Abstract
Background
Elderly patients undergoing transurethral resection of the prostate (TURP) may have preexisting cardiac or cerebral dysfunction. Maintaining hemodynamic stability is essential. The objective of this study was to compare the anesthetic efficacy and cardiovascular stability of a subarachnoid injection of 7.5 mg hyperbaric bupivacaine at the level of T12–L1 to 15 mg hyperbaric bupivacaine injected at the level of L3–4 for elderly patients undergoing TURP.
Methods
Fifty patients undergoing TURP were enrolled. Patients were randomized to either of two groups: Group I: Dural puncture was performed in the midline at the T12–L1 interspace. 7.5 mg of hyperbaric bupivacaine (1.5 ml of 0.5% solution) was then injected through a 16 gauge/26 gauge combined spinal–epidural by “needle through needle” technique. Group II: Dural puncture was performed in the midline at the L3–4 interspace. Fifteen milligrams of hyperbaric bupivacaine (3 ml of 0.5% solution) was then injected through a 25-gauge spinal needle. Demographic data, prostate size, volume of irrigation fluids, hemodynamic parameters, block characteristics, and complications were recorded.
Results
Demographic data, prostate size, volume of irrigating fluids, complications and duration of surgery were comparable in both groups.
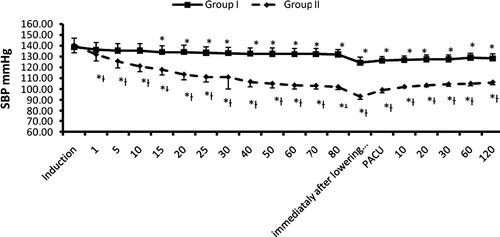
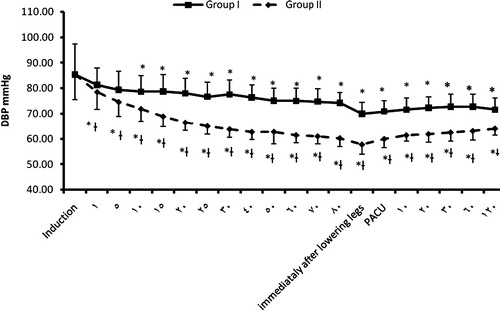
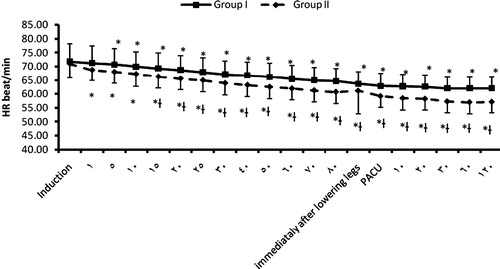
Patients in Group I exhibited a more stable blood pressure and heart rate during the study time period (P < 0.05).
The duration of sensory and motor blockade were shorter in Group I (P < 0.05).
Patients in Group II demonstrated a significantly higher peak sensory block (T4, P < 0.05), shorter mean time to peak sensory block (4.8 ± 1.1 min, P < 0.05), and earlier onset of sensory block at T10 (2.6 ± 0.5 min, P < 0.05).
Conclusion
Injection of 7.5 mg hyperbaric bupivacaine at the level of T12–L1 is sufficient to provide adequate sensory block while maintaining hemodynamic stability for TURP. This dose and injection location may offer an additional advantage of decreased duration of motor block in patients undergoing TURP.
1 Introduction
Benign hypertrophy of the prostate is a common disorder affecting 2.7% of males at the age of 45–49 years and up to 24% at 80 years [Citation1]. Anesthesia for elderly patients should consider the physiological changes that might affect organ function. Elderly people may have increased vasomotor tone. In addition, their myocardial Beta receptor response is blunted in comparison to younger patients. As a result, when subjected to decreased sympathetic tone, there will be a limited reflex increase in heart rate and myocardial contractility [Citation2]. Spinal anesthesia, in comparison to general anesthesia, is usually preferred for elderly patients for TURP due to its relatively limited effect on myocardial performance, blood pressure, and cardiac output [Citation3].
To ensure adequate sensory and motor block for TURP, spinal anesthesia should extend to at least the 10th thoracic dermatome. In order to reduce the side effects of the standard dose of hyperbaric bupivacaine, many authors suggest the addition of opioids to reduce the total mg dose. Wang et al. [Citation4] compared low dose bupivacaine and fentanyl with low dose bupivacaine and sufentanil to the standard dose of bupvicaine for TURP patients. They found that low dose bupivacaine and sufentanil maintained hemodynamics better than bupivacaine and fentanyl.
In a similar study, Kim et al. [Citation5] compared low dose bupivacaine and fentanyl to low dose bupivacaine and sufentanil. They found that both provided adequate anesthesia with stable hemodynamics.
It should be noted that respiratory depression is a known complication of intrathecal opioids. Although the use of a lipophilic opioid has less delayed respiratory depression than with a hydrophilic opioid like morphine, it has been demonstrated that early respiratory (depression within 15–30 min) can still occur with intrathecal fentanyl and sufentanil. This may limit the usefulness of using intrathecal opiods in the elderly population [Citation6,Citation7].
To the best of our knowledge there are no studies comparing the effect of low dose hyperbaric bupivacaine injected at a thoracic level with the standard dose at lumbar spinal levels for TURP in elderly patients.
The objective of this study was to evaluate the effect of injecting low dose hyperbaric bupivacaine at T12–L1 on hemodynamic stability and efficacy of sensory and motor blockade, compared to the standard dose of hyperbaric bupivacaine injected at a standard lumber spinal level for elderly patients undergoing TURP.
2 Methods
After approval of the local Ethics Committee and obtaining written informed consent, 50 ASA physical status I–II patients, aged 70–80 year old receiving spinal anesthesia for elective TURP were enrolled in this study.
Exclusion criteria included a history of allergy to local anesthetics, diabetes mellitus, psychiatric or neurologic diseases, morbid obesity (body mass index >40), coagulation disorders, infection at the site of injection, and patient’s refusal of regional anesthesia as the sole anesthetic technique.
Standard monitoring was used throughout the study including non-invasive blood pressure, ECG, and pulse oximetry. Baseline values of systolic and diastolic blood pressure and heart rate were recorded before induction of anesthesia.
An 18-gauge peripheral IV was placed. Patients were premedicated with 0.5–1 mg of midazolam IV 15 min before the spinal block. Normal saline (100 cc) was administered IV over 20 min before the procedure.
Patients were randomly assigned to one of two groups using a list of random numbers. All spinal injections were performed in the sitting position. All injections were performed by one of the investigators who was not involved in any subsequent assessment or data collection.
Group I patients (low dose bupivacaine, thoracolumbar puncture n = 25): The dural puncture was performed in the midline at the level of the T12–L1 interspace using a combined spinal epidural technique by “needle through needle” (16 gauge/26 gauge combined spinal–epidural, Braun, Pencan, Bethlehem, PA). After local infiltration with 3 cc of lidocaine (2%), the epidural space was identified with a loss of resistance technique with saline with a 16 g tuohy needle. A 26 g pencil point needle was then advanced through the tuohy needle until the dura was punctured. After appearance of CSF, 7.5 mg of 0.5% (1.5 ml) hyperbaric bupivacaine (Astra Zeneca AB, Sodertalji, Sweden) was injected. The tip of the spinal needle was not allowed to protrude more than 1.5 cm beyond the tip of the tuohy needle.
Group II patients (high dose bupivacaine, lumbar puncture, n = 25): The dural puncture was performed in the midline at the L3–4 interspace using a 25-gauge spinal needle (Unisis Corp., Tokyo, Japan). After free CSF flow was observed, 15 mg of 0.5% (3 ml) hyperbaric bupivacaine was injected.
All injections were done over a period of 5 s with cephalad orientation of the spinal needle side hole. Patients were returned to the supine position immediately after completion of the block and the patient’s legs were then placed in the lithotomy position. All patients received 25 mg of meperidine and 4 mg ondansetron intravenously immediately after injection.
Hemodynamic data, including systolic and diastolic blood pressure and heart rate, were recorded every 5 min for 30 min and then every 10 min until the end of surgery. The attending anesthesiologist was blinded to the group assignment and to the dose and location of injection of the local anesthetic. Hemodynamic data were also measured immediately after lowering the legs at the completion of the procedure. In the PACU, vital signs were recorded every 10 min for the first 30 min, then every 1 h for 2 h. All patients in this study were admitted to the PACU for 2 h. Clinically relevant hypotension (decrease in systolic arterial blood pressure by 30% or more from baseline values) was treated with a bolus of 5 mg ephedrine intravenously. Bradycardia (<50 beats/min) was treated with 0.2 mg glycopyrrolate intravenously.
Assessment of sensory block included: onset of sensory block at T10, peak sensory level of blockade, and two segment regression. This was made by the same anesthesiologist who was blinded to the treatment group. Sensory level was evaluated by loss of sensation to pinprick (20-gauge hypodermic needle). Assessment of the first two sensory parameters were made at the following times: 1, 5, 10, 30 min after the injection, whereas two segment regression was assessed at: 45, 60, 90, and 120 min after injection.
Assessment of motor blockade (Bromage Score [Citation8]) was made at the following times: 5 and 120 min after injection.
Intraoperative side effects or complications, including shivering, nausea, vomiting, TURP Syndrome, and bleeding were treated and documented if they occurred.
3 Statistical analysis
A power analysis was performed using Student’s t-test for independent samples on mean decrease of systolic blood pressure because it was the main outcome variable in the present study. A previous study found that when a standard dose of bupivacaine is used for spinal anesthesia, the mean decrease in systolic blood pressure was 40 mmHg with SD 20 [Citation9] Based on the assumption that detecting a difference of 20 mmHg in the mean decrease in SBP is considered a clinically significant difference between groups, and taking a power of 0.9 and alpha error of 0.05, a minimum sample size of 23 patients was calculated to be needed for each group. A total of 25 patients in each group were included to compensate for possible dropouts.
Categorical variables were assessed using chi-square or Fischer exact test where appropriate. Normally distributed data are presented as mean (SD), and were analyzed using Student’s t test and two-way analyses of variance with repeated measures and post hoc Dunnett test as appropriate. Data not normally distributed (tested by Kolmogorov–Smirnov test) are presented as median (range) and were analyzed with Mann–Whitney U test or the Kruskal–Wallis test as appropriate. The software SPSS v15.0 for Windows (SPSS, Inc., Chicago, Il, United States) was used for statistical analysis.
4 Results
All 50 enrolled patients completed the study. Demographic data were comparable in the two groups ().
Table 1 Demographic data. Data are presented as mean ± SD.
Both study groups were comparable regarding operative time, volume of glycine 1.5% in water, and the prostate size (). All study results are summarized in : Group II demonstrated a significantly faster onset of sensory block at the T10 dermatomal level (2.6 ± 0.5 min) compared to Group I (5.8 ± 1.3 min, P < 0.0001).
Table 2 Study data. Data are median (interquartile range [range]), mean (SD), or ratio.
The median peak sensory block level was significantly higher in Group II than that in Group I, P < 0.0001. Whereas the mean time to reach peak level was significantly lower in Group II (4.8 ± 1.1 min) compared to Group I (14.5 ± 1.4 min), (P < 0.0001). Block regression was significantly slower with the use of high dose bupivacaine, as the two segment regression of sensory blockade occurred within 2 h of injection in all of the 25 patients in the Group I compared to none in the Group II, P < 0.0001).
The onset time of motor block and the maximum motor block were comparable between the two groups. Bromage score after 5 min was comparable between the two groups. However, the number of patients with complete motor block (Bromage score of 4) after 2 h was significantly lower in Group I compared to Group II P < 0.0001, Table 2.
Administration of low dose bupivacaine resulted in a significant decrease in HR and blood pressure in Group I relative to baseline, starting 5 and 15 min, respectively after the administration of the drug, and continuing to the end of the study period. In the Group II, HR and blood pressure decreased significantly relative to baseline, starting immediately after injection of the study drug and continued throughout the study protocol. Patients in the Group II had significantly lower HR and blood pressure relative to those in Group I starting 15 and 1 min after the administration of the drug and lasting for the rest of the study period, P < 0.05 ().
Although both groups demonstrated a decline in blood pressure, none of the patients had a greater than 30% decrease from baseline requiring treatment.
There were no intraoperative instances of shivering, nausea, vomiting, TURP Syndrome, or bleeding in the two study groups.
5 Discussion
Our results demonstrated that low dose (7.5 mg) hyperbaric bupivacaine administered at the T12–L1 level in elderly patients undergoing TURP, maintained hemodynamic while providing adequate sensory and motor blockade. It also allowed a faster recovery when compared to the standard 15 mg dose administered at the L3–L4 level.
The autonomic nerve supply to the prostate has three limbs, sympathetic, parasympathetic and peptidergic. The sympathetic limb originates from T10–L2 whereas the parasympathetic limb arises from S2–4 [Citation10,Citation11]. The sensory level of blockade required for TURP should be the 10th thoracic spinal level. Of interest, the study by Ozmen et al. found that a saddle block, with 10 mg hyperbaric bupiacaine and 50 mcg fentanyl, provided adequate anesthesia for TURP patients [Citation12].
In our study, Group II demonstrated a faster onset of sensory block at the T10 dermatomal level than Group I. These findings are consistent with other studies [Citation13–Citation15]. Baricity is one of the most important factors affecting the spread of local anesthetic solutions. Other factors affecting the spread of local anesthetic include: patient’s position during and immediately after injection, total dose of local anesthetic, and level of injection. In this study, both groups received hyperbaric bupivacaine in the same position. The doses of bupivacaine, and the level of injection, therefore, are the only two variables that could contribute to the difference seen in sensory blockade between the two groups.
The mean age of patients in our study was 75 years. The use of low dose bupiacaine (7.5 mg) in this age group of patients was found to minimize the cephalad spread of hyperbaric bupivacaine (as shown by hemodynamic response) when injected at T12–L1 in Group I. A more cephalad spread was encountered with 15 mg bupivacaine injected at L3–L4 in Group II. This could be explained by the increase in thoracic kyphosis with advancing age that could limit the cephalad spread of local anesthetics injected at thoracic levels [Citation16,Citation17]. Our findings highlight the effect of the dose of local anesthetic on subarachnoid spread.
The use of opioids as an adjuvant to spinal anesthesia has been studied by multiple authors [Citation18–Citation22]. Although some studies have found opioids can prolong the duration of postoperative analgesia [Citation18–Citation21] others have shown no effect [Citation22]. Moreover the use of opioids may be associated with systemic effect such as sedation, nausea and vomiting. We did not add opioids to the local anesthetics in this study. The decision reflects our current practice and also to eliminate confounding variables.
In the current study, the use of low dose bupivacaine not only provided adequate spinal blockade but also more rapid motor recovery. The clinical significance of the shorter duration of motor blockade in Group I would be earlier ambulation and discharge from the PACU.
One of the most common complications of regional anesthesia is hypotension. This is directly related to decrease in the systemic vascular resistance seen with the sympathetic blockade. It is important to note, however that cardiac output is maintained with the decrease in the SVR [Citation23].
Our study demonstrated no deleterious effects on hemodynamics, with the use of low dose bupivacaine injected intrathecally at T12–L1. It was not surprising to observe this hemodynamic stability in the low dose bupivacaine group in view of its less extensive spread. It is likely that any sympathetic blockade was more restricted and of slower onset, resulting in less hemodynamic change.
Casati et al. [Citation24] demonstrated that minimizing hypotension with spinal anesthesia was possible by injecting a low dose of bupivacaine while keeping patients in the lateral position after injection. In our study, there was no incidence of hypotension in the supine position after injection.
To avoid injury of the conus medullaris with an intrathecal injection, Reynolds states that anesthesiologists should not perform a spinal puncture cephalad to the L3–4 interspace [Citation25].
Van Zendert et al. [Citation26] published a case report of thoracic spinal anesthesia performed safely with no instance of cord damage. Other studies [Citation27] have reported the safe use of spinal anesthesia for laparoscopic cholecystectomy.
To minimize the chance of spinal cord injury, a combined spinal epidural technique was chosen to precisely locate the epidural space and aid in limiting the depth of insertion of the spinal needle. In this study we did not have any complications of this technique.
We did not observe shivering or emesis in this study. We attribute this to the pre-emptive use of meperidine 25 mg IV and ondansetron 4 mg for all patients after induction of subarachnoid block. This is consistent with the finding of Kelska et al. [Citation28].
In conclusion, 7.5 mg hyperbaric bupivacaine injected at T12–L1 is sufficient to provide adequate sensory block, while maintaining hemodynamic stability during TURP procedures. This technique may offer the additional advantage of decreased duration of motor block in patients undergoing TURP.
6 Conflict of interest statement
No conflicts of interest.
Notes
Available online 5 May 2011
References
- K.M.VerhammeJ.P.DielemanG.S.BleuminkJ.van der LeiM.C.SturkenboomW.ArtibaniTriumph Pan European Expert Panel. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care – the Triumph projectEur Urol422002323328
- R.C.VeithJ.A.FeatherstoneO.A.LinaresJ.B.HalterAge differences in plasma norepinephrine kinetics in humansJ Gerontol411986319324
- J.P.MarkS.M.SteeleCardiovascular effects of spinal anesthesiaInt Anesthesiol Clin2719893139
- Y.C.WangQ.L.GuoE.WangW.Y.ZouSpinal anesthesia with low dose sufentanil-bupivacaine in transurethral resection of the prostateZhong Nan Da Xue Xue Bao Yi Xue Ban312006925928
- S.Y.KimJ.E.ChoJ.Y.HongB.N.KooJ.M.KimH.K.KilComparison of intrathecal and sufentanil in low-dose dilute bupivacaine spinal anaesthesia for transurethral prostatectomyBr J Anaesth1032009750754
- S.D.BelzarenaClinical effects of intrathecally administered fentanyl in patients undergoing cesarean sectionAnesth Analg741992653659
- C.M.PalmerEarly respiratory depression following intrathecal fentanyl-morphine combinationAnesthesiology74199111531155
- P.R.BromageEpidural analgesia1978WB SaundersPhiladelphia p 144
- J.W.MartyrM.X.ClarkHypotension in elderly patients undergoing spinal anesthesia for repair of fractured neck of femur. A comparison of two different spinal solutionsAnaesth Intensive Care292001501505
- J.D.BrooksAnatomy of the lower urinary tract and male genitaliaP.C.WalshA.B.RetikE.D.J.VaughanCampbell’s urology1998SaundersPhiladelphia
- M.KepperJ.KeastImmunohistochemical properties and spinal connections of pelvic autonomic neurons that innervate the rat prostate glandCell Tissue Res2811995533542
- S.OzmenA.KoşarS.SoyupekA.ArmağanM.B.HoşcanC.AydinThe selection of the regional anaesthesia in the transurethral resection of the prostate (TURP) operationInt Urol Nephrol352003507512
- N.M.GreeneDistribution of local anesthetic solutions within the subarachnoid spaceAnesth Analg641985715730
- W.KleinmanM.MikhailSpinal epidural and caudal blocksG.E.MorganClinical anesthesiology4th ed.2006Lange Medical BooksNew York
- D.T.WarrenS.S.LiuNeuraxial anesthesiaD.E.LongneckerAnesthesiology2008McGraw-Hill MedicalNew York
- J.P.RacleA.BenkhadraJ.Y.PoyB.GleizalSpinal analgesia with hyperbaric bupivacaine: influence of ageBr J Anaesth601988508514
- H.O’gormanG.JullThoracic kyphosis and mobility: the effect of agePhysiother Theory Pract31987154162
- Z.N.AkcaboyE.Y.AkcaboyM.BaydarN.GogusLow dose levobupicaine 05% versus bupivacaine 05% with fentanyl in spinal anesthesia for transurethral prostatectomyReg Anesth Pain Med322007S1S41
- H.K.KilJ.E.ChoS.Y.BanY.SongJ.Y.HongComparison of low-dose bupivacaine fentanyl and bupivacaine sufentanyl spinal anesthesia for TURP in elderly patientsReg Anesth Pain Med200720074347
- B.Ben-DavidG.MillerR.GavrielA.GurevitchLow-dose bupivacaine-fentanyl spinal anesthesia for cesarean deliveryReg Anesth Pain Med252000235239
- C.BoucherM.GirardP.DroletY.GrenierL.BergeronH.H.Le TruongIntrathecal fentanyl does not modify the duration of spinal procaine blockCan J Anaesth482001466469
- A.KararmazS.KayaS.TurhanogluM.A.OzyilmazLow-dose bupivacaine-fentanyl spinal anaesthesia for transurethral prostatectomyAnaesthesia582003526530
- R.L.CarpenterR.A.CaplanD.L.BrownC.StephensonR.WuIncidence and risk factors for side effects of spinal anesthesiaAnesthesiology71992906916
- A.CasatiG.FanelliG.AldegheriE.ColnaghiE.CasalettiV.CedratiFrequency of hypotension during conventional or asymmetric hyperbaric spinal blockReg Anesth Pain Med241999214219
- F.ReynoldsDamage to the conus medullaris following spinal anaesthesiaAnaesthesia562001238247
- A.A.J.Van ZundertG.StultiensJ.J.JakimowiczBeemVan den BorneW.G.J.M.Van der HamJ.A.W.WildsmithSegmental spinal anaesthesia for cholecystectomy in a patient with severe lung diseaseBr J Anaesth962006464466
- A.A.J.Van ZundertG.StultiensJ.J.JakimowiczBeemVan den BorneW.G.J.M.Van der HamJ.A.W.WildsmithLaparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: a feasibility studyBr J Anaesth982007682686
- E.KelsakaS.BarisD.KarakayaB.SarihasanComparison of ondansetron and meperidine for prevention of shivering in patients undergoing spinal anesthesiaReg Anesth Pain Med3120064045