Abstract
Background and objectives
Early ambulation after hemorrhoidectomy as an outpatient procedure can be provided by perianal block with local anesthesia. The objective of this study was to compare the analgesic effects of dexamethasone locally and intravenously when combined with bupivacaine and to compare it with bupivacaine as a sole local anesthetic in the perianal block technique for ano-rectal surgeries.
Patients and methods
60 ASA I, 20–40 years of age male patients, undergoing ano-rectal surgeries under perianal block local anesthesia were randomly allocated to one of three groups: Bupivacaine group, Local dexamethasone (LD) group and Intravenous dexamethsone (IVD) group. Measurements included the onset of sensory and motor blockade, duration of analgesia, VAS at 6 h following rescue analgesic, and postoperative nausea and vomiting.
Results
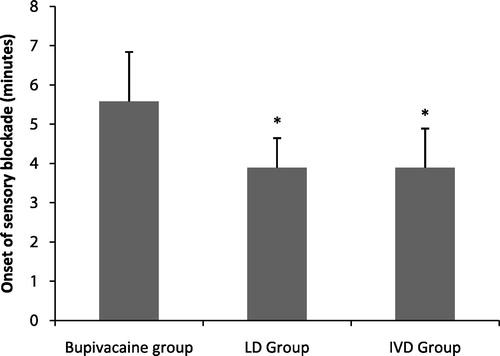
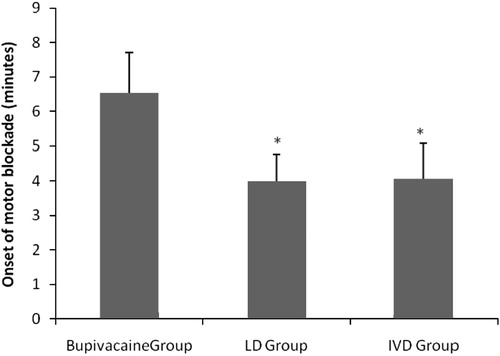
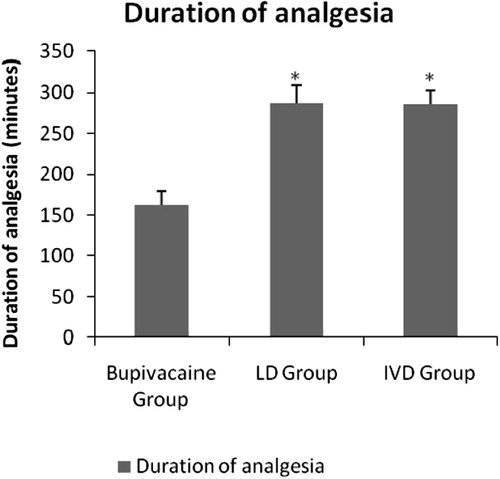
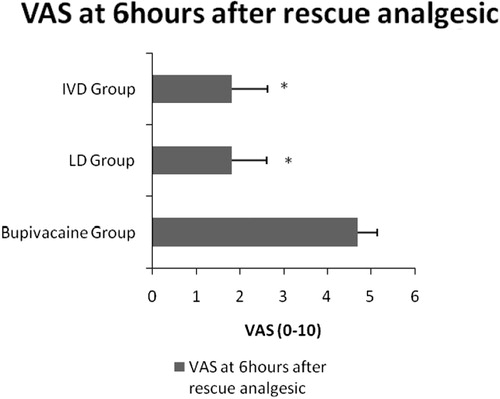
The onset of sensory and motor blockade was significantly shorter in the LD and IVD groups than in the bupivacaine group (3.8 ± 0.7, 4 ± 0.7 vs. 3.8 ± 0.9, 4 ± 1 vs. 5.5 ± 1.2, 6.5 ± 1.1, respectively, P < 0.01). The duration of analgesia was significantly prolonged in the LD and IVD groups compared to the bupivacaine group (287.7 ± 21 vs. 286.2 ± 16.9 vs. 162.3 ± 16.9, respectively, P < 0.01). Postoperative VAS was significantly lower in the LD and IVD groups compared to the bupivacaine group (1.8 ± 0.8 vs. 1.8 ± 0.8 vs. 4.7 ± 0.4, respectively, P < 0.01). The incidence of nausea and vomiting were significantly lower in the dexamethasone groups.
Conclusion
Dexamethasone when used as an adjuvant to bupivacaine in the perianal block for ano-rectal surgeries can accelerate the onset of blockade and prolong the postoperative analgesia.
1 Introduction
Hemorrhoidectomy is traditionally viewed as a very painful surgery because of wounds in the particularly sensitive anal canal. General or spinal anesthesia was classically performed for anal surgeries as an inpatient procedure. Many studies have recently shown the feasibility of successfully performing anorectal surgeries under perianal block (PAB) [Citation1]. This provided distinctive advantages as increasing the number of day case hemorrhoidectomies as well as providing several hours of postoperative pain relief.
Different adjuvants as vasoconstrictors, opioids, clonidine and corticosteroids have been added to local anesthetics in order to prolong the duration of different blocks thus allowing better postoperative patient comfort and decreasing perioperative analgesics consumption and their subsequent side-effects [Citation2]. Studies investigating the analgesic efficacy of adding corticosteroids to local anesthetic agents have been encouraging [Citation3–Citation4]. Dexamethasone microspheres have been shown to increase the duration of the intercostal nerve block in animal and human studies [Citation5]. Dexamethasone has been also found to prolong the duration of axillary block as well as intravenous regional anesthesia [Citation6]. The analgesic effect of local spinal and systemic corticosteroids in combination with bupivacaine has been also reported [Citation7].
In spite of these studies, the exact mechanism of action of dexamethasone prolongation of the duration of local anesthetic blocks is not yet clearly understood and whether it is due its local or systemic effects [Citation3–Citation8].
The purpose of this controlled study was thus to evaluate and compare the effect of dexamethasone given intravenously or added locally to bupivacaine, in patients undergoing ano-rectal surgeries by perianal block, on the onset of sensory and motor blockade, duration of analgesia and postoperative nausea and vomiting.
2 Patients and methods
After approval of the ethical committee and obtaining informed written consent, 60 American Society of Anesthesiologists I 20–40 years of age male patients underwent open hemorroidectomy, fistulectomies and fissurectomies under perianal block local anesthesia. Patients with known hypersensitivity to local anesthetics or dexamethsone, neurologic diseases, gastric discomfort, diabetes mellitus and coagulation disorders were excluded from the study.
Patients were randomly allocated by closed envelops to three groups. Patients and anesthesiologist who performed the perianal block were blinded to group allocation.
Bupivacaine group (n = 20): received local anesthetic mixture of (20 ml bupivacaine 0.5% + 20 ml normal saline) + 2 ml of normal saline intravenously.
Local dexamethasone (LD) group (n = 20): received local anesthetic mixture of (20 ml bupivacaine 0.5% + 18 ml normal saline + 2 ml of 8 mg dexamethasone) + 2 ml of normal saline intravenously.
Intravenous dexamethasone (IVD) group (n = 20): received local anesthetic mixture of (20 ml bupivacaine 0.5% + 20 ml normal saline) + 2 ml of 8 mg dexamethasone intravenously at the same time with local anesthesia.
10 min before entering the operating room (OR) an IV line was inserted and 0.05 mg/kg of midazolam + 0.02 mg/kg of ketamine + 25 mg meperidine were given as intravenous premedication and upon entering the OR all patients received routine monitoring including five lead electrocardiogram, non-invasive blood pressure monitoring and pulse oxymetry. Lactated ringer solution was infused and oxygen 4–6 L/min was applied via face mask.
Patients were placed in the lithotomy position and buttocks were taped apart. The anesthetic mixture was prepared for the bupivacaine and IVD groups by mixing 20 ml of 0.5% bupivacaine (actavis PTCehf, Bucaine® 0.5%) with 20 ml of normal saline and for LD group by mixing 18 ml of normal saline and 2 ml of dexamethasone with 20 ml of 0.5% bupivacaine. We have used 25 G spinal needle (Unisis Corp., Tokyo, Japan) which was fitted onto 50 ml syringe. The technique of the block as guided by Reshma and Begani [Citation9] and Nystrom et al. [Citation10] was done through 6 punctures at 6, 9, 12 and 3, O’clock then two punctures were done midway between 3 and 6 O’clock and mid way between 6 and 9 O’clock toward 12 O’clock and all punctures were done about 3–5 cm deep into ischiorectal fossa. At the end, we anesthetized the perianal skin circumferentially. This technique would block the sphincter and anal canal by targeting branches from the internal pudendal, and sacrococcygeal nerves.
2.1 Measurements
The onset of sensory and motor blockade was monitored every minute after the end of injection of the LA mixture and was assessed by loss of sensation to pinprick and relaxation of the sphincter, respectively.
The duration of analgesia was measured after the onset of sensory blockade till the patient’s first request of analgesia which was confirmed by asking the patient to score his pain by the visual analog score consisting of 10 cm line with 0-cm representing no pain and 10-cm representing worst pain, when VAS > 3 was confirmed an oral analgesia (rescue analgesic) was given in the form of Piroxicam (feldene flash) 20 mg + paracetamol 500 mg.
Thereafter the VAS was assessed at 6 h after rescue analgesic. During the 6 h period if any patient asked for analgesia and confirmed by VAS > 3, paracetamol 500 mg was given orally with a maximum dose of 1000 mg per single dose and 4000 mg per day
Postoperative complications in the form of nausea and vomiting were recorded by the attending nurse till the end of 6 h after rescue analgesics and were managed by intravenous Granitryl (Granisetron) 1 mg/ml.
In the event of failure to achieve sensory and motor blockade, general anesthesia was induced and the patient was excluded from the study.
2.2 Statistical analysis
The primary outcome variable was the duration of analgesia. Based on a previous pilot study we expected the duration of analgesia to be 240 (SD, 40) minutes after the administration of bupivacaine alone. To demonstrate that the addition of 8 mg dexamethasone to bupivacaine would prolong the duration of analgesia by 20%, we calculated that 12 patients per group were required to detect a statistically significant difference between groups with α = 0.05 and 80% power. However, to allow for the comparisons between the 3 groups, an adjusted P (Bonferroni correction) of 0.025 was considered significant for the primary outcome and the required sample size increased to 15 per group. A total of 20 patients in each group were included to compensate for possible dropouts.
Data were presented as mean (SD). Parametric and non-parametric versions of ANOVA test were used for an analysis of continuous and discrete data, as appropriate, with post hoc tests done if significance was detected. A P-value of <0.05 was considered statistically significant. All statistical calculations were done using computer programs Microsoft Excel 2003 (Microsoft Corporation, NY, and USA) and SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
3 Results
56 male patients completed the study (19 in bupivacaine group, 18 in LD group and 19 in IVD group), and four patients were excluded from the study because of unsuccessful blockade where general anesthesia was induced. Patients characteristics () (including age, body mass index and duration of surgery) were comparable between the three groups (P = 0.5 vs. 0.7 vs. 0.9, respectively)
Table 1 Patient characteristics and duration of surgery.
The onset of sensory blockade () was faster in the LD group (3.8 ± 0.7 min) and IVD group (3.8 ± 0.9 min) when compared to the bupivacaine group (5.5 ± 1.2 min, P-value < 0.01). Both LD group and IVD group showed comparable results.
The onset of motor blockade () was significantly faster in the LD group (4 ± 0.7 min) and IVD group (4 ± 1 min) when compared with the bupivacaine group (6.5 ± 1.1 min, P-value < 0.01). The aforementioned parameter was comparable between LD and IVD groups.
The duration of analgesia () was significantly prolonged in the LD group (287.7 ± 21 min) and the IVD group (286.3 ± 16.9 min) when compared to the bupivacaine group (162.3 ± 16.9 min, P-value < 0.01) and it was comparable between both groups.
VAS at 6 h after rescue analgesic () tended to be significantly lower in the LD Group (1.8 ± 0.8) and the IVD group (1.8 ± 0.8) compared to the bupivacaine group (4.7 ± 0.4, P-value < 0.01) and it was comparable between both groups.
In the bupivacaine group, 5 patients complained of nausea compared with 2 patients in the LD group and this difference did not reach statistical significance, while no patient complained of nausea in the IVD group and the difference between it and the bupivacaine group was statistically significant (P < 0.05). 2 patients in the bupivacaine group developed vomiting and it was not recorded in the dexamethasone groups ().
Table 2 Postoperative nausea and vomiting.
4 Discussion
In this randomized controlled study done on 56 male patients under perianal block for hemorroidectomy, we demonstrated that adding dexamethasone to bupivacaine resulted in faster onset of blockade and a prolonged duration of analgesia with lower incidence of nausea and no vomiting.
There is an evidence based recommendation for adoption of the perianal blocks for anorectal surgeries [Citation11] instead of spinal or general anesthesia. Anannamcharoen et al. [Citation12] found that perianal block offers more advantages over spinal block concerning less urinary retention and extended analgesia in the postoperative period. For the young population the postoperative spinal headache comes as one of the most annoying complications [Citation13] and this justified concern also directed the attention toward the use of perianal blocks for these kinds of surgeries.
The known mechanism of analgesic action of corticosteroids is through occupying glucocoticoid receptors of different cells [Citation14]; therefore, it acts on the nociceptor C fibers which are encased in single Schwann cell sheath [Citation15]. Its mode of action does not include blockade of Na channels that are distributed along the unmyelinated fibers, but they act through the potassium channels [Citation16]. Therefore, dexamethasone and bupivacaine act on the same nociceptor fibers but with two different mechanisms and blockade of C fibers will close the gate of pain transmission thus producing preemptive analgesic effect.
Parrington et al. [Citation17] did not find any difference in the onset of sensory or motor blockade when they added dexamethasone to mepivacaine which is of low hydophobicity for supraclavicular brachial plexus block. Bigat et al. [Citation6] as well did not demonstrate the rapid onset of sensory or motor blockade when they added dexamethasone to moderately hydrophobic lidocaine for intravenous anesthesia. Another study [Citation11] found that perianal block with mixed bupivacaine–lignocaine results in a rapid onset of blockade.
In this study, we have selected the highly hydrophobic agent bupivacaine with consequent high potency but slower onset than moderately or low hydrophobic local anesthetic [Citation15], and we found that adding dexamethsone locally and intravenously as well to bupivacaine resulted in a more rapid onset of sensory and motor blockade than using bupivacaine without dexamethasone.
Nerve conduction depends on Na+–K+ pump and depolarization switches both Na+ and K+ channels to an active form. Furthermore, Na+ entry would produce further depolarization that leads to more opened Na+ channels; however, the action potential is not complete till enough K+ channels become opened to initiate repolarisation [Citation15]. The blockade effect of corticosteroid on K channels and its consequence on the onset of blockade remains to be a question for further investigations.
The analgesic effects of adding dexamethasone to local anesthetics have been extensively studied in peripheral nerve blocks with lack of studies in local infiltration blocks. A study [Citation17] demonstrated that dexamethsone combined with mepivacaine can extend the duration of analgesia in brachial plexus block. In our study, the use of dexamethsone as an adjuvant to bupivacaine has resulted in a longer duration of analgesia when compared with the bupivacaine group and this is consistent with Gupta [Citation19] who demonstrated the shorter duration of anaesthesia when using local infiltration with local anaesthetic alone as compared to adding dexamethasone to the local anesthetic.
In this context, Vargas and Ross [Citation20] and Watters et al. [Citation21] demonstrated a decline in postoperative required analgesic with a preemptive use of oral and intravenous dexamethasone. In our study, VAS was significantly lower with dexamethasone groups and in consistent with our findings Curda et al. [Citation22] found that subcutaneous injection of the combined dexamethasone and bupivacaine reduces postoperative pain scores and King [Citation23] found that intravenous dexamethasone results in lower postoperative pain scores after discectomy surgery. Furthermore, Glasser et al. [Citation7] showed that wound infiltration with combined methyl prednisolone–bupivacaine had reduced postoperative required doses of narcotics.
In this context the comparable effects of both local and intravenous dexamethasone may be due to the preemptive effect on the nociceptor C fibers and suppression of the inflammatory response that results from intraoperative tissue trauma [Citation24].
The implication of the importance of our finding in reducing postoperative requirement of analgesics in this kind of ambulatory surgery refers to, if there was a frequent request for postoperative analgesic there would be a delay in-home discharge, increase in hospital costs and patient dissatisfaction.
In this study we have only used a single dose of dexamethasone. The half life of this long acting corticosteroid is about 36–54 h and it was found that the single dose does not inhibit the hypothalamic pituitary –adrenal axis. While, large doses of corticosteroids were found to impair wound healing, mask the febrile response to infection and increase the gastrointestinal discomfort [Citation25,Citation26].
The preservative in the steroid preparation which is benzyl alcohol and insoluble steroid particle matter have focused the attention of the suspected neurotoxicity of dexamethasone when injected perineurally [Citation27,Citation28], therefore, the US Food and drug administration did not approve the use of local dexamethasone as an adjuvant to local anesthetics. However, the neurotoxicity of dexamethasone has been [Citation29,Citation30] discussed in the pain text books and it was found that 4–12 mg of dexamethsone through epidural, perineural and intravenous routes has no neurotoxic effects. Furthermore many studies [Citation31] have not found long term effects on the function of peripheral nerves by using locally applied corticosteroids.
The antiemetic effects of dexamethasone is still ill defined, one of the proposed mechanisms is the presence of glucocorticoid receptors on the central nuclei that are involved in the control of nausea and vomiting [Citation32,Citation33]. In this study the antiemetic rule of dexamethasone was highly significant not only by the venous route but also through the local route which may be due to systemic absorption. Many studies [Citation34,Citation35] have demonstrated the antiemetic rule of intravenous corticosteroids while Parrington et al. [Citation17] observed lower incidence of nausea and vomiting with local dexamethasone.
To the best of our knowledge this is the first report comparing intravenous and local dexamethasone as adjuvants to bupivacaine in anorectal surgeries.
We conclude that in the perianal block, when dexamethasone, whether intravenous or local is added to bupivacaine, it produces a rapid onset of blockade and can extend the postoperative analgesia.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- P.AphinivesPerianal block for ambulatory hemorrhoidectomy, an easy technique for general surgeonJ Med Assoc Thai.922009195197
- J.G.FosterP.H.RosenbergClinically useful adjuvants in regional anaesthesiaCurr Opin Anaesthesiol162003477486
- A.MovafeghM.RazazianF.HajimaohamadiA.MeyasamieDexamethasone added to lidocaine prolongs axillary brachial plexus blockAnesth Analg1022006263267
- P.A.VieraI.PulaiG.C.TsaoP.ManikantanB.KellerB.ConnellyDexamethasone with bupivacaine increases duration of analgesia in ultrasound-guided interscalene brachial plexus blockadeEur J Anesthesiol272010285288
- C.DrogerD.BenzigerF.GaoC.B.BerdeProlonged intercostals nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheresAnesthesiolgy851996969974
- Z.BigatN.BoztugN.HadimiogluDoes dexamethasone improve the quality of intravenous regional anesthesia and analgesia?Anesth Analg1022006605609
- R.S.GlasserR.S.KnegoJ.B.DelashawR.G.FesslerThe perioperative use of corticosteroids and bupivacaine in the management of lumbar disc diseaseJ Neurosurg781993383387
- H.TaguchiK.ShinguH.OkudaH.MatsumotoAnalgesia for pelvic and perineal cancer pain by intrathecal steroid injectionActa Anaesthesiol Scand462002190193
- P.J.ReshmaM.M.BeganiProctological surgery as day care: 8 year experience of a successful day care centreBombay Hosp J502008179183
- P.O.NystromK.DerwingerR.GerjyLocal perianal block for anal surgeryTech Coloproctol820042326
- R.Saranga BharathiV.SharmaA.K.DabasA.ChakladarEvidence based switch to perianal block for ano-rectal surgeriesInt J Surg8120102931
- S.AnannamcharoenP.CheeranontC.Boonya-usadonLocal perianal nerve block versus spinal block for closed hemorrhoidectomy: a randomized controlled trialJ Med Assoc Thai9112200818621866
- D.TurnbullD.ShepherdPost-dural puncture headache: pathogenesis, prevention and treatmentBr. J. Anaesth.9152003718729
- D.J.KopaczP.G.LacoutureD.WuThe dose response and effects of dexamethasone on bupivacaine microcapsules for intercostals blockade (T9YT11) in healthy volunteersAnesth Analg962003576582
- Strichartz GR, Berde CB, Local anesthetics. In: Miller RD (Ed.), Anesthesia, 5th ed. New York, Churchill Livingstone, 2000, pp. 491–521.
- B.AttardiK.TakimotoR.GealyC.SevernsE.S.LevitanGlucocorticoid induced up-regulation of a pituitary K+ channel mRNA in vitro and vivoRecep Channel11993287293
- S.ParringtonW.ChanD.Brown-ShrevesR.SubramanyamDexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockadeReg Anesth Pain Med352010422426
- A.GuptaWound infiltration with local anaesthetics in ambulatory surgeryCurr Opin Anaesthesiol2362010708713
- J.H.Vargas3rdD.G.RossCorticosteroids and anterior cruciate ligament repairAm J Sports Med171989532534
- W.C.Watters3rdA.P.TempleM.GranberryThe use of dexamethasone in primary lumbar disc surgery. A prospective, randomized, double-blind studySpine141989440442
- G.A.CurdaPostoperative analgesic effects of dexamethasone sodium phosphate in bunion surgeryJ Foot Surg221983187191
- J.S.KingDexamethasone – a helpful adjunct in management after lumbar discectomyNeurosurgery141984697700
- G.BrodnerE.PogatzkiH.Van AkenH.BuerkleC.GoetersC.SchulzkiH.NottbergN.MertesA multimodal approach to control postoperative pathophysiology and rehabilitation in patients undergoing abdominothoracic esophagectomyAnesth Analg861998228234
- A.SalernoR.HermannEfficacy and safety of steroid use for postoperative pain relief update and review of the medical literatureJ Bone Joint Surg88200613611372
- E.NovakS.S.StubbsC.E.SeckmanM.S.HearronEffects of a single large intravenous dose of methylprednisolone sodium succinateClin Pharmacol Ther111970711717
- H.T.BenzonA.J.GissenG.R.StrichartzM.J.AvramB.G.CovinoThe effect of polyethylene glycol on mammalian nerve impulsesAnesth Analg661987553559
- H.T.BenzonT.L.ChewR.J.McCarthyH.A.BenzonD.R.WalegaComparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroidsAnesthesiology1062007331338
- Williams BA, Neumann KJ, Goel SK, Wu C. Postoperative pain and other acute pain syndromes. In: Benzon HT, Rathmell JP, Wu CL, Turk DC, Argoff CE, editors. Raj’s Practical Management of Pain. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Racz GB, Noe CL. Pelvic spinal neuraxial procedures. In: Raj P, Lou L, Serdar E, et al., editors. Interventional pain management. 2nd ed. Philadelphia, PA: Saunders Elsevier; 2008.
- A.JohannsenL.DahlinJ.M.KernsLong term local corticosteroid application does not influence nerve transmission or structureActa Anaesthesiol Scand391995364369
- J.W.FunderMineralocorticoid receptors and glucocorticoid receptorsClin Endocrinol451996651656
- R.J.NaylorF.C.InallThe physiology and pharmacology of postoperative nausea and vomitingAnaesthesiology49199425
- A.L.S.PappasR.SukhaniA.J.HotalingM.Mikat- StevensThe effects of preoperative dexamethasone on the immediate and delayed postoperative mortality and morbidity in children undergoing adenotonsillectomyAnesth Analg8719985761
- Y.FujiiH.TanakaH.ToyookaThe effects of dexamethsone on the antiemetics in the female patients undergoing gynecologic surgeryAnesth Anal851997913917
Further reading
- Z.BigatN.BoztugN.HadimiogluN.CeteN.CoskunfiratE.ErtokDoes dexamethasone improve the quality of intravenous regional anesthesia and analgesia? A randomized, controlled clinical studyAnesth Analg10222006605609