Abstract
Background
Mirtazapine is a specific serotonergic antidepressant drug. The aim of this study was to compare the efficacy of mirtazapine as PONV prophylaxis with a classic 5HT3 receptor antagonist; ondansetron.
Methods
Eighty female patients with high PONV risk undergoing prophylactic mastectomy with a standardized anesthetic were randomized to receive either an oral disintegrating tablet (ODT) of mirtazapine 30 mg (group M) or ondansetron 16 mg (group O) 1 h before surgery. Preoperative anxiety level was assessed by state and trait anxiety inventory before taking the study drug and 1 h after. Vital sign variables, the incidence of PONV, the use of rescue antiemetic, complete response, postoperative VAS pain scores, the inverted observer’s assessment of alertness/sedation scale and side effects were compared.
Results
Mirtazapine premedication reduced preoperative state anxiety inventory scores (P < 0.01) and the incidence of early nausea and late vomiting (P < 0.05). The percentage of patient having complete responses during the first 24 h after anesthesia was 75% after mirtazapine and 65% after ondansetron prophylaxis. Anesthetic requirements, postoperative pain, sedation scores, and side effects were similar between the two groups.
Conclusion
Mirtazapine prophylaxis reduces preoperative anxiety and the incidence of postoperative early nausea and late vomiting compared with ondansetron, without untoward sedative or cardiovascular effects.
Keywords:
1 Introduction
Women undergoing breast surgery are at particular high risk for the development of postoperative nausea and vomiting (PONV) and an incidence of 60–80% in the placebo group has been reported in many studied [Citation1–Citation3]. Women who elected to undergo prophylactic mastectomy (surgery to remove one breast in hopes of preventing or reducing risk of breast cancer in women who had cancer in the other breast) reported experiencing higher rate of anxiety and depression associated with developing breast cancer [Citation4].
Mirtazapine is a noradrenergic and specific serotonergic antidepressant. It is anxiolytic by virtue of its antagonist of the 5HT2 receptor, and is strongly sleep inducing. Its antagonist at 5HT3 receptor may help to prevent nausea and vomiting [Citation5]. The use of mirtazapine in the management of nausea and vomiting has been reported in the literature, both for treatment [Citation6], and premedication [Citation7]. However, the comparison between mirtazapine as PONV prophylaxis and other 5HT3 receptor blockades have not been studied.
The aim of this study was to compare the efficacy of mirtazapine as PONV prophylaxis with ondansetron in women undergoing prophylactic mastectomy.
2 Methods
After approval of the hospital ethics committee and informed patient written consent to this double-blind study, 80 ASA physical status 1 or 2 women undergoing prophylactic mastectomy were enrolled in this study. Patients who were smokers, or with gastrointestinal disorders, clinically significant major organ disease, or who had received other antidepressant drugs or an anti-emetic within 48 h before surgery were excluded.
Patients were randomly divided into two equal groups using computer-generated random numbers with the closed-sealed envelope, to receive either an oral disintegrating tablet (ODT) of mirtazapine 30 mg (group M) or ondansetron 16 mg (group O) 1 h before surgery. To insure the study was blinded, the nurse who prepared or administered the study drugs was not involved in patient care.
Preoperative anxiety levels using the Spielberger state and trait anxiety inventory (STAI) were assessed before taking the study drug, 1 h (immediately before induction of anesthesia), and 24 h after. STAI is a well-established instrument for the self-reporting of anxiety in the preoperative context [Citation8]. A score for each, ranging between 20 and 80; may then be calculated by an investigator using a scoring key [Citation9] with higher scores indicate more anxiety.
Patients fasted overnight before their scheduled operation. No additional premedication was given. On arrival in the operating room, electrocardiogram, pulse oximetry, noninvasive arterial blood pressure, and peripheral temperature monitoring were applied. Baseline vital signs were obtained and subsequent values were recorded every 5 min throughout surgical procedure. Anesthesia was induced with fentanyl 1.5 μg/kg and propofol 1.5–2.5 mg/kg until loss of eyelash reflex. Tracheal intubation was facilitated with rocuronuim 0.5 mg/kg. Anesthesia was maintained with isoflurane (1–2.5%), nitrous oxide in 40% oxygen and intermittent doses of muscle relaxant if needed to maintain adequate muscle relaxation throughout the procedure. The respiratory tidal volume was adjusted to keep end-tidal CO2 at 4.8–5.2%. The isoflurane concentration was adjusted to keep heart rate and blood pressure within 20% of preinduction values throughout the anesthesia period. All surgical procedures were completed by the same surgeon. At the end of surgery, atropine 0.02 mg/kg and neostigmine 0.05 mg/kg were given IV for antagonism of neuromuscular blockade. Time to awaken (from the end of anesthesia until the patients opened their eyes on command) and time to the first dose of postoperative analgesia were recorded. Postoperatively, nalbuphine 20 mg IM was prescribed every 4 h or as requested by the patients. The ward nurses were instructed to omit the four hourly doses if they considered that the patient was over sedated or pain free (pain levels below four on visual analog scale; VAS). Postoperative pain intensity was rated by the patients using a 10-cm VAS, with 0 = no pain and 10 = the worst pain imaginable. The patient’s level of sedation was assessed using the inverted observer’s assessment of alertness/sedation (OAA/S) scale [Citation10] with a score of 1 = awake alert to 5 = asleep, unarousable. The postoperative data (e.g. vital signs, pain, and sedation scale) were collected every 4 h. The occurrences of early (0–2 h), delayed (2–24 h) and total (0–24 h) PONV were recorded [Citation11]. Nausea was defined as a subjectively unpleasant sensation associated with awareness of the urge to vomiting. Vomiting was the forceful expulsion of gastric contents from the mouth. The severity of nausea was assessed using a verbal numerical rating scale from 0 = no nausea and 10 = nausea as bad as it could be. For the purpose of data collection, retching (the same as vomiting but without expulsion of gastric contents) was considered vomiting. If patients experienced nausea for 30 min, or more than one emetic episode in 15 min, rescue antiemetic treatment consisted of metoclopramide 10 mg IV every 4 h. Complete response was defined as no PONV or no administration of rescue antiemetic during 24 h after surgery. Duration of hospital stay and incidence of side effects (headache, dizziness, elevated liver enzymes, somnolence, or dry mouth) were recorded. Blood samples were taken from all patients preoperatively and after 1 week postoperatively to compare liver enzymes level (SGPT).
2.1 Statistical analysis
Power analysis revealed a sample size of 40 patients per group, was sufficient to achieve a power of 80% with α error at 0.05 and β at 0.2 to detect a clinically relevant 30% reduction in the total frequency of PONV [Citation12]. Parametric data were analyzed by Student’s t test; frequencies of nausea, and vomiting were analyzed by using χ2 test or Fisher’s exact test with small values. The VAS data were analyzed by using the Mann–Whitney’s U test. A value of P < 0.05 was considered statistically significant. Commercial SPSS 11.0 software for window and Graph pad In Stat version 3.0 were used for data processing.
3 Results
There were no differences in patient demographics, the simplified risk score by Apfel et al. [Citation13], and operative characteristics; (duration of anesthesia, propofol induction dose, the concentration of isoflurane for maintenance, and recovery time) between the two groups (). There was no difference in mean baseline vital signs values (heart rate, blood pressure, and Spo2) or in subsequent values during surgery and analgesia between the two groups. We found significantly lower preoperative state-anxiety level in M group at 1 h after mirtazapam administration compared with group O ().
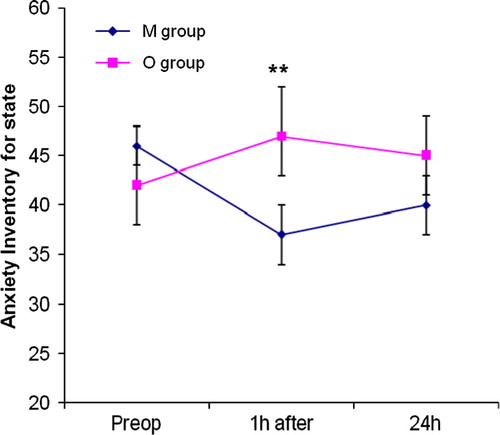
Table 1 Patient demographics and operative characteristics in mirtazapine M and ondansetron O groups. Data expressed in mean (SD), numbers (n).
demonstrates the incidence of nausea and vomiting during different observatory periods. The total mean verbal nausea assessment score was significantly lower in the M group compared with O group during 0–24 h postoperatively (mean ± SD; 1.9 ± 2.3 versus 3.2 ± 2.1; P < 0.05). The incidence of nausea between groups was statistically significant during early (0–2 h) observation period (P < 0.05). However, the incidence of vomiting was statistically less during late (2–24 h) observation period in the M group (P < 0.05). Numbers of patients with two or more emetic episodes and the requirement for rescue antiemetic were significantly reduced in M group versus O group (P < 0.05). The 95% confidence interval (CI) for total PONV/24 h ranges from 0.3607 to 1.414 (relative risk = 0.7143).
Table 2 Number of patients (%) with nausea and vomiting in mirtazapine (group M) and ondansetron (group O), at intervals 0–2, 2–24, 0–24 h after the end of surgery.
Postoperative wound pain scores (VAS) at rest are reported in . Pain scores were less than 4 in all patients. There were no statistically significant differences in the postoperative pain scores or in the rescue pain medication between groups. Also there were no significant differences in the mean sedation score between groups. There were no significant differences in incidence of none-emetic postoperative side effects or duration of hospital stay among the two groups.
Table 3 Pain and sedation score, first opioids request, nalbuphine consumption, incidence of side effects, and time to discharge.
4 Discussion
This study showed that administration of ODT of 30 mg mirtazapine compared with 16 mg ondansetron, 1 h before operation in women at high risk undergoing prophylactic mastectomy, reduced preoperative anxiety and incidence of postoperative early nausea and late vomiting, without untoward sedative or cardiovascular effects.
In this study, the percentage of patients with no PONV over first 24 h after anesthesia were 75% after mirtazapine prophylaxis and 65% after ondansetron prophylaxis. The dosage of ondansetron and mirtazapine used is similar to that recommended for optimal oral dose to prevent PONV. The optimal dose of ondansetron to prevent PONV is likely to be 8 mg IV or 16 mg orally as suggested from several multicentre trials [Citation14]. Dosed orally or intravenously, the mean elimination half-life of ondansetron is approximately 3 h. There are potential advantages of using ODT form of ondansetron which disperses rapidly when placed under tongue without taking a drug with water and absorbed into the circulation more slowly than IV form, thus providing a longer period of effective blood level [Citation15]. Blockage of receptors in the chemoreceptor trigger zone before the arrival of emetic stimuli associated with anesthesia and surgery provides greater and long acting antiemetic efficacy [Citation16]. The literature contains a few reports on the use of the ODT form of ondansetron for PONV in adult [Citation17,Citation18]. The incidence of complete response is reported as frequent as in our work after 16 mg ondansetron tablets [Citation19].
Mirtazapine ODT is rapidly absorbed after oral administration and peak plasma level with the onset of action is reached within about 1.6 h. The elimination half-life ranges from 20 to 40 h. The anxiolytic and sleep-improved effects of mirtazapine are more rapid in onset within 1 h of oral administration; a result from the blockade of 5HT2 receptors in fasting patients [Citation20]. Anxiety or mirtazapine independently affects neither the propofol dose required for unconsciousness nor the anesthetic requirements and cardiovascular events that follow propofol induction. The evidence for a link between preoperative anxiety and PONV from previous results remains weak [Citation21,Citation22]. Our results demonstrate that mirtazapine was associated with less incidence of early nausea with lower grade during 24 h postoperative period compared with ondansetron prophylaxis. Quinn et al. [Citation23] survey has demonstrated an association between pre-operative anxiety and postoperative nausea but not vomiting. It has also been suggested that nausea and vomiting are separate entities and that nausea is not the normal and inevitable precursor to vomiting [Citation24]. Anxiolytic and sleep-improved agent as mirtazapine may be beneficial as a part of prophylactic anti-nausea measures.
The low incidence of early postoperative vomiting in both groups may have been related to the use of propofol for induction. Propofol has been alleged to possess direct antiemetic action even when administered in sub hypnotic doses [Citation25]. A previous study has found postoperative opioids to be one of the main predictors of PONV in the late postoperative period [Citation26]. In both groups, patients had similar pain scores and used nearly similar amounts of nalbuphine in the first 24 h postoperatively. The high incidence of late vomiting after ondansetron compared with mirtazapine premedication in our study setting might have related to short half life of ondansetron and to the fact that nalbuphine-induced vomiting can last for a much longer periods. A wide individual variation in sensitivity to narcotics could be another explanation for this.
However, there are certain limitations in this study. First, group sizes with more patients may be required to demonstrate statistically significant reduction in the incidence of nausea and vomiting in both early and late observation periods in the treatment groups. Second, placebo control group was not used as there is a reported evidence of high risk of PONV among female patients undergoing breast surgery for long duration. It is unethical to use placebo tablet in this trial. Third, 5HT3 antagonists with short duration of action were used in comparison with long acting mirtazapine. Dosed orally or intravenously, the mean elimination half-life of tropisetron is 8 h [Citation27]. Ondansetron, a 5HT3 antagonist, is the “gold standard” antiemetic because of its safety and efficacy compared with alternatives. Fourth, no control was used for the issue of postoperative opioids administration. Anderson et al. [Citation28] showed an almost linear relation between the dose of postoperative opioids and the incidence of vomiting. It appears to be in the best interest of patients in this study to use less emetogenic alternatives rather than opioids for postoperative analgesia, e.g. local anesthesia, as regional blockade or as wound infiltration, paracetamol, and non-steroidal anti-inflammatory agents [Citation29].
In conclusion, this study showed that premedication with ODT of mirtazapine 30 mg, versus ondansetron 16 mg may reduce the level of preoperative anxiety and the incidence of early nausea and late vomiting in high-risk female patients undergoing prophylactic mastectomy under general anesthesia.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- B.HammasS.E.ThornM.WattwilSuperior prolonged antiemetic prophylaxis with a four-drug multimodal regimen – Comparison with propofol or placeboActa Anaesthesiol Scand462002232237
- Y.FujiiH.TanakaH.ToyookaProphylactic antiemetic therapy with granisetron–dexamethasone combination in women undergoing breast surgeryActa Anaesthesiol Scand42199810381042
- S.SadhasivamA.SaxenaS.KathirvelT.R.KannanA.TrikhaV.MohanThe safety and efficacy of prophylactic ondansetron in patients undergoing modified radical mastectomyAnesth Analg89199913401345
- M.B.M.TanE.M.A.BleikerM.B.Menke-PluymersA.R.Van GoolS.van DoorenB.N.Van GeelM.M.Tilanus-linthorstJ.G.Ba KlijinC.T.BrekeimansC.SeynaeveStandard psychological consultations and follow up for women at increased risk of hereditary breast cancer considering prophylactic mastectomyHered Cancer Clin Pract7200969
- G.L.StimmelJ.A.DopheideS.M.StahlMirtazapine: an antidepressant with noradrenergic and specific serotonergic effectsPharmacotherapy1719971012
- A.RohdeJ.DembinskiC.DornMirtazapine (Remergil) for treatment resistant hyperemesis gravidarum: rescue of a twin pregnancyArch Gynecol Obstet2682003219221
- C.-C.ChenC.-S.LinY.-P.KoY.-C.HungH.-C.LaoY.-W.HsuPremedication with mirtazapine reduces preoperative anxiety and postoperative nausea and vomitingAnesth Analg1062008109113
- I.MaranetsZ.N.KainPreoperative anxiety and intraoperative anesthetic requirementAnesth Analg89199913461351
- A.P.MorleyC.H.PapageorgiouA.M.MarinakiD.J.CooperC.M.LewisThe effect of preoperative anxiety on induction of anesthesia with propofolAnaesthesia632008467473
- D.A.ChernikD.GillingsH.LaineJ.HendlerJ.M.SilverA.B.DavidsonE.M.SchwamJ.L.SiegelValidity and reliability of the observer’s assessment of alertness/sedation scale: study with intravenous midazolamJ Clin Psychopharmacol101990244251
- C.C.ApfelN.RoewerK.KorttilaHow to study postoperative nausea and vomitingActa Anaesthesiol Scand462002921928
- J.LermanStudy design in clinical research: sample size estimation and power analysisCan J Anesth431996184191
- C.C.ApfelE.LaaraM.KoivurantaC.A.GreimN.RoewerA simplified risk score for predicting postoperative nausea and vomiting: conclusion from cross-validation between two centersAnesthesiology911999693700
- M.R.TramerJ.M.ReynoldsR.A.MooreH.J.McQuayEfficacy, dose–response, and safety of ondansetron in prevention of postoperative nausea and vomiting. A quantitative systemic review of randomized placebo-controlled trialsAnesthesiology87199712771289
- A.PiratS.F.TuncayA.TorgayS.CandanG.ArslanOndansetron, orally disintergrating tablets versus intravenous injection for prevention of intrathecal morphine-induced nausea, vomiting, and pruritus in young malesAnesth Analg101200513301336
- J.TangB.WangP.F.WhiteM.F.WatchaJ.QiR.H.WenderThe effect of timing of ondansetron administration on its efficacy, cost-effectiveness, and cost-benefits as a prophylactic antiemetic in the ambulatory settingAnesth Analg861998274282
- T.J.GanR.FraniakJ.ReevesOndansetron orally disintegrating tablet versus placebo for the prevention of postdischarge nausea and vomiting after ambulatory surgeryAnesth Analg94200211991200
- K.s.ThagaardS.SteineJ.ReaderOndansetron disintegrating tablets of 8 mg twice a day for 3 days did not reduce the incidence of nausea or vomiting after laparoscopic surgeryEur J Anaesthesiol202003153157
- R.JokelaM.KoivurantaT.Kangas-SaarelaS.PurhonenS.AlahuhtaOral ondansetron, tropisetron or metoclopramide to prevent postoperative nausea and vomiting: a comparison in high-risk patients undergoing thyroid or parathyroid surgeryActa Anaesthesiol Scand462002519524
- C.j.TimmerJ.M.SitsenL.P.DelbressineClinical pharmacokinetics of mirtazapamClin Pharmacokinet382000461474
- M.F.WatchaP.F.WhitePostoperative nausea and vomiting: its etiology, treatment and preventionAnesthesiology771992162184
- J.E.Van den BoschK.G.MoonsG.J.BonselC.J.KalkmanDoes measurement of preoperative anxiety have added value for predicting postoperative nausea and vomitingAnesth Analg100200515251532
- A.C.QuinnJ.H.BrownP.G.WallaceA.J.AsburyStudies in postoperative sequelae. Nausea and vomiting-still a problemAnaesthesia4919946265
- G.R.MorrowThe assessment of nausea and vomiting. Past problems, current issues and suggestion for future researchCancer53198422672278
- A.BorgeatO.H.G.Wilder-SmithM.SaiahK.RifatSubhypnotic doses of propofol possess direct antiemetic propertiesAnesth Analg741992539541
- C.C.ApfelP.KrankeM.H.KatzVolatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial designBr J Anaesth882002659668
- R.C.LeeG.L.PloskerD.McTavishTropisetron. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential as an antiemeticDrugs461993925943
- B.J.AndersonC.J.RalphA.W.StewartC.BarberC.HolfordThe dose-effect relationship for morphine and vomiting after day-case tonsillectomy in childrenAnaesth Intensive Care282000155160
- V.DahlJ.C.RaederNon-opioid postoperative analgesiaActa Anaesthesiol Scand44200011911203