Abstract
Background
To find out the cost effective antiemetic drug combination as a prophylaxis against nausea and vomiting during regional anesthesia for cesarean section.
Methods
After the gaining of institutional ethical approval, 240 parturients scheduled for elective cesarean delivery under spinal anesthesia were randomly allocated to receive either 2 mg granisetron plus 8 mg dexamethasone (group II) IV immediately after clamping of the fetal umbilical cord or 2 mg midazolam plus 8 mg dexamethasone (group III) IV or placebo (group I).
Results
The use of rescue antiemetic medication, which indicates either vomiting or severe nausea, in the post delivery period intraoperatively was 37%, 14%, 23% in group I, II and III, respectively. These values are significantly less than the corresponding values during the first 24 h after surgery which was 20%, 7%, 13%, respectively. No clinically serious adverse events were observed in any of the groups.
Conclusion
The prophylactic use of a granisetron/dexamethasone combination is better than midazolam/dexamethasone for reducing nausea and vomiting in patients during and after spinal anesthesia for cesarean section.
1 Introduction
Nausea and vomiting during regional anesthesia for cesarean section still remain a big problem not only for the patient only but for the surgeon and the anesthesiologist as well. The etiology of intraoperative nausea and vomiting is complex; it may be attributed to surgical stimulation, hypotention, vagal stimulation and uterotonic drugs. Patient demographic data and anesthetic technique also have a role [Citation1].
A plenty of pharmacological approaches including dopamine receptor antagonists (e.g. metoclopramide), butyrophenones (e.g. dropridol), antihistaminic (diphenhydramine), anticholinergic drugs (atropine) and steroids (dexamethazone) have been used as a prophylactic antiemetic during regional anesthesia for cesarean section; however, these drugs may cause side effects such as sense of drowsiness, dystonia and extrapyramidal signs [Citation2].
Granisetron is selective antagonist of 5-hydroxytryptamine type 3 (5-HT3) receptors and it is an efficient antiemetic during and after regional anesthesia for cesarean section [Citation3,Citation4]. A combination of granisetron and dexamethasone has been reported to be a more powerful than granisetron alone [Citation2].
Benzodiazepines including midazolam have been reported to be a good alternative for the usual antiemetics in controlling persistent postoperative nausea and vomiting [Citation5].
We hypothesized that a combination of midazolam and dexamethazone given after cord clamping, would be effective as granisetrone–dexamethazone combination in reducing postdelivery and postoperative nausea and vomiting in women undergoing cesarean delivery under regional anesthesia with low cost.
2 Patient and methods
After the gaining of institutional ethical approval and written informed consent from the participants, the study was performed in 240 women ASA I and II (American Society of Anesthesiologists), with uncomplicated pregnancies, who were scheduled for elective cesarean delivery under spinal anesthesia. Exclusion criteria included patients who had gastrointestinal diseases, those who had a history of previous postoperative emesis, or an antiemetic medication within 24 h before surgery. All parturients received 1000 ml lactated Ringer’s solution IV over 30 min before spinal injection. The subjects were allocated randomly to three groups, using a computer-generated randomization code. The group I (n = 80) received saline (placebo), while group II (n = 80) received 2 mg granisetron plus 8 mg dexamethasone IV immediately after clamping of the fetal umbilical cord and group III (n = 80) received 2 mg midazolam plus 8 mg dexamethasone IV immediately after clamping of the fetal umbilical cord. The drug solutions in all groups were prepared by one anesthesiologist and they looked identical. Another anesthesiologist, who was blinded to the study, gave the drugs. All staff in the operating room was unaware of the randomization code. After placement of standard monitors, spinal anesthesia with 0.5% hyperbaric bupivacaine according to height (2.6 ml for patients taller than 155 cm and 2.4 ml for those shorter than 155 cm) was administered. After induction of spinal anesthesia, the parturient was placed supine with left uterine displacement and head up with slight trendlenberg of the table to achieve adequate surgical block (T4 sensory level) which was assessed by analgesia to pinprick with fine dental needle. Non-invasive arterial blood pressure was measured every 3 min until the end of surgery. Supplementary oxygen 3 L/min was administered. Ringer lactate was administered IV infusion (4 ml/kg/h) with replacement of any fluid deficit or blood loss more than 1000 cc. Uterus was routinely exteriorized in all cases. Maternal hypotension (decrease in systolic blood pressure of >10% from baseline) after spinal anesthesia was treated aggressively with additional IV fluid, more uterine tilt, and increments of IV phenylephrine 25 μg. After delivery of the baby, 5 U of IV oxytocin was given to all parturient to enhance uterine contraction.
Nausea and vomiting were evaluated and recorded every 10 min intraoperatively and at 2 h, 4 h, 6 h, 12 h and 24 h postoperatively by an independent anesthetist who is blinded to group assignment. Nausea was assessed using visual analogue score (VAS; 0, no nausea; 10, worst imaginable nausea). An antiemetic “rescue” drug (10 mg metoclopromide intravenously) was administered in case of severe nausea (nausea VAS 4 or more) or vomiting within the study period.
Data were also collected regarding the duration of surgery, amount of phenylephrine consumed and complications (headache, drowsiness, blurred vision, allergic reactions). Patient satisfaction was evaluated and recorded based upon the whole patient experience regarding antiemesis during the study period (10-point verbal numeric scoring system, 0 = not at all satisfied, 10 = fully satisfied). Sedation was assessed in the postanaesthetic care unit (PACU) with modified Ramsey sedation score (RSS) [Citation6] (Awake levels were: 1, patient anxious and agitated or restless or both; 2, patient co-operative, orientated, and tranquil; 3, patient responds to commands only. Asleep levels were dependent on the patient’s response to a light glabellar tap or loud auditory stimulus: Level 4, a brisk response; 5, a sluggish response; and 6, no response) intraoperatively and postoperatively.
3 Statistical analysis
To test the normality of data distribution K–S (Kolmogorov–Smirnov) test was done. Normally distributed data were subjected to parametric tests.
Data values were expressed as frequency (%), means ± SD, or medians (ranges). The analysis of the data was done to test statistical significant difference between groups. Differences between groups were analyzed by the analysis of variance (ANOVA) followed by least significant difference (LSD) test for the post hoc comparison. Student t-test was used to compare between two groups. Chi square test was used for qualitative data; P is significant if it is <0.05. A prior power analysis indicated that 80 patients in each group would be sufficient to detect a 20% reduction in the incidence of nausea and vomiting, with a type-I error of 0.05 and a power of approximately 90%. The statistical analysis of data done by using excel program and SPSS program statistical package for social science version 17 (SPSS Inc., Chicago, USA).
4 Results
The three groups were not significantly different with respect to demographic characteristics, level of sensory block, gestational age, phenylephrine dose and duration of surgery ().
Table 1 Patients characteristics and intraoperative data.
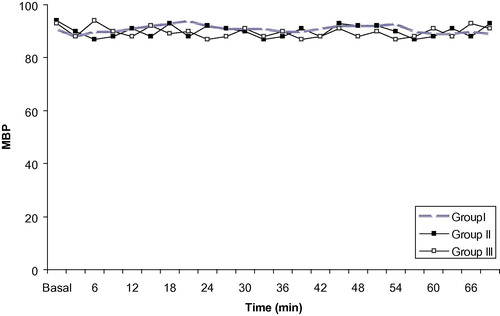
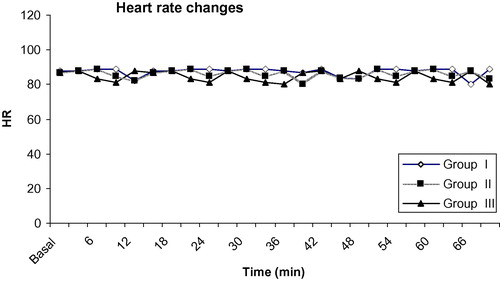
Nausea and vomiting were statistically significant less in groups II, III during operation after delivery of the fetus and for 24 h postoperatively. Also, nausea and vomiting were statistically significant less in group II when compared to group III during the same period. There was no statistically significant difference between the groups in the incidence of nausea and vomiting intraoperatively before delivery of the fetus (). The use of antiemetic rescue was statistically significant high in group I when compared to group II, III during operation and postoperatively. Also parturients in group III received statistically significant less antiemetic rescue drug when compared to group II during operation and postoperatively. Sedation was statistically significant high in groups III when compared to group I and II during operation. Whereas, there were no statistically significant difference between groups postoperatively (). All Groups were statistically comparable as regard to mean arterial blood pressure and heart rate ( and ).
Table 2 Incidence of nausea and vomiting.
Table 3 Patient satisfaction and side effects.
Patient satisfaction with PONV control was higher with the active treatment groups (II and III) compared with group I, whereas, groups II and III were comparable regarding patient satisfaction. There was no statistically significant difference in the incidence of adverse effects between the three groups ().
5 Discussion
Pregnant women are more liable for occurrence of nausea and vomiting than nonpregnant patients, this is due to the high level of progesterone which causes smooth muscle relaxation, decreases lower esophageal sphincter tone, decreases gastrointestinal motility and increases gastrin secretion [Citation5]. Moreover, when those pregnant women undergo spinal anesthesia for cesarean section; an additional risk of intraoperative postdelivery emetic symptoms is added; this can be attributed to postinduction hypotension which may lead to brainstem hypoxia and stimulation of vomiting center [Citation7,Citation8].
In this study, to avoid the influence of hypotension on the results, rapid fluid infusion, left uterine displacement, or administration of phenylephrine were performed, so that the difference in use of antiemetic during and after cesarean section under spinal anesthesia can be attributed to the study drug combination.
Granisetron is one of 5HT3 receptor antagonists which were introduced in 1991 [Citation9], and it is devoid of drawbacks of traditional used antiemetics, no change in vital signs and no interaction with concomitant used anesthetics [Citation10].
Dexamethasone was used as effective antiemetic for cancer patients receiving chemotherapy [Citation11], tonsillectomy [Citation12,Citation13], thyroidectomy [Citation14], laparoscopic surgery and abdominal hysterectomy [Citation15]. Glucocorticoids are known to have multiple effects on central nervous system. They have an effect on neurotransmitter concentrations, receptor densities, signal transduction and neurone configuration [Citation16,Citation17]. Many receptors for the glucocorticoids are found in the nucleus of the solitary tract, the raphe nucleus and the area postrema. These nuclei are reported to have marked role in regulation of emetic symptoms [Citation18,Citation19].
We chose to evaluate the use of a granisetron/dexamethasone combination in comparison with midazolam/dexamethasone for reducing nausea and vomiting in patients during and after spinal anesthesia for cesarean section. Our results showed statistically significant decrease for nausea and vomiting in groups II and III when compared with group I during operation after delivery of the fetus and for 24 h postoperatively. But, there was a statistically significant decrease for nausea and vomiting in group II when compared with group III during the same period. Also, the use of rescue antiemetic drug was statistically significant high in group I when compared to group II, III and in group III when compared to group II during operation and postoperatively.
Our results are in agreement with a study showed that a combination of granisetron and dexamethasone is more effective for controlling emetic symptoms during and after spinal anesthesia for cesarean delivery than granisetron alone [Citation2]. How dexamethasone enhances granisetron is not known exactly, it is suspected that dexamethasone may antagonize stimulation of 5-HT receptors [Citation20,Citation21]. Fujii and his colleagues did not register significant side effects of using this combination apart from increased cost of antiemetic therapy [Citation2].
In contrast to our result, Balki et al. [Citation1] found that prophylactic granisetron does not prevent postdelivery nausea and vomiting during elective cesarean delivery under spinal anesthesia. This may be attributed to use of dexamethasone in addition to granisetron.
In a double blind randomized study by Tarhan et al. [Citation5], it was reported that a subhypnotic dose of midazolam was an effective antiemetic as a subhypnotic dose of propofol for pregnant women undergoing cesarean section under spinal anesthesia. This is in accord with our study. Midazolam may exert its antiemetic effect through interference with neuronal reuptake of adenosine which will reduce synthesis, release and postsynaptic action of dopamine at CRTZ [Citation5,Citation22]. Also, it is thought that benzodiazepines including midazolam bind to receptors on gamma amino butyric acid (GABA) – ergic neurons which are suspected to have an inhibitory effect on central dopaminergic pathways [Citation5,Citation23]. All of this beside the anxiolytic effect of midazolam may explain its antiemetic effect [Citation5,Citation24].
In our study, we suspected that addition of dexamethasone to midazolam will increase its efficacy as an antiemetic and will be comparable with granisetron–dexamethasone combination. But our results showed a significant increased incidence of emetic symptoms with midazolam–dexamethasone combination in comparison with granisetron–dexamethasone combination; beside significant increased incidence of unwanted sedation in a patient undergoing regional anesthesia.
In Egypt, granisetron (56 Egyptian pounds for 2 mg) and dexamethasone. (3 Egyptian pounds for 8 mg) are much more expensive than midazolam (3.5 Egyptian pounds for 2 mg) and dexamethasone. However, a decision about antiemetics should not be limited to these costs but should also consider the outcome of the patients and the overall cost of care if emesis was to occur. A cost-effective analysis, defined as the cost per unit of success was not performed in this study.
Our study has a few limitations. We did not include other antiemetic combination rather than those used .The second limitation is that non-pharmacological antiemetic methods was not used. So further studies are needed.
In summary, a combination of midazolam and dexamethasone given after cord clamping, is not effective as granisetron–dexamethasone combination in reducing post delivery and postoperative nausea and vomiting in women undergoing cesarean delivery under regional anesthesia.
Notes
Available online 13 May 2011
References
- M.BalkiS.KasodekarS.DhumneJ.A.CarvalhoProphylactic granisetron does not prevent postdelivery nausea and vomiting during elective cesarean delivery under spinal anesthesiaAnesth Analg1042007679683
- Y.FujiiY.SaitohH.TanakaH.ToyookaGranisetron/dexamethasone; combination for reducing nausea and vomiting during and after spinal anesthesia for cesarean sectionAnesth Analg88199913461350
- Y.FujiiH.TanakaH.ToyookaGranisetron prevents nausea and vomiting during spinal anaesthesia for caesarean sectionActa Anaesthesiol Scand421998312315
- Y.FujiiH.TanakaH.ToyookaPrevention of nausea and vomiting during and after spinal anaesthesia for caesarean section with granisetron, droperidol and metoclopramide: a randomized, double-blind, placebo-controlled trialActa Anaesthesiol Scand421998921925
- O.TarhanN.CanbayS.CelebiA.UzunF.SahinU.CoskunAyparSubhypnotic doses of midazolam prevent nausea and vomiting during spinal anesthesia for cesarean sectionMinerva Anesthesiol732007629633
- M.A.RamsayT.M.SavegeB.R.SimpsonR.GoodwinControlled sedation with alphaxalone–alphadoloneBMJ21974656659
- S.DattaM.H.AlperG.W.OstheimerJ.B.WeissMethods of ephedrine administration and nausea and hypotention during spinal anesthesia for cesarean sectionAnesthesiology5619826870
- C.K.PatraR.P.BadolaK.P.BhargavaA study of factors concerned in spinal anesthesiaBr J Anaesth44197212081211
- W.SneaderDrug Discovery: A History2005John Wiley and Sons Ltd.West Sussex, Englandp.217–19.
- Y.ErhanE.ErhanH.AydedeO.YumusA.YenturOndansetron, granisetron, and dexamethasone compared for the prevention of postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy: a randomized placebo-controlled studySurg Endosc226200814871492
- M.S.AaproD.S.AlbertsDexamethasone as an antiemetic in patients treated with cisplatinN Engl Med3051981520
- A.L.S.PappasR.SukhaniA.J.HotalingM.Mikat StevensJ.J.JavorskiJ.DonzelliK.SenoyThe effect of preoperative dexamethasone on the immediate and delayed postoperative morbidity in children undergoing adenotonsillectomyAnesth Analg8719985761
- W.M.SplinterD.J.RobertsProphylaxis for vomiting by children after tonsillectomy: dexamethasone versus perphenazineAnesth Analg851997534537
- J.J.WangS.T.HoS.C.LeeY.C.LiuY.H.LiuY.C.LiaoThe prophylactic effect of dexamethasone on postoperative nausea and vomiting in women undergoing thyroidectomy: a comparison of droperidol with salineAnesth Analg891999200203
- Y.FujiiH.TanakaH.ToyookaThe effect of dexamethasone on antiemetics in female patients undergoing gynecologic surgeryAnesth Analg851997913917
- B.P.SchimmerK.L.ParkerAdrenocorticotropic hormone; adrenocortical steroids and their synthetic analogs; inhibitors of the synthesis and actions of adrenocortical hormonesJ.G.HardmanL.E.LimbirdP.B.MolinoffR.W.RuddonGoodman and Gillman’s the Pharmacological Basis of Therapeutics9th edn.1996McGraw-HillNew York14591486
- M.MorimotoN.MoritaH.OzawaK.YokoyamaM.KawataDistribution of glucocorticoid receptor immunoreactivity and mRNA in the rat brain: an immunohistochemical and in situ hydridization studyNeurosci Res261996235269
- J.W.FunderMineralocorticoid receptors and glucocorticoid receptorsClin Endocrinol451996651656
- R.J.NaylorF.C.InallThe physiology and pharmacology of postoperative nausea and vomitingAnaesthesia49199425
- J.CarmichaelB.M.J.CantwellC.M.EdwardsA pharmacokinetic study of granisetron (BRL 43694A), A selective 5-HT3 receptor antagonist: correlation of anti- emetic responseCancer Chemother Pharmacol2419894549
- B.M.S.AaproP.M.PleziaD.S.AlbertsDouble-blind crossover study of the antiemetic efficacy of high-dose dexamethasone versus high dose metoclopramideJ Clin Oncol21984466471
- J.K.OlynykS.R.CullenM.F.LeahyMidazolam: an effective anti-emetic agent for cytotoxic chemotherapyMed J Aust1501989466467
- H.UnlugencT.GulerY.GunesG.IsikComparative study of the entiemetic efficacy of ondansetron, propofol and midazolam in the early postoperative periodEur J Anaesthesiol2120046065
- K.P.BauerP.M.DomA.M.RamirezJ.E.O’FlahertyPreoperative intravenous midazolam: benefits beyond anxiolysisJ Clin Anesth162004177183