel bacterial overgrowth, resulting in deconjugation of bile acids. Consequently, there is a decrease in the availability of bile acids for micellar formation of fatty acids [Citation30]. In detail, intraluminal calcium binds preferentially with these fatty acids (fat saponification). Therefore, less free calcium is available to precipitate dietary oxalate, leaving much more soluble oxalate for absorption [Citation31]. Another factor that may promote renal stone formation after continent urinary diversion includes dehydration, which results from the hypovolemic salt losing condition associated with ileal reservoirs [Citation32]. However, this mainly occurs in the early postoperative period, during which none of our present patients developed calculi [Citation32].
Stoma stenosis is a frequent outlet complication of cutaneous urinary diversions [Citation5,Citation33]. A higher rate of stoma stenosis has been reported for the appendix stoma in some series as compared with the intussuscepted ileal nipple, and corroborates the correlation between the diameter of the efferent segment and the risk of stoma stenosis [Citation33]. The rate of pouch stones was twice as high for the intussuscepted ileal nipple as compared with the appendix stoma in our present series. An association between the use of metal staples for fixation of the efferent segment and the incidence of pouch stone formation has previously been reported in continent urinary diversion [Citation5]. Complication rates of different ureteric re-implantation techniques (anti-refluxive by Le Duc/Goodwin or refluxive end-to-side anastomosis) were studied in patients who underwent continent urinary diversion by means of the cutaneous Florida pouch [Citation33]. Strictures were found in 13.3% and 12.5% with tunnelled re-implantation and in 4.9% and 6.3% with end-to-side anastomosis of the ureters; however, the rate of refluxing RUs was higher in the latter group (7.0% vs 3.3%).
The present study has some limitations related to the retrospective nature of the trial and the number of included patients. Therefore, a larger prospective randomised multicentre trial is recommended to assess the findings of the present study in order to minimise late complications of the Mainz I pouch.
In conclusion, the cutaneous ileocecal pouch (Mainz I pouch) is a safe and established technique when an orthotopic pouch is not possible. The long-term follow-up shows acceptable complication rates and satisfactory continence conditions, but metabolic disorders must be prevented to maximally preserve the RUs.
Conflicts of interest
Authors have no conflict of interest to declare.
Source of funding
Authors have no funding to disclose.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- M.RinkL.KluthE.EichelbergM.FischR.DahlemContinent catheterizable pouches for urinary diversionEur Urol Suppl92010754762
- R.K.GilchristJ.W.MerricksH.H.HamlinI.T.RiegerConstruction of a substitute bladder and urethraSurg Gynecol Obstet901950752760
- E.W.GerharzU.KöhlK.WeingärtnerM.D.MelekosR.BonfigH.RiedmillerComplications related to different continence mechanisms in ileocecal reservoirsJ Urol158199717091713
- E.W.GerharzU.N.KöhlM.D.MelekosR.BonfigK.WeingärtnerH.RiedmillerTen years’ experience with the submucosally embedded in situ appendix in continent cutaneous diversionEur Urol402001625631
- D.G.HolmesJ.B.TrasherG.Y.ParkD.C.KuekerJ.W.WeigelLong-term complications related to the modified Indiana pouchUrology602002603606
- C.WebsterR.BukkapatnamJ.D.SeigneJ.Pow-SangM.HoffmanM.Helalet alContinent colonic urinary reservoir (Florida pouch): long term surgical complications (greater than 11 years)J Urol1692003174176
- J.W.ThüroffP.AlkenH.RiedmillerU.EngelmannG.H.JacobiR.HohenfellnerThe Mainz Pouch (mixed augmentation ileum and cecum) for bladder augmentation and continent diversionJ Urol13619861726
- M.FischJ.W.ThüroffContinent cutaneous diversionBJU Int102200813141319
- D.DindoN.DemartinesP.A.ClavienClassification of surgical complications. A new proposal with evaluation in a cohort of 6336 patients and results of a surveyAnn Surg2402004205213
- C.WiesnerR.BonfigR.SteinE.W.GerharzS.PahernikH.Riedmilleret alContinent cutaneous urinary diversion: long-term follow-up of more than 800 patients with ileocecal reservoirsWorld J Urol242006315318
- J.W.ThüroffP.AlkenH.RiedmillerG.H.JacobiR.Hohenfellner100 cases of Mainz pouch: continuing experience and evolutionJ Urol1401988283288
- S.BaileyM.H.KamelE.A.EltahawyN.K.BissadaReview of continent urinary diversion in contemporary urologySurgeon1020123335
- A.LampelM.FischR.SteinD.Schultz-LampelM.HohenfellnerC.Eggersmannet alContinent diversion with the Mainz pouchWorld J Urol1419968591
- J.HardtD.FilipasR.HohenfellnerU.T.EgleQuality of life in patients with bladder carcinoma after cystectomy: first results of a prospective studyQual Life Res92000112
- J.HardtF.PetrakD.FilipasU.T.EgleAdaptation to life after surgical removal of the bladder—an application of graphical Markov models for analysing longitudinal dataStat Med232004649666
- B.BjerreC.JohansenK.StevenHealth-related quality of life after urinary diversion: continent diversion with the Kock pouch compared with ileal conduit: a questionnaire studyScand J Urol Nephrol Suppl1571994113118
- C.CastagnolaJ.M.MaréchalM.T.HanauerM.DawahraJ.M.DubernardQuality of life and skin urinary diversions: results of a questionnaire completed by 73 patients [in French]Prog Urol61996207216
- E.W.GerharzK.WeingärtnerT.DopatkaU.N.KöhlH.D.BaslerH.N.RiedmillerQuality of life after cystectomy and urinary diversion: results of a retrospective interdisciplinary studyJ Urol1581997778785
- Y.OkadaK.OishiY.ShichiriY.KakehiA.HamaguchiT.Tomoyoshiet alQuality of life survey of urinary diversion patients: comparison of continent urinary diversion versus ileal conduitInt J Urol419972631
- D.FilipasU.T.EgleC.BüdenbenderM.FischJ.FichtnerS.O.Hoffmannet alQuality of life and health in patients with urinary diversion: a comparison of incontinent versus continent urinary diversionEur Urol3219972329
- S.MadersbacherJ.SchmidtJ.M.EberleH.C.ThoenyF.BurkhardW.Hochreiteret alLong-term outcome of ileal conduit diversionJ Urol1692003985990
- I.IborraJ.L.CasanovaE.SolsonaTolerance of external urinary diversion (Bricker) followed for more than 10 yearsEur Urol39Suppl. 52001146147
- W.R.PittsJrE.C.MueckeA 20-year experience with ileal conduits: the fate of the kidneysJ Urol1221979154157
- J.D.SchmidtC.E.HawtreyR.H.FlocksD.A.CulpComplications, results and problems of ileal conduit diversionsJ Urol1091973210216
- A.KristjanssonL.WallinW.ManssonRenal function up to 16 years after conduit (refluxing or anti-reflux anastomosis) or continent urinary diversion. 1. Glomerular filtration rate and patency of uretero-intestinal anastomosisBr J Urol761995539545
- S.AkerlundK.DelinN.G.KockG.LyckeB.M.PhilipsonR.VolkmannRenal function and upper urinary tract configuration following urinary diversion to a continent ileal reservoir (Kock pouch): a prospective 5 to 11-year followup after reservoir constructionJ Urol1421989964968
- H.C.ThoenyM.J.SonnenscheinS.MadersbacherP.VockU.E.StuderIs ileal orthotopic bladder substitution with an afferent tubular segment detrimental to the upper urinary tract in the long term?J Urol168200220302034
- T.M.TurkF.C.KoleskiD.M.AlbalaIncidence of urolithiasis in cystectomy patients after intestinal conduit or continent urinary diversionWorld J Urol171999305307
- J.PfitzenmaierJ.LotzA.FaldumM.BeringerR.SteinJ.W.ThüroffMetabolic evaluation of 94 patients 5 to 16 years after ileocecal pouch (Mainz pouch 1) continent urinary diversionJ Urol170200318841887
- Y.S.KimN.SpritzM.BlumJ.TerzP.SherlockThe role of altered bile acid metabolism in steatorrhoea of experimental blind loopJ Clin Invest451966956962
- H.J.CanosG.A.HoggJ.R.JefferyOxalate nephropathy due to gastrointestinal disordersCan Med Assoc J1241981729733
- R.D.MillsU.E.StuderMetabolic consequences of continent urinary diversionJ Urol161199910571066
- J.L.LockhartJ.M.Pow-SangL.PerskyP.KahnM.HelalE.SanfordA continent colonic urinary reservoir: the Florida pouchJ Urol1441990864867