Abstract
Objective
To compare the efficacy and safety of general anesthesia (GA) vs. spinal anesthesia (SA) in percutaneous nephrolithotomy (PCNL).
Methods
Two hundred patients were enrolled in a prospective randomized study to receive either GA or SA for PCNL. Patients’ characteristics, vital parameters, visual analog scale (VAS) and needs for additional analgesia were evaluated. Intraoperative and post-operative complications were recorded. Patients’ and surgeons’ satisfactions were also compared.
Results
Vital parameters were maintained at safe values throughout procedures in both groups. Visual analog pain score was lower in SA group till 1 h postoperative in comparison with GA group (P < 0.05). Patients in SA group recorded lower consumption of analgesia in the 1st postoperative day in comparison with GA group (P < 0.05). Postoperative shivering was higher in SA group than GA group (8% vs. 2%) while nausea and vomiting was higher in GA group than SA group (5% vs. 2% and 4% vs. 1% respectively). Patients in GA group reported higher overall satisfaction scores than SA group (mean 9.6 ± 0.4 vs. 8.6 ± 0.8, P < 0.05). Similarly, surgeon’ satisfaction score was higher in favor of GA group compared with SA group (mean 10 ± 00 vs. 8.3 ± 0.4, P < 0.05).
Conclusions
Both GA and SA are effective and safe in PCNL. SA has fewer complications and lower consumption of analgesia postoperatively. However, GA provides more satisfaction for patients and surgeon.
1 Introduction
Percutaneous nephrolithotomy (PCNL) is considered to be the gold standard treatment for renal calculi especially when limitations of extracorporeal shock wave lithotripsy (ESWL) are countered. PCNL can be performed under spinal (SA), epidural (EA) or general anesthesia (GA) [Citation1,Citation2]. From urological perspective, the particular advantages of GA in PCNL procedure include its feasibility to control tidal volume, secure patient airway especially in prone position, and extensibility of anesthesia time [Citation1,Citation3]. The feasibility to control tidal volume minimizes renal mobility secondary to respiration while extensibility of anesthesia time allow surgeon to create multiple punctures with subsequent increased efficacy of the procedure especially in cases with large stone burden. Moreover, GA is more comfortable for the patients and the ability to carry out prolonged operation in prone position without limitation of airway is another advantage [Citation3,Citation4]. On the other hand, SA has some advantage over GA, such as lower postoperative pain, lower consumption of analgesic drugs and avoidance of side effects from multiple medications used in GA [Citation5].
A limited number of prospective randomized trials have been carried out to establish which one of these procedures is better in decreasing perioperative complications [Citation5,Citation6]. Therefore impact of anesthesia type on efficacy of PCNL is still unclear. The aim of this study was to compare the efficacy and safety of GA vs. SA in patients undergoing PCNL.
2 Materials and methods
The study protocol was approved by local ethical committee. Between January 2011 through May 2013, 200 patients (ASA I or II) of either sex aged from 20 to 60 years underwent PCNL. All patients underwent preoperative evaluation including detailed history taking, physical examination, preoperative urine analysis, urine culture, serum creatinine level, complete blood count (CBC) and liver function tests, electrocardiography (ECG) and plain chest X-rays. For the detection of stone characteristics, intravenous urography (IVU) and/or non-contrast computed tomography were carried out.
Patients under chronic treatment with analgesics or corticosteroids, patient with contraindications to spinal anesthesia (coagulopathy, local infection…), allergy to local anesthetic solutions or opioids, patients with significant spinal, hepatic, cardiovascular, respiratory or psychiatric disorders were excluded from the study.
Patients with concomitant pelviureteric junction obstruction, horseshoe kidneys, concomitant ureteric stones, and those who did not will to be involved in randomization were also excluded from the study. After informed consent, all patients were enrolled in a prospective randomized protocol to receive either spinal anesthesia (SA) or general anesthesia (GA) (100 patients in each group). Randomization was carried out by opening sealed envelope at the operating theater at the day of surgery. The day before surgery, the study protocol: spinal and general anesthesia procedures were explained to each patient and all patients were instructed to describe pain on the visual analog scale (VAS) for pain. All patients received 10 mg diazepam orally at the night of surgery. On arrival of the patients to theater suite, and after routine monitoring, peripheral intravenous cannula (18G) was inserted. Lactated Ringer’s solution was infused at a rate of 8 ml/kg to replenish the overnight fasting hours. Patients of both groups were premedicated with fentanyl 1 μg/kg and midazolam 0.05 mg/kg.
All patients received intravenous 3rd generation cephalosporin, 2 h before surgery and for next 1 day thereafter.
In SA group spinal anesthesia was done by injecting 3–4 ml of heavy bupivacaine 0.5% plus 25 μg fentanyl at L3–4 intervertebral space in sitting position using 25 gauge spinal needle. Head of the bed was tilted down for 5–10 min with checking the level of anesthesia. Conscious sedation during PCNL was obtained with intravenous midazolam 1–2 mg.
In GA group induction of general anesthesia was induced with propofol 2–3 mg/kg and rocuronium 0.9 mg/kg to facilitate tracheal intubation. Anesthesia was maintained with isoflurane (1–2%) and 60% air in oxygen mixture. Controlled ventilation was achieved by (Drager-model (Primus), S. No: 5370893, Germany, 2006) ventilator to maintain end tidal carbon dioxide tension around 35 mm Hg. ECG, noninvasive blood pressure, pulse oximetry and end tidal carbon dioxide (ET CO2) was monitored throughout surgery by (Datex-Omeda model (S/5) AN. S. No: 3422715, Finland, 1998) monitor. In patients of the GA group neuromuscular block was antagonized with neostigmine 0.04 mg/kg and atropine 0.02 mg/kg at the end of surgery.
2.1 PCNL procedure
While patient was in modified lithotomy position, a 5-French open tip ureteric catheter was inserted by using 19-ch. cystoscopy. Under fluoroscopy, renal punctures were created at time of surgery in all patients by the urologist. All procedures were carried out in prone position. A 22-ch. drainage nephrostomy tubes and ureteric catheter were routinely left for 48 h after PCNL.
2.2 Measurable outcome
Pre-operative parameters included patients’ demographics, ASA status, body mass index and stone size.
Intra-operative parameters included recording of pulse, blood pressure at basal level and every 15 min till the end of procedure. Hypotension was defined when systolic blood pressure was <90 mm Hg. Bradycardia was defined when pulse <60 beat/min. Any conversion from spinal to general anesthesia was documented and the patient was excluded from the study. Operative time was calculated starting from onset of cystoscopic fixation of ureteric catheter till end of PCNL.
After patients were transferred to post-anesthesia care unit, meticulous recording of vital parameters continued every 15 min. Post-operative pain was assessed in both groups over 24 h using VAS for pain assessment. The scale consists of 10 cm horizontal line ranging from 0 (no pain) to 10 (intolerable pain). Patients were asked to mark the line vertically at a point which matched their pain [Citation7,Citation8].
VAS score was recorded by attending nurse at 15 min, 30 min, 1 h, 2 h, 4 h, 6 h, 12 h, 18 h and 24 h postoperatively. Adverse effects including nausea, vomiting, shivering or pruritus were recorded up to 24 h postoperatively. Intramuscular pethidine 50–100 mg was given when VAS ⩾ 4. The total dose of pethidine consumed by each patient was calculated. At the end of the study period, Satisfaction Visual Analog Scale system was used to evaluate patients and surgeon satisfaction in a similar manner to that used to measure pain [Citation7,Citation8]. The overall patients and surgeon satisfactions were assessed using 10 point visual analog scale (VAS) with 0 representing extremely unsatisfied and 10 representing extremely satisfied [Citation9].
2.3 Statistical analysis
The power of this clinical trial was retrospectively calculated using the G power analysis program version 3. Using post hoc power analysis with visual analog score for pain assessment as the primary objective and assuming type 1 error protection of 0.05 and an effect size convention of 0.5, a total sample size of 200 patients produced a power of 0.96. For continuous variables, data were tested for normal distribution using Kolmogorov Smirnov test. For comparison with basal levels, Wilcoxon’s signed rank test or paired-samples T test was used whenever appropriate. Mann–Whitney U test or independent-samples T test was used to compare both groups. Fisher’s exact test or Chi-square test was used to compare categorical variables. For all tests, statistical significance was considered when p < 0.05. All statistical analysis was conducted by using SPSS®, version 17 Chicago, Ilions.
3 Results
Two hundred patients, were enrolled in this study (64% males and 36% females in GA group VS 60% males and 40% females in SA group). Mean age ± SD at the time of presentation was 43 ± 11 years in GA group VS 44 ± 11 years in SA group. BMI kg/m2 for GA group was 27.4 ± 2.1 while for SA group was 27.1 ± 4.2. Mean stone burden was similar between both groups. No significant difference was found between both groups regarding patients’ demographics characteristics and mean surgery time (.).
Table 1 Patients demographics, duration of surgery and mean stone size. Values are mean ± standard deviation or number (n) and percentage.
Intra-operative heart rate and mean arterial blood pressure were comparable in both groups at the basal level, and then it continued at lower level in spinal group till 1.5 h after beginning of the procedure .
Table 2 Intra-operative changes in heart rate (beat/min) and mean arterial blood pressure (mm Hg) values are mean ± standard deviation.
VAS was lower in SA group till 1 h postoperatively in comparison with GA group (p < 0.05) . Patients in SA group started to receive analgesics after the 1st hour from the end of the surgical procedures while patients in GA group received analgesics early postoperative. Patients in GA group reported higher overall satisfaction scores than patients in SA group (mean 9.6 ± 0.4 vs. 8.6 ± 0.8, p < 0.05). Similarly, over all surgeons’ satisfaction score was higher in favor of GA group compared with SA group (10 ± 00 vs. 8.3 ± 0.4, P < 0.05) .
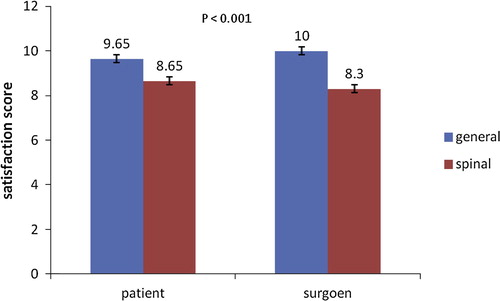
Table 3 Postoperative visual analogue scale for pain score (From 0 “no pain” to 10 “intolerable pain”) values are expressed as mean ± standard deviation.
Postoperative shivering was higher in SA group than GA group (8% vs. 2%) while nausea and vomiting was higher in GA group than SA group (5% vs. 2% and 4% vs. 1% respectively). Postoperative consumption of analgesia was significantly lower in patients in SA group in the 1st postoperative day in comparison with patients in GA group (P < 0.05) . No patients had other complications such as arrhythmia, hypotension or respiratory trouble throughout monitoring. All procedures in SA were accomplished without need to conversion to GA.
Table 4 Post-operative complications and pethidine usage (mg/day) values are expressed as (count and percentage) or mean ± standard deviation.
4 Discussion
Many studies conducted comparison between regional and GA in PCNL procedure with conflicting results. In a prospective randomized study comparing spinal epidural block vs. general anesthesia Singh et al., reported lower VAS score, less need for analgesics and shorter hospital stay in spinal epidural group [Citation5]. These superior results of spinal epidural block have been supported by other reports [Citation10]. In this study, patients in SA group recorded lower VAS score and lower consumption of analgesia postoperatively. Kuzgunbay et al. found no difference between general anesthesia and spinal epidural anesthesia regarding operative time, postoperative hemoglobin level, hospital stay, success rate and postoperative complications [Citation11]. However more patients’ satisfaction was reported with spinal epidural block [Citation1,Citation10]. Complications of GA such as vascular, pulmonary and neurological complication specially during changing patient’s position from lithotomy to prone have been reported [Citation12–Citation15]. On the other hand, SA is usually associated with hypotension resulting from sympathetic block especially during changing into prone position [Citation13,Citation16,Citation17]. In a recent retrospective study that involved 1004 patients, complications were graded and compared between GA and SA [Citation18]. The GA group had more complications according to modified Clavien classification. However, not all complications were directly related to anesthesia. In the current study, no significant difference was found between both groups regarding overall rate of postoperative complications. Shivering was reported with SA more than GA group. Meanwhile, nausea and vomiting was higher in GA. No major complications were reported in both groups.
The mean operative time in the current study, like many other reports, was higher in GA group [Citation18]. This could be reflected on higher satisfaction rates which were recorded by surgeon. The feasibility of GA to be prolonged might provide enough time to finish PCNL without burden of anesthesia end-time.
On the other hand, patients’ satisfactions were higher in GA group. This finding was contradictory to most of published studies [Citation10,Citation19] and this may be explained by patients discomfort from prolonged stay in prone position [Citation20] in SA group with awareness of a lot of noise in the operation theater. Furthermore most of the patients had wrong ideas about spinal needle consequently preferred general anesthesia to avoid spinal needle puncture.
5 Conclusions
Both GA and SA are effective and safe in PCNL. SA has fewer complications and lower consumption of analgesia postoperatively. However, GA provides more satisfaction for patients and surgeon.
Financial support
The authors declare herby that the study did not receive any form of financial support.
Conflict of interest
No conflict of interest emerged during the implementation of this work. The paper had not been presented at any congress before.
Notes
Available online 26 September 2014
References
- T.TangpaitoonC.NisoogB.LojanapiwatEfficacy and safety of percutaneous nephrolithotomy (PCNL): a prospective and randomized study comparing regional epidural anesthesia with general anesthesiaInt Braz J Urol3842012504511
- M.ElbealyD.RashwanS.A.KassimS.AbbasA comparison of the effects of epidural anesthesia, lumber paravertebral block and general anesthesia in percutaneous nephrolithotomyJ Med Sci822008170176
- R.PrakashB.B.KushwahaShashibhushanV.K.BhatiaG.ChandraB.P.SinghA comparative study of bupivacine 0.25% alone and with fentanyl or dexmedetomidine for percutaneous nephrolithotomy (PCNL) under epidural anaesthesiaIndian J Sci Res5120143946
- M.A.AttariS.A.MirhosseiniA.HonarmandM.R.SafaviSpinal anesthesia versus general anesthesia for elective lumbar spine surgery: a randomized clinical trialJ Res Med Sci1642011524529
- V.SinghR.J.SinhaS.N.SankhwarA.MalikA prospective randomized study comparing percutaneous nephrolithotomy under combined spinal-epidural anesthesia with percutaneous nephrolithotomy under general anesthesiaUrol Int872011293298
- KimSung SooLeeJeong WooYuJi HyoungSungLuck HeeChungJae YongNohChoong HeePercutaneous nephrolithotomy: comparison of the efficacies and feasibilities of regional and general anesthesiaKorean J Urol542013846850
- P.DolanM.SuttonMapping visual analogue scale health state valuations onto standard gamble and time trade-off valuesSoc Sci Med44199715191530
- A.RobinsonP.DolanA.WilliamsValuing health status using VAS and TTO: what lies behind the numbers?Soc Sci Med45199712891297
- C.G.FisherL.BelangerE.G.GoftonPostoperative randomized clinical trial comparing patient-controlled intravenous analgesia with patient controlled epidural analgesia after lumbar spinal fusionSpine2882003739743
- S.KaracalarC.Y.BilenB.SarihasanS.SarikayaSpinal-epidural anesthesia versus general anesthesia in the management of percutaneous nephrolithotripsyJ Endourol23200915911597
- B.KuzgunbayT.TuruncS.AkinP.ErgenogluA.AriboganH.OzkardesPercutaneous nephrolithotomy under general versus combined spinal-epidural anesthesiaJ Endourol23200918351838
- S.MehrabiA.Mousavi ZadehM.Akbartabar TooriF.MehrabiGeneral versus spinal anesthesia in percutaneous nephrolithotomyUrol J1012013756761
- S.MehrabiK.Karimzadeh ShiraziResults and complications of spinal anesthesia in percutaneous nephrolithotomyUrol J7120102225
- A.BasiriS.MehrabiH.KianianA.JavaherforooshzadehBlind puncture in comparison with fluoroscopic guidance in percutaneous nephrolithotomy: a randomized controlled trialUrol J420077983
- B.BorzoueiS.HabibollahM.BaharResults of percutaneous nephrolithotomy under spinal anesthesiaWorld Acad Sci Eng Technol620120520
- G.SunanaG.RahulM.NanditaM.ArtiV.SiddarthM.RajeshPercutaneous nephrolithotomy under spinal anesthesia and the efficacy of adding adjuvant clonidine to intrathecal hyperbaric bupivacaine: a comparative studyInternet J Anesthesiol3312014
- G.MovasseghiV.HassaniM.R.MohagheghR.SafaeianS.SafariM.M.ZamaniR.NabizadehComparison between spinal and general anesthesia in percutaneous nephrolithotomyAnesth Pain Med412014e13871
- T.CicekU.GonulalanR.DoganM.KosanO.IstanbulluogluM.GonenB.OzturkH.OzkardesSpinal anesthesia is an efficient and safe anesthetic method for percutaneous nephrolithotomyUrology83120145055
- M.GonenB.BasaranTubeless percutaneous nephrolithotomy: spinal versus general anesthesiaUrol J1101201412111215
- M.K.MoslemiS.H.Mousavi-BaharM.AbedinzadehThe feasibility of regional anesthesia in the percutaneous nephrolithotomy with supracostal approach and its comparison with general anesthesiaUrolithiasis4120135357
