Abstract
Background
The present study evaluated the efficacy and safety of single injection technique for peribulbar block using a short needle and a small volume as adjuvant to general anesthesia in children undergoing ophthalmic surgery. The aim was to reduce complications accompanying general anesthesia and to improve postoperative outcome.
Method
Forty children aged 6–12 years, ASA I or II scheduled for ophthalmic surgery were included in the study. Children were randomly allocated into two equal groups (n = 20) to receive either general anesthesia alone (GA group) or single injection peribulbar block in conjunction with general anesthesia (GA-PB group). Peribulbar block was performed using single injection of 3–4 ml of 2% lidocaine-hyaluronidase mixture (10 IU/ml) and 0.5% bupivacaine with a ratio of (1:1), with a 28G, 12 mm needle. Intraoperative heart rate and mean arterial pressure, incidence of oculocardiac reflex (OCR) and number of patients required fentanyl were recorded. Postoperative nausea and vomiting (PONV), time to first rescue analgesic and number of patients who required rescue analgesia were reported.
Results
No patient developed OCR or required intraoperative analgesic supplements in GA-PB group compared to 11 (55%) and 5 (25%) patients, respectively, in GA group (p < 0.05 and p < 0.05 respectively). Intraoperative HR and MAP measures were significantly reduced in GA-PB group compared with GA group (p < 0.05). A significantly lower incidence of PONV was recorded in GA-BP group versus GA group (p < 0.05). The time to first rescue analgesic was significantly longer in GA group than GA-PB group (p < 0.05). The number of patients who required rescue analgesia in the first postoperative 12 h was significantly higher in GA group compared to GA-PB group. No serious complication was recorded in GA-PB group.
Conclusion
Single injection, peribulbar block using a short needle and a small volume is a safe and effective technique when combined with general anesthesia in pediatric ophthalmic surgery.
1 Introduction
Ophthalmic surgery is a common procedure in children where general anesthesia is the standard technique [Citation1]. Still yet, oculocardiac reflex (OCR), postoperative nausea and vomiting (PONV), postoperative pain and irritability are major problems in pediatric ophthalmic surgeries. Moreover, excessive crying and straining could be detrimental to intraocular pressure (IOP) and corneal sutures [Citation2,Citation3].
Regional anesthesia for ophthalmic surgeries was previously studied in conjunction with general anesthesia to overcome the above mentioned complications [Citation1,Citation4,Citation5].
Double injection Peribulbar block as an adjuvant to general anesthesia has been investigated and reported to be effective, however, this technique is administered blindly and some remarkable risks including, globe perforation and intravascular injection have been reported [Citation6]. These potential risks directed the authors to use a single rather than multiple injection techniques for peribulbar block [Citation7,Citation8].
In children, the double injection peribulbar block carry potentially more risks than in adults owing to the fact that there are important anatomical differences between the two age groups. The size of the eye relative to the bony orbit is much greater in childhood. The eye occupies almost 50% of the volume of the bony orbit at birth and 33% at 4 years, while the adult eye takes up only 22% of the orbital volume [Citation9].
The effectiveness of single injection technique was previously investigated in adults [Citation10,Citation11]. In the literature search, there was no data concerning its usage in pediatric age group.
The aim of this study was to evaluate the efficacy and safety of single injection peribulbar block with a short needle and small volume of local anesthetic in conjunction with general anesthesia in pediatric ophthalmic surgeries. The Incidence of OCR, hemodynamic stability, intraoperative analgesic requirement, PONV and postoperative analgesia were evaluated.
2 Material and methods
After obtaining institutional ethical committee’s approval, informed written parental consent was obtained for all patients. Forty ASA I or II children, aged 6–12 years, undergoing elective ophthalmic surgeries were enrolled in this randomized controlled study. The study was conducted at, Abu El-Rish hospital, Cairo university (December 2008–January 2010).
Children with endophthalmitis or inflammatory eye pathology, raised IOP, eye injury, single eye or known allergy to the study drugs were excluded from the study. Visual analog scale (VAS) was taught to the children and their parents two hours before surgery, with 0 representing no pain at all and 10 representing the worst imaginable pain.
Patients were randomly allocated according to computer-generated randomization list to one of two equal groups to receive either general anesthesia (GA) alone (GA group, n = 20) or combined general-single injection peribulbar block anesthesia (GA-PB group, n = 20).
Upon arrival to the operating room, standard monitor including; electrocardiogram (ECG), non-invasive blood pressure and pulse oximeter were attached to the patients. A standard BIS® monitor strip (BISX®, Aspect medical System, Norwood, MA, USA) was placed on the forehead. A bispectral index of 40–50% was considered the target range for surgical anesthesia.
After insertion of 24–22 G IV catheter, in all patients general anesthesia (GA) was induced with propofol 2–3 mg/kg and fentanyl 1 μg/kg. An appropriate size laryngeal mask airway (LMA) was inserted after achieving BIS value less than 50%. Anesthesia was maintained using 100% oxygen and sevoflurane with spontaneous respiration and capnogram was attached to obtain continuous measurement of end-tidal carbon dioxide (ETCO2). Sevoflurane concentration was titrated on the basis of BIS changes to achieve a target value between 40 and 50. End-tidal sevoflurane concentration was recorded every 5 min intraoperatively.
After confirmation of the eye to be operated, patients assigned to GA-PB group were subjected to peribulbar block as described.
2.1 Peribulbar block technique
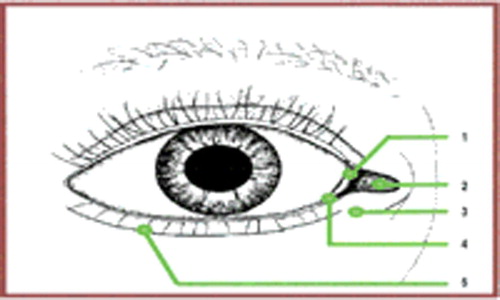
A single injection technique with 3–4 ml of 2% lidocaine-hyaluronidase mixture (10 IU/ml) and 0.5% bupivacaine with a ratio of (1:1) was performed using a 28 G, 12 mm beveled short needle. The injection site was limited superiorly with the inferior lacrimal canaliculus, medially with lateral margin of the nose, an imaginary perpendicular line that join inferior lacrimal papilla to inferior margin of the orbit laterally and inferior orbital margin inferiorly (). The needle was advanced slowly in the antero-posterior direction for half of its length and then obliquely in the direction of the optical foramen until the needle was on the same plane of the bony margin of the orbit [Citation12]. After negative aspiration, the local anesthetic mixture was slowly injected. Digital ocular compression was performed for 5 min.
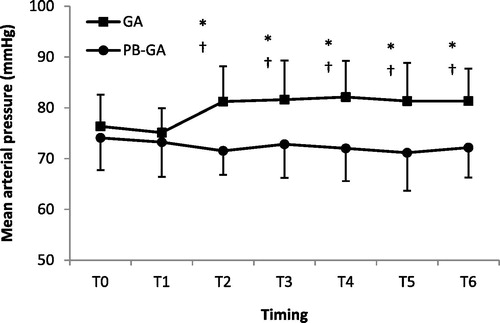
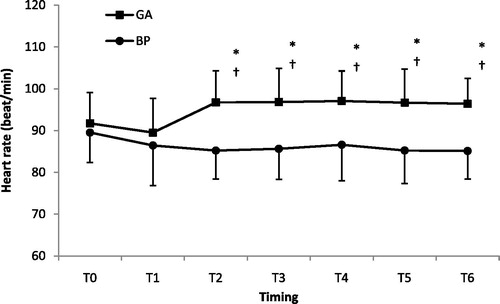
Intraoperative mean arterial blood pressure (MAP) and heart rate (HR) were recorded before induction (T0), immediately after induction (T1), at incision (T2), and every 15 min till the end of the procedure (T3–T6). An increase in HR or MAP by more than 20% above the baseline despite a BIS value within the target range (40–50) was assumed to be due to insufficient analgesia and 0.5 μg/kg i.v. fentanyl was given. Intraoperative fentanyl supplements were recorded in both groups.
After several trial cases done before the study, the optimum duration to perform the block was calculated to be 3–4 min after induction. Intra-ocular pressure (IOP) was measured pre-induction (baseline) (IOP1), immediately after induction of GA (IOP2). Then at 5 and 10 min later in GA group (IOP3, 4) or immediately after peribulbar block and 5 min ocular compression in GA-PB group (IOP3, 4).
Occurrence of any arrhythmia or oculocardiac reflex, which was defined as a rapid reduction in heart rate >20% of baseline was recorded. It was treated by asking the surgeon to stop stimulation and if this was not effective, intravenous atropine 0.01 mg/kg was given. The need for atropine medication was also recorded.
At conclusion of surgery, sevoflurane was discontinued and the LMA was removed. Patients transferred to the post anesthesia care unit (PACU) where they were observed for one hour then discharged to the ward to be observed for 12 h postoperatively. Postoperative recovery was evaluated using a modified Aldrete Score [Citation13] every 5 min, Time to achieve full scoring ⩾9 was recorded. Postoperative pain was assessed at 30 min, 1, 3, 6 h and 12 h using visual analog score (VAS). 1 mg/kg diclofenac suppository was given if VAS > 3. The time interval from PACU admission to the first rescue analgesic and requirements of rescue analgesia were recorded.
Incidence of postoperative nausea and vomiting was assessed for 12 h postoperatively, patients who had persistent nausea or more than one vomiting episode in one hour received ondansetron 0.15 mg/kg. Number of patients who required antiemetic therapy was recorded. The occurrence of complications related to the peribulbar block (chemosis, subconjunctival hemorrhage or perforation) was documented as well as any difficulty recorded during surgery could be attributed to the block.
3 Statistical analysis
Assuming that a difference of 30% or more in the time to first analgesic dose would be of clinical interest, a sample size of 20 patients per group was calculated to achieve a power of 80% and a significance level of 0.05.
Statistical analysis was performed using SPSSwin statistical package version 15 (SPSS Inc., Chicago, IL). Data were presented as mean ± SD or number (%) as appropriate. Comparison between the two groups was performed using unpaired student’s t-test. Intragroup comparison relative to baseline was performed using repeated measure analysis (ANOVA) with post hoc Dunnet’s test if ANOVA results were significant. Nominal variables were compared using Fisher’s exact test. A p-value < 0.05 was considered significant
4 Results
Patients in both groups were comparable with respect to age, sex, weight, ASA physical status, duration and type of surgery ().
Table 1 Demographic and operative data. Values are expressed as mean ± SD or ratio.
In GA-PB group no patient experienced OCR compared to 11 (55%) children in GA group (p < 0.05). Five Out of them required atropine medication.
No patients required intraoperative supplementary fentanyl in GA-PB group compared to five patients (25%) in GA group, all of them needed one bolus only (p < 0.05).
Mean End tidal sevoflurane concentration was comparable in both groups (2.4 ± 0.39 vs 2.6 ± 0.41).
MAP and HR values were comparable in both groups at T0 and T1. Values at (T2–T6) were significantly higher in GA group compared to its baseline value and to GA-PB group (p < 0.05) ( and ).
IOP values were comparable in the two groups at IOP1 (baseline) and IOP2. Compared to baseline, there was a significant increase in IOP in GA-PB group immediately after the injection of local anesthetic (IOP3) (p < 0.05) and returned to its baseline value after 5 min of compression (IOP4). In GA group there were no changes in IOP at all measurement points ().
Table 2 Intraoccular pressure measurements (mmHg) of both groups (mean ± SD).
In PACU, time to achieve full Aldrete score was comparable in both groups (12.1 ± 2.6 min in GA-PB group vs 14.6 ± 3.1 min in GA group).
Incidence of PONV over 12 h and number of children who required antiemetic treatment were significantly reduced in GA-PB group compared to GA group [1 (5%) and 0 (0%) vs 7 (35%) and 3 (43%) respectively] (p < 0.05).
In the postoperative period (12 h), a significantly lower number of children in GA-PB group required analgesic rescue compared with those in GA group. The time to first rescue analgesic was significantly prolonged in GA-PB group compared to GA group (p < 0.05). The frequency of rescue analgesia required was less in GA-PB group compared with GA group (p > 0.05) ().
Table 3 Postoperative analgesia of both groups [n (%) or mean ± SD].
The performance of peribulbar block was not associated with any serious complications. Only four patients manifested with self limiting subconjunctival hemorrhage in GA-PB group which resolved without treatment.
5 Discussion
The present study demonstrated that single injection, peribulbar block reduced the incidence of OCR, intraoperative fentanyl requirement and PONV, in addition it prolonged the time to first rescue analgesic when combined with general anesthesia in pediatric ophthalmic surgery.
In previous studies [Citation1,Citation14], authors used 16 mm long needles in double injection peribulbar block in pediatrics. The single injection technique used in the current study was performed using a shorter needle of 12 mm length, 28 G to reduce the complications associated with longer needles as hemorrhage or globe perforation [Citation6]. However, there was a higher incidence of subconjunctival hemorrhage in the PB group related to the needle length used, explained by restriction of bleeding to the anterior orbit [Citation12]. Moreover, using a single injection in the current study was not associated with the complications reported with the double injection technique which included rare but ultimately serious complications, such as vascular injuries or incidence of misdirection [Citation6]. The puncture site and the needle direction in our work were in a relatively avascular area and with less incidence to misdirection.
Previous researches that investigated double injection peribulbar block in pediatrics used volumes up to 10 ml of local anesthetic mixture [Citation1,Citation3]. Owing to the fact that the mechanism of increased IOP is related to the mechanical pressure effect from the volume injected [Citation15], particularly in pediatrics with special anatomical configuration, a smaller volume (3–4 ml) was used in this study. This smaller volume was associated with transient IOP increase with no operative effect.
OCR is a trigeminal vagal reflex caused by traction of extraocular muscles, pressure on the orbit, trauma and orbital hematoma [Citation16].
Different methods have been used to prevent OCR, such as premedication with anticholinergics and adequate anesthetic depth [Citation17]. Premedication using atropine has been used to prevent OCR, especially in infant and young children as they tend to have higher resting vagal tone. However, it was not found to be totally effective moreover, it may cause tachycardia and variety of cardiac arrhythmias. These effects may stay longer than the reflex itself, as it is a self-limiting reflex. This finding discouraged many authors to use atropine routinely [Citation14,Citation17,Citation18].
In the present work single injection peribulbar block significantly reduced the incidence of OCR in GA-BP group compared to the GA group. This finding could be attributed to blocking the afferent limb of OCR and reduced the afferent stimuli from muscle traction [Citation19,Citation20].
In accordance with our results, Deb et al. [Citation1] reported that 4% of children in peribulbar block group experienced OCR compared to 60% in GA group when they studied the efficacy of double injection technique for peribulbar block as adjuvant to GA in ophthalmic surgery.
Another study done by Gupta et al. [Citation14] reported lower incidence of OCR in children undergoing strabismus surgery when using double injection peribulbar block in conjunction with GA (13% in BP group vs 94% in GA group). The higher incidence in GA group reported in the latter study compared to our study may be due to younger age group (2–13 years) as children tend to have higher resting vagal tone [Citation21]. Moreover, all patients were undergoing strabismus surgery which is known to have a higher incidence of OCR [Citation22].
In the current work, single injection peribulbar block provided adequate intraoperative analgesia as evident by reduction in intraoperative fentanyl requirement and hemodynamic stability in GA-BP group). These results coincided with the results of the previous works which investigated the intraoperative analgesic effect of regional blocks in ophthalmic surgery [Citation1,Citation3,Citation23].
PONV is a common problem following ophthalmic surgery [Citation24]. Repeated vomiting can affect the integrity of corneal suture, increase the cost of antiemetic drugs and prolonged the postoperative stay [Citation25]. PONV is mediated by the oculo-emetic pathway which shares the afferent limb of the reflex arc with OCR [Citation26].
Inspite of the fact that per bulbar block is used safely in children, it’s less used in strabismus surgery as it produces hypotonic eye. Still yet, this finding was weighted against its advantages including the satisfactory analgesia and akinesia, thus reducing the incidence of PONV by allowing time for the child to adapt to visual changes postoperatively [Citation27].
In the present work, using single injection peribulbar block as adjuvant to GA reduced the incidence of PONV; this is in line with the results reported by Gupta et al. [Citation14] and Deb et al. [Citation1] who found that double injection peribulbar block effectively reduced the incidence of PONV in children undergoing ophthalmic surgery under GA. Similar results were reported in adults undergoing vitreoretinal surgery, where single injection peribulbar block was used in conjunction with GA [Citation10].
Subramaniam and his colleagues [Citation3] also reported that the incidence of PONV was 81.39% in group GA vs 54.76% in patient received double injection peribulbar block and explained this high incidence in both groups by the long duration of vitreoretinal surgery and waned effect of the block.
In contradiction to our finding, Chhabra et al. [Citation27] and Moral et al. [Citation28], could not detect a significant difference in PONV when compared peribulbar block as adjuvant to GA and GA alone in ophthalmic surgery. This may be due to the antiemetic effect of propofol [Citation29] as they used total intravenous anesthesia (TIVA) as an anesthetic technique.
The effectiveness of double injection peribulbar block in reducing postoperative pain in ophthalmic surgery was previously reported [Citation3,Citation30].
In this study, single injection peribulbar block effectively reduced postoperative pain as the time to first rescue analgesic was significantly longer and number of pain free patients were significantly higher in GA-BP group than in GA group. This finding is in accordance with results reported by Ghali and Btarny in 2010 [Citation10], when they studied the effect of single injection peribulbar block in adults undergoing vitreoretinal. Also Subramaniam et al. [Citation3] reported similar results when using double injection peribulbar block in pediatrics.
In contrast when Shende et al. [Citation19] investigated the usage of peribulbar block as adjuvant to general anesthesia during retinal detachment surgery, they found out that time to first rescue analgesic was comparable in peribulbar and GA groups. This could be explained by the use of lower concentration of bupivacaine (0.25%) in the peribulbar block group and morphine in GA group as stated by Ghali and Btarny [Citation10].
6 Conclusion
Single injection peribulbar anesthesia using a short needle and small volume is an effective technique as an alternative approach for regional anesthesia in pediatric ophthalmic surgery. It provided low incidence of OCR, less intraoperative opioid requirements, stable intraoperative hemodynamics, less PONV and improved postoperative analgesia. It has the advantage of being simple and safe, decreased volume of local anesthetic used, and single puncture with short needle which provides less incidence of vascular trauma and misdirection.
Notes
Available online 26 March 2011
References
- K.DebR.SubramaniamM.DehranSafety and efficacy of peribulbar block as adjuvant to general anaesthesia for paediatric ophthalmic surgeryPaediatric Anaesthesia112001161167
- G.B.SmithR.C.HamiltonC.A.CarrOphthalmic Anesthesia2nd ed.1996Oxford University PressLondonp.189–224
- R.SubramaniamS.SubbarayuduV.RewariUsefulness of pre-emptive peribulbar block in pediatric viteroretinal surgery: a prospective studyRegional Anesthesia and Pain Medicine2820034347
- Y.AtesN.UnalH.CuhrukN.ErkanPostoperative analgesia in children using preemptive retrobulbar block and local anesthetic infiltration in strabismus surgeryReg Anesth Pain Med231998569740
- B.GhaliJ.RamJ.K.MakkarSubtenon block compared to intravenous fentanyl for perioperative analgesia in pediatric cataract surgery1084200911321138
- M.V.ParulekarS.BergJ.S.ELstonAdjunctive peribulbar anesthesia for paediatric ophthalmic surgery: are the risks justified?Paediatr Anaesth1220028586
- J.RipartJ.Y.LefrantJ.I.L’HermiteCaruncle single injection episcleral (sub-tenon) anesthesia for cataract surgery: mepivacaine versus a lidocaine-bupivacaine mixtureAnesth Analg912000107109
- J.RipartJ.Y.LefrantB.VivienOphthalmic regional anesthesia: medial canthus episcleral (sub-tenon) anesthesia is more efficient than peribulbar anesthesia: a double-blind randomized studyAnethesiology92200012781285
- S.Duke-ElderSystem of Ophthalmologyvol. 31963Henry KimptonLondonp.310–2
- A.M.GhaliA.M.El btarnyThe effect on outcome of peribulbar anaesthesia in conjunction with general anesthesia for vitreoretinal surgeryAnaesthesia652010249253
- A.M.GhaliA.HafezSingle-injection percutaneous peribulbar anaesthesia with a short needle as an alternative to the double-injection technique for cataract extractionAnesth Analg11012010245247
- L.RizzoM.MariniC.RosatiPeribulbar anesthesia: a percutaneous single injection technique with a small volume of anestheticAnesth Analg10020059496
- J.A.AldreteThe post-anesthesia recovery score revisitedJ. Clin Anesth7199589
- N.GuptaR.KumarS.KumarProspective randomized double blind study to evaluate the effect of peribulbar block or topical application of local anaesthesia combined with general anaesthesia on intra-operative and postoperative complication during pediatric strabismus surgeryAnaesthesia62200711101113
- B.AzmonY.AlsterM.LazerO.GeyerEffectiveness of sub-Tenon’s versus peribulbar anesthesia in extracapsular cataract surgeryJ Cataract Refract Surg25199916461650
- S.LangD.LanignM.Van der WalTrigeminocardiac reflexes: maxillary and mandibular variants of oculocardiac reflexCanad J Anaesthesia381991757760
- R.K.MirakhurC.J.JonesJ.W.DundeeD.B.ArcherIntramuscular or intravenous atropine or glycopyrolate for prevention of OCR in children during squint surgeryBr J Anesthesia5419821059
- R.DellB.WilliamsAnaesthesia for strabismus surgery a regional surveyBr J Anaesthesia821999761763
- D.ShendeS.SadhasivamR.MadanEffect of peribulbar bupivacaine as an adjuvant to general anesthesia on post-operative outcome following retinal detachment surgeryAnesthesia552000970975
- U.RutaT.MollhoffH.MarkodimitrakisG.BrodnerAttenuation of the oculocardiac reflex after topically applied lidocaine during surgery for strabismus in childrenEur J Anesthesiol1319961115
- V.F.BlancJ.F.HardyJ.MiltonJ.L.JacobThe occulocardiac reflex: a statistical analysis in infants and childrenCanad Anaesthestists’ Soc J301992360369
- V.K.MisuryaS.P.SingV.K.KulshresthaPrevention of oculocardiac reflex during extraocular muscle surgeryInd J Ophthalmol3819908587
- A.ChhabraR.SinhaR.SubramaniamComparison of sub-Tenon’s block with i.v. fentanyl for paediatric vitreoretinal surgeryBr J Anesthesia10352009739743
- S.SadhasivamD.ShendeR.MadanProphylactic ondansetron in prevention of postoperative nausea and vomiting following pediatric strabismus surgery: a dose response studyAnesthesiology92200010351042
- M.F.WatchaThe cost/effective management of postoperative nausea and vomitingAnesthesiology922000931933
- A.A.Van den BergA.LambourneP.A.ClyburnThe oculoemetic reflex: a rationalization of postophthamic anaesthesia vomitingAnaesthesia441989110117
- A.ChhabraR.PandeyM.KhandelwalAnesthetic techniques and postoperative emesis in pediatric strabismus surgeryReg Anesthesia Pain Med30120054347
- J.MorelJ.PascalD.CharierPreoperative peribulbar block in patients undergoing retinal detachment surgery under general anesthesia: a randomized double-blind studyAnesthesia Analgesia102200610821087
- T.StandlS.WilhelmG.Von KnobelsdorffPropofol reduces emesis after sufentanil supplemented anaesthesia in pediatric squint surgeryActa Anaesth Scand401996729733
- N.KristinC.L.SchonfeldM.BechmannVitreoretinal surgery: pre-emptive analgesiaBr J Ophthamol85200113281331