Abstract
Objective
Mucosal bleeding during FESS often interferes with optimal visualization of the nasal surgical field and can impair the safety and efficiency of the procedure. This study was conducted to evaluate the efficacy of tranexamic acid and Epsilon Aminocaproic Acid to decrease bleeding and improve visualization of the surgical field during FESS.
Materials and methods
A total of 90 patients ASA I-II aged from 18 to 50 years and undergoing FESS for chronic sinusitis were enrolled in this study. Surgery was performed under general anesthesia patients were randomly assigned to three equal groups (30 patients each), patients in TXA group received intravenous tranexamic acid 10 mg/kg diluted in 100 ml saline. EACA group received intravenous Epsilon Aminocaproic Acid 100 mg/kg diluted in 100 ml saline and the control group received IV 100 ml normal saline (all infusions were through 10 min). The duration of surgery, volume of blood loss, pre and postoperative hemoglobin, MAP and HR, surgical field quality surgeon satisfaction and side effects were recorded.
Results
The duration of surgery was significantly less in TXA and EACA groups than the control group (121.1 ± 7.1 min), (120.8 ± 6.0 min), versus (146.1 ± 7.3 min) volume of blood loss in TXA group and EACA group was comparable (195.3 ± 32.2 ml) and (201.5 ± 30.6 ml) but each of them has significant less blood loss than the control group (365.1 ± 48.8 ml). The postoperative hemoglobin was significantly lower in the control group (11.9 ± 0.4 gm/dl) compared to TXA group (12.6 ± 0.2 gm/dl) and EACA group (12.4 ± 0.2 gm/dl). Both TXA and EACA groups had comparable improved quality of the surgical field with most of patients classified as grade 1 and 2 according to Boezaart scale while the control group had most of patients in grade 3, accordingly the surgeon satisfaction is significantly higher in TXA and EACA groups compared to the control group. No significant difference in side effects between all groups.
Conclusion
Intravenous tranexamic acid and Epsilon Aminocaproic Acid (EACA) effectively reduce bleeding during FESS and improve visualization of the surgical field and so increase the surgeon satisfaction with no significant difference between both drugs.
1 Introduction
Functional endoscopic sinus surgery is a skillful minimally invasive surgical technique widely used for management of chronic rhinosinusitis and chronic polypous rhinosinusitis. Mucosal bleeding often interferes with optimal visualization of the nasal surgical field [Citation1] and can impair the safety and efficiency of the procedure, as it may prolong the duration of surgery due to the need for frequent suctioning, or increase the incidence of surgical complications as injury of orbital vasculature [Citation2].
Many factors including arterial blood pressure, heart rate, and coagulation disorders have great effect on bleeding in FESS, so various maneuvers are used to decrease bleeding and provide clear surgical field, e.g. local vasoconstrictors, elevation of the patient’s head, use of beta blockers and controlled hypotensive anesthesia [Citation3]. In some patients bleeding cannot be controlled by the previous techniques and other alternatives are required, one of them is the use of antifibrinolytic drugs as tranexamic acid and Epsilon Aminocaproic Acid (EACA), previous studies proved the efficacy of these agents to reduce bleeding in patients undergoing cardiac surgery, major orthopedic, spine and prostatic surgeries [Citation4–Citation6]. Some dental surgeons used tranexamic acid as a mouthwash for dental extractions [Citation7]. Tranexamic acid and Epsilon Aminocaproic Acid are synthetic derivatives of amino acid lysine that produce reversible blockade of lysine binding sites on plasminogen molecules, so reducing the conversion of plasminogen to plasmin which is responsible for the degradation of blood clots [Citation4,Citation5].
This study was conducted to evaluate the efficacy of two antifibrinolytic agents; Tranexamic acid and Epsilon Aminocaproic Acid (EACA) to control and limit bleeding and improve visualization of the surgical field during FESS procedures.
2 Materials and methods
This randomized controlled comparative study was done in ENT surgical theater in Kasr El-Ainy Hospital. The study was approved by the hospital ethics committee, and a written informed consent was taken from every patient during the preoperative visit.
A total of 90 patients aged from 18 to 50 years and undergoing FESS for chronic sinusitis were enrolled in this study. All patients were: ASA I and-II. Patients with uncontrolled hypertension, renal or hepatic dysfunction, coronary or cerebral artery disease, autonomic disturbance, deep vein thrombosis or peripheral vascular disease, bleeding diathesis and patients receiving anticoagulants were excluded from the study.
Patients were randomly assigned to three equal groups (30 patients each); TXA group to receive iv tranexamic acid, EACA group to receive iv Epsilon Aminocaproic Acid and control group to receive normal saline. Randomization was done by means of computer-generated codes. The anesthesiologists, surgeons, and patients were blinded to study drugs, and an anesthesiologist not involved in study prepared the infusion drugs before induction of anesthesia.
After complete preoperative assessment (medical history, vital signs, and airway assessment), patients were explained about the procedure and advised to practice mouth breathing. All routine preoperative investigations were assessed (ECG, complete blood picture, kidney and liver functions), complete coagulation profile was assessed to exclude any coagulation defects. Upon arrival to the operating room monitors were applied (ECG, pulse oximeter, and non invasive measurement of arterial blood pressure) and a venous cannula was inserted on the dorsum of the hand. After application of 100% oxygen at 5 l/min for 5 min – while asking the patient to practice mouth breathing – anesthesia was induced with intravenous fentanyl 1 μg/kg, propofol 2 mg/kg, lidocaine 1.5 mg/kg and atracurium (0.5 mg/kg) to facilitate tracheal intubation with a suitable size cuffed ETT, then an oropharyngeal pack was inserted, and the patient was positioned with head up 30°. Anesthesia was maintained with isoflurane (1.5–2%), and 100% oxygen, controlled ventilation with a tidal volume of 10 ml/kg and respiratory rate of 10–12 breaths/min was adjusted to maintain end tidal CO2 at 30–35 mmHg.
After induction of anesthesia, patients in TXA group received intravenous tranexamic acid 10 mg/kg diluted in 100 ml saline administered during 10 min infusion. Patients in EACA group received intravenous Epsilon Aminocaproic Acid (EACA) 100 mg/kg diluted in 100 ml normal saline and infused over 10 min. The control group received 100 ml normal saline by intravenous infusion through 10 min. All the procedures were performed by the same anesthesia and surgical teams using the same surgical technique. Intraoperative monitoring included 5 leads ECG, arterial blood pressure (invasive method after insertion of 20 gauge cannula in the radial artery of the non dominant hand), pulse oximeter for arterial oxygen saturation, and end tidal carbon dioxide was assessed by capnogram. Moderate hypotensive anesthesia was used to maintain mean arterial pressure (MAP) around 55–65 mmHg during surgery by adjusting isoflurane concentration (1.5–2%) and infusion of nitroglycerine through a separate venous cannula (0.5–5 μg/kg/min) and titration of rate of infusion according to measurement of mean arterial blood pressure. Intraoperative fluid supply was obtained with 0.9% saline or lactated ringer’s solution (3 ml/kg/h and replacement of blood loss). At the end of surgery the oropharyngeal pack was removed, good suctioning of blood and secretions from the mouth was done under direct vision using the laryngoscope, and reversal of muscle relaxants was done by neostigmine 0.05 mg/kg and atropine 0.02 mg/kg and extubation is achieved when the patient is fully awake then the patient is instructed to breath from his mouth.
3 During the procedure the following data were assessed and recorded
| • | Intraoperative blood loss monitored directly from the collection into the calibrated bottle in the suction apparatus (100 ml graded suction canister) and the amount of irrigation solution used during the procedure was subtracted from the total amount of fluid accumulated in the suction device, also the volume of blood loss recorded by counting the number of cotton strips used during surgery, a fully soaked cotton strip was estimated to contain 5 ml blood and partially soaked one contains 2.5 ml blood. | ||||
| • | Duration of operation (from induction to extubation). | ||||
| • | Assessment of nitroglycerine requirement. | ||||
| • | Pre- and postoperative hemoglobin concentration. | ||||
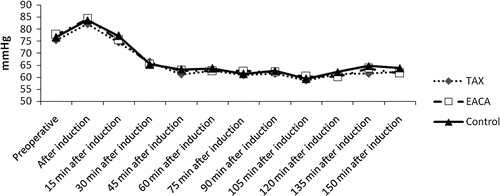
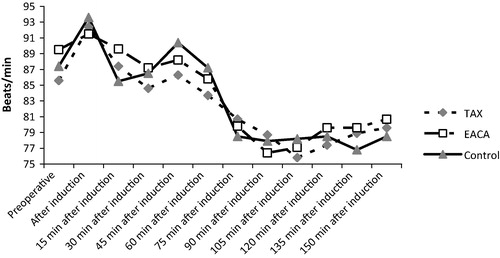
| • | Hemodynamic parameters: mean arterial blood pressure (MAP) and heart rate (HR) were recorded before induction of anesthesia as a base line, after induction of anesthesia, and recorded every 15 min till the end of surgery. | ||||
| • | Assessment of the quality of the surgical field by the surgeon with a predefined scale (Boezaart scale) at half an hour interval () [Citation8]. | ||||
| • | The surgeon satisfaction with the surgical field quality was graded by 5 items Likert scale as 1: not satisfied at all, 2: slightly satisfied, 3: moderately satisfied, 4: very satisfied, 5: extremely satisfied [Citation9]. | ||||
| • | The incidence of any side effects e.g., nausea, vomiting, pruritus, fever, postoperative epistaxis and clinical evidence of thrombus development was assessed for at least 24 h. | ||||
Table 1 Boezaart et al. grading scale for scoring of surgical field bleeding [Citation8].
4 Statistical analysis
Data were analysed using IBM SPSS Advanced Statistics version 20.0 (SPSS Inc., Chicago, IL). Numerical data were expressed as mean and standard deviation. Chi-square test (Fisher’s exact test) was used to examine the relation between qualitative variables. For quantitative data, comparison between the 3 groups was done using ANOVA test, then post-Hoc “Schefe test” was used for pair-wise comparison. A p-value <0.05 was considered significant.
Power analysis was done based on volume of blood loss and bleeding score of 3 between the 3 study groups. For volume of blood loss, Student’s t test for independent samples was chosen to perform the analysis, the power of statistical comparison was 19% in between TXA and EACA, while it was more than 95% if comparing between either TXA, or EACA to control group, while Fisher Exact test was chosen for bleeding score 3. The power of statistical comparison between TXA and EACA was less than 20%, while it was more than 95% if done between either of them and the control group. α-error level was fixed at 0.05 and the sample size was entered to be 30 participants in each group. Calculations were done using PS Power and Sample Size Calculations Software, version 3.0.11 for MS Windows (William D. Dupont and Walton D. Vanderbilt, USA).
5 Results
A total number of 90 patients aged from 18 to 50 years were enrolled in this study. No significant differences were noted between the three groups in the study as regards the demographic data, but the duration of surgery was significantly less in tranexamic acid and EACA groups than the control group (121.1 ± 7.1 min), (120.8 ± 6.0 min), versus (146.1 ± 7.3 min) ().
Table 2 Demographic data and duration of surgery of the 3 groups.
As for nitroglycerine requirement it showed no significant difference between TXA group (12.6 ± 2.5 mg) EACA group (12.4 ± 2.4 mg) and control group (12.6 ± 2.7 mg). Volume of Blood loss in TXA group and EACA group was comparable with no significant difference between both groups (195.3 ± 32.2 ml) and (201.5 ± 30.6 ml) (p = 0.822) but each of them has significant lower amount of blood loss as compared to control group (365.1 ± 48.8 ml) ().
Table 3 Pre- and postoperative hemoglobin concentration and volume of blood loss in the three studied groups.
The postoperative hemoglobin concentration was significantly lower in the control group (11.9 ± 0.4 gm/dl) compared to TXA group (12.6 ± 0.2 gm/dl) and EACA group (12.4 ± 0.2 gm/dl) with no significant difference between the latter two groups ().
The MAP and HR were comparable in the three groups with no statistically significant differences between them. However, all values were within the clinically accepted ranges ( and ).
The quality of the surgical field depending on Boezaart scale is shown in . There were no significant difference between TXA and EACA groups in all measurement times as most of patients were classified as grades 1 and 2, while the control group had most of patients in grade 3 with significant difference relevant to the other two groups, no patient was found in grade 4 or 5 in all groups.
Table 4 Quality of the surgical field according to Boezzart scale.
The surgeon satisfaction of the surgical field during surgery based on five points Likert scale also showed no significant difference between TXA and EACA group, but both groups showed significantly higher satisfaction compared to control group ().
Table 5 Surgeon satisfaction according to Likert’s scale (5 points scale).
The three groups were comparable as regards the side effects. Only 4 patients in TXA group and 3 patients in EACA group have nausea and vomiting compared to 3 patients in control group, no patient had postoperative epistaxis in TXA and EACA groups, while there was one case in the control group. None of the patients showed signs or symptoms of thromboembolic events.
6 Discussion
During endoscopic sinus surgery, excessive bleeding represents a major problem for both the surgeon and the anesthesiologist. Bleeding is difficult to control in this procedure due to anatomical and surgical reasons.
There is a great role of the anesthesiologists in improving the surgical conditions to achieve bloodless field for better visualization of the intranasal structure [Citation10], and to avoid the risk of surgical complications as damage of orbit or optic nerve, unintended penetration of the middle cranial fossa, or even damage of internal carotid artery. FESS is better done under general anesthesia and several methods were used to reduce surgical field bleeding e.g. reverse trendelburg position up to 30°, local mucosal vasoconstrictors, and controlled hypotension [Citation3].
In this study antifibrinolytic drugs (Tranexamic acid and Epsilon Aminocaproic Acid) were used as i.v adjuvants to decrease the surgical field bleeding, and improve visualization. There was a significant decrease in the volume of intraoperative blood loss, and duration of surgery with significant improvement in the quality of the surgical field in both groups (TXA and EACA) compared to the control group.
Tranexamic acid and Epsilon Aminocaproic Acid are widely and effectively used to reduce blood loss and subsequent need for blood transfusion in oral, orthopedic, spinal, cardiac surgery, liver transplantation and prostate surgery [Citation11–Citation13].
Tranexamic acid (TXA) and Epsilon Aminocaproic Acid (EACA) are synthetic lysine analogs and act as inhibitors of fibrinolysis as they bind to the lysine binding sites on plasminogen, inhibiting binding to fibrin, and thus suppressing the whole process of fibrinolysis. These agents inhibit the natural degradation of fibrin and so stabilize clots [Citation10], they have no effect on blood coagulation parameters [Citation12].
The dose of antifibrinolytic drugs in the present study was within the dose range previously found to be effective, it has been proved that the mean duration of the effect of TXA and EACA is approximately 3 h. Considering the relatively short duration of FESS, so a single bolus dose of either drug was used, others in cardiac or orthopedic surgery used continuous infusion after the bolus dose [Citation13].
In this study there was no significant difference between all groups as regards the demographic characteristics, the MAP, and HR, and nitroglycerine requirements, and these results are concomitant with study of Alimian et al. [Citation9] that compared, the effect of 10 mg/kg tranexamic acid with placebo in 84 patients randomized into two equal groups and undergoing FESS, there was no significant difference in MAP, HR between both groups. Another study done by Abbasi et al., who compared the effect of two doses of intravenous tranexamic acid on two equal groups with 35 patients in each group were scheduled for endoscopic sinus surgery under general anesthesia, where group A received 5 mg/kg of TXA, while another 35 patients (group B) received 15 mg/kg iv TXA, no significant difference was found in MAP and HR between both groups in all measuring times [Citation14].
The duration of surgery was significantly less in both TXA and EACA groups compared to the control group. Also, the amount of blood loss was significantly less in both TXA and EACA groups (195.3 ± 32.2 ml), (201.5 ± 30.6 ml) compared to the control group (365.1 ± 48.8 ml), these results were in agreement with those of previous study of Alimian et al. [Citation9]. Where blood loss in TXA group (184 ± 64 ml) was significantly less than the placebo group (312 ± 75 ml) and p < 0.01.
Moise et al. used tranexamic acid 10 mg/kg, compared to saline group (30 patients in each group, the patients were undergoing FESS under general anesthesia, the study group received 10 mg/kg tranexamic acid in 10 ml saline solution and the control group received 10 ml saline solution with two administrations: before induction and before nasal pack removal, the results proved that the total blood loss intraoperatively and postsurgically decreased up to 50% level in the study group compared to the control group [Citation15].
The postoperative Hb concentration was significantly lower in the control group (11.9 ± 0.4) compared to TXA group (12.6 ± 0.2) and EACA group (12.4 ± 0.2) this is in agreement of the study of Abbas et al. who compared the effect of tranexamic acid to placebo in 32 patients undergoing bimaxillary osteotomy they received diluted tranexamic acid (20 mg/kg) or equal volume of normal saline intravenously just before induction of anesthesia, there was significant reduction in postoperative Hb of the control group 10.68 compared to tranexamic acid group 11.56 g/dl [Citation16].
Application of tranexamic acid or aminocaproic acid effectively reduced the amount of blood loss during other types of surgeries e,g orthopedic, cardiac, oral, and spine surgeries, these findings were in agreement with this study [Citation4–Citation7].
Camarsa et al. [Citation13] compared the efficacy of aminocaporic acid and tranexamic acid in control postoperative bleeding on removal of pneumatic tourniquet during total knee replacement the total blood loss was significantly less in antifibrinolytic group compared to control group (P < 0.01), no significant differences were found between EACA and TXA groups for any of outcome measures, this finding was also correlated to our study.
In cardiothoracic surgery many studies also proved the comparable effect of both drugs in reducing blood loss and need for blood transfusion as that done by Netti et al. for patients undergoing thoracic aortic surgery [Citation17].
The difference of the nature of endoscopic nasal surgery as FESS with limited anatomical space from orthopedic or cardiac surgery requires the need to improve the visualization of the surgical field. Validated scales were used to evaluate surgical field quality and surgeon satisfaction. In the current study the surgeons were more satisfied with the surgical field in TXA and EACA groups than the control group this was evidenced by using the Boezaart grading scale for scoring of surgical field bleeding as minimum or occasional suctioning required in all measurement times and most of patients were in grade 1 and 2 of Boezaart scale in both TXA and EACA groups with no significant difference between both groups in contrast to the control group which had most of patients in grade 3. Accordingly the surgeon satisfaction assessment by Likert scale showed that the surgeons were more satisfied with the surgical field in both TXA and EACA groups than the control group, this result was correlated with that of Alimian et al. who compared 10 ml/kg iv tranexamic acid with placebo, there was significant decrease in bleeding and higher surgeon satisfaction of the visibility of the surgical field in TXA group [Citation9].
The study of Jabalameli et al., and that of Yaniv et al. have comparable results to the current study as regards the improvement of quality of the surgical field and reduced volume of bleeding although they used topical and oral tranexamic acid in FESS [Citation18,Citation19] this may be due to local antifibrinolytic effect of the drug.
Other studies were not supporting the results of the current study as that of Mottaghi et al. [Citation20] who compared 500 mg of iv tranexamic acid with placebo in 50 patients undergoing FESS, there were no significant difference between both groups as regards SBP, DBP, MAP, HR, and there were similar results of changes in bleeding and surgeon satisfaction scores, these results do not agree with the results of the current study and other previous studies this may be related to difference in the surgical technique or difference in tissue hypertrophy, the different dose of tranexamic acid may also play a role in this different results as the dose used in Mottaghi et al. study was fixed dose 500 mg which may be less than the dose used in most studies.
On the other hand a study done by Athanasiadis et al. compared 30 patients undergoing FESS, the patients were randomized into three groups to receive either 2.5 g of EACA, 100 mg of TXA, or 1 g of TXA while the contralateral nasal side received saline, the solution was applied as spray, bleeding was documented using standardized videoscopy and grading scales, it concluded that tranexamic acid can reduce surgical site bleeding at 2, 4, 6 min after application, while the aminocaproic acid has no significant effect, this finding was different from the current study, this may be related to difference in method of application and time of assessment [Citation21].
Another study of Kushaga et al. [Citation22] comparing the effect of iv TXA, EACA and placebo for corrective spinal surgery where efficacy was determined by intraoperative and postoperative blood loss, they concluded that TXA is more effective in reducing blood loss than EACA or placebo. these results are contradicting with the comparable effect of TXA and EACA detected in the current study and other studies as that of Schauhan et al. [Citation23] comparing TXA and EACA in adult cardiac surgery, they concluded that both drugs are equally effective in reducing postoperative blood loss, also the study of Makhija et al. [Citation24] to evaluate efficacy and safety of TXA versus EACA in patients undergoing thoracic aortic surgery in 64 adult patients with (CPB) where TXA group patients received a bolus of 10 mg/kg of TXA followed by a maintenance infusion of 1 mg/kg/h until chest closure while the EACA group received a bolus of 50 mg/kg of EACA followed by a maintenance infusion of 25 mg/kg/h until chest closure where they found that cumulated mean blood loss and blood product requirement were comparable.
The incidence of side effects in all groups was comparable, they were related to nausea and vomiting (4 patient in TXA group, 3 patients in EACA group and 3 patients in control group), only one case of postoperative epistaxis in the control group. No reported cases of clinical thromboembolic events and this is comparable with all previous mentioned studies. Although not performing echo-Doppler systematically on patients enrolled in the study is considered as limitation of this study but many previous studies and isolated case reports considered much higher doses of antifibrinolytic drugs and continued the medication in the postoperative period with safe outcome [Citation9,Citation13].
Other limitation of the study is the exclusion of patients with the bleeding diathesis or impaired coagulation profile from the study in which the use of antifibrinolytic drugs could limit the blood loss.
In conclusion this clinical study has demonstrated that both intravenous tranexamic acid and aminocaproic acid effectively reduce bleeding during FESS and improve visualization of the surgical field and so increase the surgeon satisfaction with no significant difference between both drugs. They are cheap effective and safe drugs.
Acknowledgment
Great thanks to; Dr. Adel Eladwey the surgeon who helped us and had great effort in this study.
Notes
Available online 5 September 2014
References
- F.SaricaogluV.CelikerF.BasgulO.YapakeiU.AyparEffect of hypotensive anaesthesia on cognitive functions and recovery at endoscopic sinus surgeryEur J Anaesthesiol222005154163
- A.R.BakerA.B.BakerAnaesthesia for endoscopic sinus surgeryActa Anaesthesiol Scand542010795803
- Sumitha MaryJaccoloTony ThomsonChandyVergheseTCherianOral bisoprolol improves surgical field during Functional endoscopic sinus surgeryJ Anaesthiol Clin Pharmacol30120145964
- P.N.KaharN.GuptaP.GovilV.ShabEfficacy and safety of tranexamic acid in control of bleeding following TKR; a randomized clinical trialIndian J Anesth532009667671
- BhavanisVigayVikramBedrSubbroMitraBikramDasRole of tranexamic acid in reducing postoperative blood loss and transfusion requirement in patients undergoing hip and femoral surgeriesSJA7120132932
- H.FawazyE.ElmistekawyD.BonneauD.LatterL.FrotleCan local application of tranexamic acid reduce postcoronary bypass surgery blood loss. A randomized controlled trialJ Cardiothorac Surg4200925
- G.CarterA.GrossTranexamic acid mouth wash; a prospective randomized study of a 2 day regimen versus 5 day regimen to prevent postoperative bleeding in anticoagulated patients requiring dental extractionsInt J Oral Maxillofacial Surg322003504507
- A.P.BoezaartJ.Vander MerweA.CoetzuComparison of sodium nitroprusside and esmolol induced controlled hypotension for functional endoscopic sinus surgeryCan J Anesth421995373376
- M.AlimianM.MohseniThe effect of intravenous tranexamic acid on blood loss and surgical field quality during the endoscopic sinus surgery: a placebo controlled clinical trialJ Clin Anaesth232011611615
- P.MandalIsoflurane anaesthesia for functional endoscopic sinus surgeryIndia J Anaesth47120033740
- W.S.ChoiM.G.IrwinN.SammanThe effect of tranexamic acid on blood loss during orthoganic surgery; a randomized controlled trialJ Maxillo Facial Surg762009125133
- M.W.EortmannBasser A.A.KleinAntifibrinolytic agents in current anaesthetic practiceBr J Anaesth11142013459463
- M.A.CamarsalC.OlleM.Serra PratA.MartinM.SanchezP.RicosA.PerezL.OpissolEfficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement: a randomized clinical trialBJA9652006576582
- H.AbbasiS.BehdadV.AyatoliahiN.NazemianP.MirstiaamsiComparison of two doses of tranexamic acid on bleeding and surgery site quality during sinus endoscopy surgeryAdv Clin Exp Med2162013773780
- A.MoiseL.AgachiE.DragulinN.MincuG.SleleaTranexamic acid reduces with 50% the total nasal bleeding of patients that underwent functional endoscopic sinus surgeryEur J Anaesthesiol27472010115118
- AbbasKarimiSussan SoltaniMohammadiMahboobehHasheminasabEfficacy of tranexamic acid on blood loss during bimaxillary osteotomy: a randomized double blind clinical trialSJA6120124145
- NettiMakhjaAnjuSarupriaShivkumarChoudharySambhurumathDasRamakrishnanLakshnyUshaKiramComparison of Epsilon aminocaproic acid and Tranexamic acid in thoracic aortic surgery; clinical efficacy and safetyJ Cardiothorac Vascular Anaesth276201312011207
- M.Jabalamelik.ZakeriEvaluation of topical tranexamic acid on intraoperative bleeding in endoscopic sinus surgeryJIMS312006221223
- E.YanivJ.ShvertoT.HaddarHaemostatic effect of tranexamic acid in elective nasal surgeryAm J Rhinol202006227229
- K.MottaghiF.SafariA.SalimiS.MalekN.RahimiEvaluation of intravenous Tranexamic acid effects on bleeding, duration of surgery and surgeon satisfaction in endoscopic sinus surgeryJ Iran Anesth Crit Care Med Assoc Iran7220101429
- T.AthanasidiadisA.G.BeualP.J.WormaldEffects of topical antifibrinolytics in endoscopic sinus surgery: a pilot randomized controlled trialAm J Rhinol212007737742
- KushagaVemaThomas JErrioBaron SLonnerA Prospective randomized, double-blinded single-site control study comparing blood loss prevention of Tranexamic acid (TXA) to Epsilon Aminocaproic (EACA) for corrective spinal surgeryBMC Surg20101013
- SchauhanP.GhardeA.BisoiS.KaleU.JivaryA comparison of aminocaproic acid and tranexamic acid in adult cardiac surgeryAnna Cardiac Anesth720044043
- N.MakhijaA.Sarupria KumarS.ChoudharyS.DasR.LakshmyU.KiranComparison of Epsilon aminocaproic acid and Tranexamic acid in thoracic aortic surgery: clinical efficacy and safetyJ Cardio Thoracic Vascular Anesth276201312011207