Abstract
Background
Breast surgery is commonly performed in geriatric patients. In this age group, patients commonly suffer from comorbidities, making regional anesthesia the preferred option during surgery. Both segmental thoracic spinal anesthesia (TSA), thoracic paravertebral (TPB) and pectoral nerve (Pecs) blocks were tried successfully. This encouraged us to compare between segmental thoracic spinal anesthesia (TSA) and pectoral nerve (Pecs) block for surgeries in the thoracic region, namely breast surgery.
Methods
Forty (ASA) I–II patients aged between 40–65 years with cancer breast surgeries were enrolled in this study. In regard to anesthetic choice, patients were randomly divided into two groups, with 20 patients in each: Group A, with pectoral nerve block and group B, with thoracic spinal block. Standard monitoring in the form of mean blood pressure (MBP) and heart rate (HR) was recorded. Onset time for sensory block, time to reach peak sensory level, regression times of motor blocks and sensory blocks. Intraoperative VAS and post-operative VAS were recorded. Any postoperative complications such as bradycardia, hypotension, nausea and vomiting were assessed.
Results
The time onset of both sensory and motor blocks was compared; there was statistically significant difference between both groups (P < 0.05). T1 was the highest level of sensory block attained at 17.7 ± 1.7 and 5.5 ± 1.6 min after injection in group A, and group B respectively and the total time for block was significantly prolonged in group A (940.3 ± 17.2 min) compared to group B (315.5 ± 44.3 min) as P ⩽ 0.0001. Regression times of motor blocks and sensory blocks, were significantly prolonged in group A (994 ± 55 min, 940 ± 34 min) compared to group B (382 ± 45 min, 351 ± 35 min) as P < 0.0001.
Also, there was significant prolongation of duration of postoperative analgesia with significant reduction of total fentanyl requirement during the first 24 h postoperative in group A compared to group B.
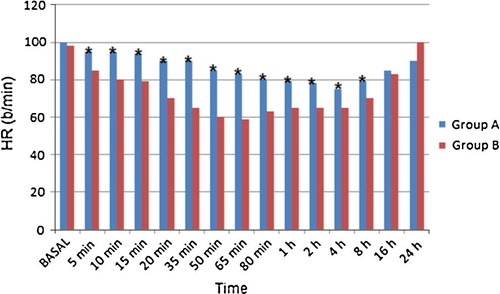
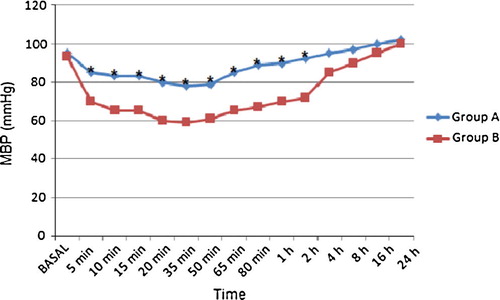
Regarding the hemodynamic variables (MBP, HR), there were significant decrease in HR and mean blood pressure (MBP) between the both groups throughout the intraoperative and early postoperative periods.
Conclusion
In conclusion, both Pecs and TSB provide effective intraoperative anesthesia and prolonged postoperative pain relief after breast surgery, but the Pecs block is technically simple and easy to learn with few contraindications, provides hemodynamic stability, and has a low complication rate and it is therefore a safe and effective technique in performing intraoperative anesthesia and controlling postoperative pain after unilateral conservative breast surgery.
Introduction
Breast cancer is the most common cancer diagnosed in Egyptian women [Citation1]. Many modalities are used in treatment of cancer breast including chemotherapy, radiotherapy and surgical intervention. The incidence of breast cancer, as well as the need of surgical treatment, has increased probably due to modern diagnostic tools. Nowadays, surgical intervention is more conservative. Surgery for management of cancer breast has many advantages in spite of its neuroendocrine, metabolic and cytokine responses that will affect the immune system according to their magnitude. Type of anesthesia used during these surgeries may augment these responses [Citation2].
General anesthesia (GA) is by far the most common utility used for breast surgeries. Different regional techniques have been tried during breast surgery, including thoracic epidural, thoracic paravertebral block, thoracic spinal block and Pecs block [Citation3].
It has been proposed that injection of local anesthetic drug into pectoral nerve could easily lead to the establishment of a block appropriate for the breast surgeries without any significant side-effects. Pectoral nerve block is a novel interfacial block technique that aims to cover the whole breast area involving the axilla and all breast nerves in the form of medial pectoral nerve and lateral pectoral nerve (Pecs I) and long thoracic nerve; thoracic-intercostal nerves from T2-T6 and thoracodorsal nerve (nerve to latissimus dorsi) (Pecs II).
It is associated with a decreased need for analgesics for controlling postoperative pain, decreased PONV, improved patient outcome, lowered postoperative pulmonary complications and, finally, decreased duration of post-anesthesia care unit (PACU) stay [Citation4].
Another type of regional anesthesia is thoracic spinal anesthesia. There are a number of advantages to deliver the spinal anesthetic directly to the required heights in the body. Firstly, one of the most obvious advantages is that there is no blockade of the lower extremities, i.e. little caudal spread. This means that a significantly large portion of the body has no venal dilation, and may offer a compensatory buffer to adverse changes in blood pressure intra-operatively. This is one of the major risks identified in surgery [Citation5]. Secondly, the dosing of the anesthetic is relatively low, giving the highly specific block to only certain nerve functions along a section of the cord. Thirdly, the degree of muscle relaxation achievable without central or peripheral respiratory or circulatory depression is superior to that with general anesthesia. In addition, the danger of cardiac arrest is much diminished. Fourthly, the patients have motor control over their legs during the surgery, which in turn means many patients exhibit a high level of satisfaction with the technique and decreased anxiety [Citation6].
Dexmedetomidine, a novel drug, is being used in anesthetic practice for its sedative, anxiolytic, and analgesic effect. It has additional advantages such as minimal respiratory depression, cardiac protection, neuroprotection and renoprotection [Citation7]. Dexmedetomidine is a highly selective α 2 adrenergic agonist; it has evolved as a choice for various applications and procedures in the perioperative and critical care settings. It is also emerging as a valuable adjunct to regional anesthesia and analgesia, where gradually evolving studies can build the evidence for its safe use in central neuraxial blocks.
The primary outcome of this study was to evaluate the efficacy of Pecs block and segmental thoracic spinal anesthesia as a sole regional anesthetic technique in female patients undergoing conservative breast surgery. The secondary outcome was comparing two blocks as regards the efficacy, intraoperative hemodynamic parameters and hemodynamic stability, duration of anesthesia, postoperative analgesia, patient satisfaction and side-effects.
Materials and methods
This controlled randomized study was carried out at Oncology Centre in Mansoura University for six months after approval of the local research and ethics committee and after obtaining written informed consent from the included patients. The study enrolled 40 female patients, ASA physical status I or II with breast lump scheduled for unilateral conservative breast surgery without axillary clearance. Exclusion criteria included age below 18 years old or more than 60 years old, obesity (body mass index (BMI) > 35), pregnancy, lactation, known allergy to bupivacaine or any contraindication to regional block (history of bleeding disorder, kyphoscoliosis, herpes zoster). Patients were randomly assigned to one of two groups 20 patients in each group by closed envelop technique. Group (A) received Pecs, and group (B) received TSB.
Preoperatively, the procedure, intended anesthetic technique and 10 cm VAS were explained to all the patients, and patients were exposed to routine preoperative evaluation, including history taking, general examination, and laboratory investigations. An 18-G intravenous cannula was inserted in the contralateral upper limb to the side of surgery, through which a 500–1000 mL of Ringer acetate solution was infused intravenously for every patient. Sedation with midazolam (2–3 mg intravenously) and pre-emptive analgesia by fentanyl 1 μg/kg were performed 15 min before the block was done.
On arrival to the operating room, routine monitors were attached (ECG, noninvasive blood pressure, and pulse oximeter). The block was performed according to the group they were assigned to.
.1 Thoracic spinal group
The patient was placed in the sitting position with the head flexed to perform the block.
The desired insertion level was determined by ultrasound guidance using a 2–5 MHz curved array probe (Sonosite M-Turbo; Sonosite Inc., Bothell, Washington, USA). The T5-T6 intervertebral level was determined on the basis of the ‘counting-up’ method from the last rib. The probe was oriented in a sagittal direction and placed at the level of the 12th rib in a parasagittal plane 2 cm from the midline. The probe was moved in cephalad direction and the ribs were counted up until the fifth rib was reached. The probe was then directed medially to identify the ligamentum flavum at the T5-T6 intervertebral space, and a skin mark was placed to identify the correct level of the block. The block was performed under complete aseptic conditions and after sterilization of the back. The skin of the puncture site was infiltrated with 2% lidocaine. The puncture was performed via paramedian approach, at the T5-T6 interspace in all patients, with a 25G cut needle (B. Braun Melsungen AG). After piercing the ligamentum flavum, the needle’s stylet was removed and the hub observed for free flow of CSF; once flow of clear CSF began, 1 ml of hyperbaric bupivacaine 0.5% in addition to 5 μg dexmedetomidine was injected.
.2 Pectoral nerve block group
Pecs block was performed while the patient in supine position with placing the ipsilateral upper limb in abduction position with a 50 mm needle (Stimuplex D, B Braun, Melsungen AG, Germany) using ultrasonic guidance after sheathing. The US probe was first placed at infraclavicular region after skin sterilization and moved laterally to locate the axillary artery and vein directly above 1st rib where pectoralis major and pectoralis minor muscles are identified at this US window. After infiltration of the skin at puncture site with 3 ml of xylocaine 2%, the needle was inserted in plane with US probe to the fascial plane between pectoralis muscles and 10 ml of bupivacaine 0.5% and 5 μg dexmedetomidine was injected to block median pectoral nerve (C8, T1) and lateral pectoral nerve (C5, C6, C7) (pec-1). Then, the US probe was moved toward axilla till serratus anterior muscle was identified above 2nd, 3rd and 4th ribs then the needle was reinserted into the fascial plane between pectoralis minor muscle and serratus anterior muscle and 20 ml of levobupivacaine 0.5% and 10 μg dexmedetomidine were injected after aspiration to block long thoracic nerve (nerve to serratus anterior), thoracic intercostal nerves from T2-T6 and thoracodorsal nerve (nerve to latissimus dorsi) (pec-2). So the patients in this group received 30 ml of 0.5% levobupivacaine and 15 μg dexmedetomidine for the purpose of this study. The sensory level was tested with pin prick and ice pack.
In both techniques the patient was placed in supine position and supplemental oxygen was administered (2–3 l/min) through a face mask or nasal cannula. Warming device (Bair Hugger; Augustine Medical Inc., Eden Praire, MN) was used to maintain normothermia.
After testing the quality of anesthesia (adequate sensory block to pin prick from the lower border of the clavicle to the inferior costal margin), the surgery was initiated. If the sensory block was inadequate after 15 min, the patient underwent general anesthesia and she was excluded from the study. Any episodes of hypotension or bradycardia were recorded. Hypotension (defined as SBP < 90 mmHg) was treated initially with ephedrine 5 mg intravenously followed by fluid bolus of 250 ml Ringer acetate solution if needed. Bradycardia (defined as HR < 50 beats/min) was treated with atropine 0.5 mg intravenously. Intraoperative anxiety was treated with midazolam 1–2 mg intravenously. Pain during the procedure was treated by fentanyl 1 μg/kg intravenous boluses. Intraoperative nausea and vomiting were treated by ondansetron 4 mg intravenously. The need for supplemental analgesics or antiemetics was recorded.
Vital signs [heart rate (HR), mean blood pressure (MBP) and oxygen saturation (SpO2)] were recorded every 5 min for 20 min and then every 15 min until the end of the procedure then at 1, 2, 4, 8, 16, and 24 h postoperatively. The upper and lower levels of sensory block were assessed by the pin-prick method 5 min after performing the block, and reassessed every 15 min until the end of the procedure. Surgery was initiated only when an adequate sensory block was achieved (at least from T2-T6). The time required to achieve this level was recorded. The maximum upper and lower sensory levels reached after 15 min were recorded. The degree of motor block in the upper and lower limbs was assessed at the same time points. The motor block in the upper limbs was assessed by the epidural scoring scale for arm movements (ESSAM) score: hand grip (T1/C8), wrist flexion (C8/C7), and elbow flexion (C6/C5); four grades (0–3) based on the number of absent movements [Citation8]. The motor block in the lower limbs was assessed by the modified Bromage scale: 0, free movement of legs and feet; 1, just able to flex knees with free movement of feet; 2, unable to flex knees but with free movement of feet; and 3, unable to move legs or feet [Citation9]. 10-cm visual analogue score (VAS) [Citation10] was assessed every 30 min intraoperative and at 1 h, 2 h, 4 h, 8 h, 16 h, and 24 h, postoperatively. General anesthesia was not used unless a satisfactory block level was not achieved by either Pecs or TSB after 15 min or if systemic analgesics did not control any intraoperative pain. Patients were advised about the possibility to convert to general anesthesia if they were dissatisfied with the block they received. Any intraoperative or postoperative complications were recorded (urinary retention, nausea, vomiting, hypotension, pleural puncture).
In the post-anesthetic care unit (PACU), the sensory level of the block was assessed every 30 min and the time until complete regression of the block was recorded. The degree of motor block was assessed at the same time points. Patients were discharged from PACU after total regression of block provided that postoperative pain was well controlled by systemic analgesics in the form of fentanyl 1 μg/kg and total analgesic requirement was calculated. Patient satisfaction was evaluated intraoperatively and after discharge from PACU at the same time of assessment of VAS and classified as totally satisfied, average satisfaction, or not satisfied. The incidence of any complications was recorded. The patients were discharged from hospital when cleared by the surgeon as complication free.
.3 Statistical analysis
The power of this clinical trial was retrospectively calculated using G power analysis program version 3 using post-hoc power analysis type II error protection of 0.05 and effect size conversion of 0.8, total sample size of 40 patients and 20 patients in each group produced a power of 0.79.
The statistical analysis of data was done by using excel program for figures and statistical Package for social Science (SPSS Inc, Chicago, IL, USA) program version 16. To test the normality of data distribution Kolmogorov–Smirnov test was done and only significant data revealed to be nonparametric. Unpaired student-t test was used for between-group comparisons of numerical variables ‘if its assumptions were fulfilled’ otherwise for nonparametric, the Mann–Whitney test was used. The description of data was done in the form of mean (±SD) for quantitative data. Any difference or change showing probability (P) less than 0.05 was considered statistically significant at confidence interval 95%.
Results
Forty female patients undergoing conservative breast surgery were recruited in this study. Patients’ demographics and duration of surgery are shown in with no statistically significant difference between the both groups.
able 1 Patients’ demographics and duration of anesthesia in the two studied groups.
All blocks were performed with ultrasonic guidance and adequate sensory level was achieved in all patients after injection of local anesthetic.
Comparing the time onset of both sensory and motor blocks in upper limb, there was statistically significant difference between both groups (P < 0.05). T1 was the highest level of sensory block attained at 17.7 ± 1.7 and 5.5 ± 1.6 min after injection in group A, and group B respectively ().
able 2 Characteristics of block in the two studied groups.
The total time for block was significantly prolonged in group A (940.3 ± 17.2 min) compared to group B (315.5 ± 44.3 min) as P ⩽ 0.0001 ().
There was no significant lower limb motor block in any of the patients, and a Bromage scale of 0 was recorded in all patients whether before or after surgery in both techniques.
Speaking about regression times of motor blocks and sensory blocks in upper limb, it was significantly prolonged in group A (994 ± 55 min, 940 ± 34 min) compared to group B (382 ± 45 min, 351 ± 35 min) as P < 0.0001 ().
Regarding the hemodynamic variables (MBP, HR), there were significant decrease in HR and mean blood pressure (MBP) between the both groups throughout the intraoperative and early postoperative periods ( and ). Arterial oxygen saturation was maintained above 97% with supplemental oxygen through face mask at 3 l/min, with none of the patients showing signs of respiratory compromise in both groups.
Both VAS throughout surgery and first 24 h postoperative and total analgesics requirement during the first 24 h postoperative were significantly decreased in group A comparing with group B ( and ).

able 3 Intraoperative and postoperative visual analogue scores in two studied groups.
Only one case (5%) developed hypotension and bradycardia in group A versus four cases (20%) of patients in second group. They showed an adequate response to the vasopressor (ephedrine 5 mg intravenous single dose) and maintained hemodynamic stability after that, and also three cases in group B developed nausea and vomiting during the event of hypotension and improved after the correction of hypotension with no need for an antiemetic. No patients developed postoperative urine retention, or problems with restoring activity postoperatively on the day of surgery.
Patients’ satisfactions were comparable in both groups, where 15 cases (75%) in group A and 14 cases (70%) in group B are satisfied.
Discussion
The pectoral nerve block (Pecs) and unilateral or conventional thoracic spinal anesthesia had been used with success, both as aesthetic and analgesic techniques, for different breast surgeries. Benefits include prolonged post-operative pain relief, a reduction of PONV and the potential for ambulatory discharge [Citation11].
This study is one of the rare studies that used Pecs block as a sole anesthetic regimen intraoperatively and it is the first to compare these two techniques in conservative breast surgeries in cancer breast.
In our study, we used levobupivacaine at concentration of 0.5% instead of 0.2% or 0.25% which is used in analgesic regimen, in addition to the usage of 15 μg dexmedetomidine which augments anesthetic effect and duration of action of local anesthetic.
The results of our study indicated that patients who were scheduled for conservative breast surgeries in cancer breast, both Pecs block and thoracic spinal block achieved adequate anesthesia and good controlling of postoperative pain but Pecs block has several crucial advantages.
Additionally, we proved that there was a significant prolongation in the onset time to achieve the desired level of block with significant prolongation of block time in Pecs (group A) versus TS (group B). On other hand VAS and total analgesic requirement were significantly reduced in group A intraoperatively and for longer time postoperatively than in group B. Also HR and BP significantly diminished in group B than in group A.
These results are in agreement with Wahba and his colleagues who randomized sixty patients undergoing elective MRM into either PVB with 10 ml of levobupivacaine 0.25% at the level of fourth thoracic vertebra or Pecs block with 10 ml of levobupivacaine 0.25% injected in between pectoralis major and pectoralis minor muscle and another 20 ml levobupivacaine 0.25% in between pectoralis minor and serratus anterior muscle. They found that Pecs block reduced postoperative morphine consumption in the first 24 and pain scores in the first 12 h in comparison with PVB after mastectomy [Citation12].
Pecs block is usually used as perioperative analgesia for breast surgery. Local anesthetic is injected between the pectoralis major (PMm) and minor (Pmm) muscles for a Pecs I block, and between the serratus anterior muscle and Pmm for a Pecs II block. Some researchers have used the Pecs block as an anesthesia technique in breast surgery of the elderly where they used 35–45 ml 0.2% ropivacaine and they concluded that Pecs block, with a sufficient volume of local anesthetic, may be a good option as anesthesia for breast surgery of the elderly [Citation13].
Regarding intraoperative vitals (HR, MAP, SpO2), we have found that there was significant decrease in HR and MBP with TS group, and our findings are in contrast with Das et al. who proved there were no significant decrease in HR or MAP with spinal anesthesia. This discrepancy between these results and ours can be explained by many causes. Firstly, Das and his colleagues did unilateral spinal block for hernial repair whose effect is minimal on hemodynamics and secondly the spinal block was performed in lumber area not thoracic which has a lesser sympathetic block with weaker effects on hemodynamics. Thirdly we used dexmedetomidine at a dose of 5 μg in thoracic spinal block which has a hypotensive and bradycardic effects [Citation14].
On the other hand, our findings are in agreement with Elakany and Abdelhamid who proved that hypotension and bradycardia were developed in 15% of cases that received segmental thoracic spinal anesthesia [Citation15].
Pectoral nerve block (Pecs) is a novel interfascial plane block which can provide analgesia after breast surgery and it is away from sympathetic supply of breast and chest area [Citation16], whereas the thoracic spinal blocks bilateral sympathetic supply to breast and chest area, and also the extent of the spread of the drugs is greater. These differences might explain the significance in the incidence of hypotension and bradycardia between the 2 groups.
In this study we performed the spinal block at the T5 level to cover the field of surgery which extends from T2 to T6 and minimizes the risk of injuring the spinal cord where it was found that the posterior dural-spinal cord distance was significantly greater at the mid-thoracic region (T5 = 5.8 ± 0.8 mm) compared with the upper (T2 = 3.9 ± 0.8 mm) and lower thoracic levels (T10 = 4.1 ± 1.0 mm) [Citation17].
Another anatomical study performed by Lee et al., showed very similar results. In their study, they performed MRI of the thoracic and lumbar spines in the supine, laterally recumbent, and sitting (head-down) positions. They found that the separation of the dura mater and spinal cord is greatest posteriorly in the middle thoracic region compared with the upper and lower thoracic levels for all three positions. We limited our selection of patients to ASA physical status I and II, aged below 60 years, BMI ⩽ 35 to minimize the sequelae of a high spinal block or any hemodynamic or respiratory complication due to block of cardioaccelerator fibers or intercostal nerves, respectively [Citation18].
Many authors confirmed that Pecs block was superior to PVB and the thoracic spinal anesthesia where it provided acceptable surgical anesthesia, maintaining good quality and long duration of postoperative analgesia where it blocks lateral pectoral nerve (C5–7) lying between pectoralis major muscle and pectoralis minor muscle and medial pectoral nerve (8–1) running under pectoralis minor muscle and both supply that muscles; spinal nerves (T2–6) running in plane between intercostal muscles and constitute lateral and anterior branches to supply chest wall and long thoracic nerve (C5–7) and thoracodorsal nerve (C6–8) which supply serratus anterior and latissimus dorsi muscle respectively. It also has a good hemodynamic stability. So it is considered as a safer and simple anesthetic and analgesic technique [Citation19].
Finally, it was found that the addition of dexmedetomidine either intrathecally or paravertebrally markedly prolonged both sensory and motor blocks, delay the first dose analgesic requirement and total analgesic requirements. These data coincide with Kim and his colleagues who added 3 μg dexmedetomidine with 6 mg of hyperbaric bupivacaine 0.5% and found longer duration of spinal block with less analgesic request and the time to the first analgesic request was longer [Citation20].
The main limitations to this study are the small number of patients included as well as the short duration of the study. Further studies with larger sample sizes are required to detect any potential disadvantages or complications associated with these blocks techniques, especially in patients with concurrent diseases.
Conclusion
In our study, Pecs and TSB provide effective intraoperative anesthesia and prolonged postoperative pain relief after breast surgery, but the Pecs block is technically simple and easy to learn with few contraindications, provides hemodynamic stability, and has a low complication rate and it is therefore a safe and effective technique in performing intraoperative anesthesia and controlling postoperative pain after unilateral conservative breast surgery.
Financial support
The authors declare herby that the study did not receive any form of financial support.
Conflict of interest
No conflict of interest emerged during the implementation of this work. The paper had not been presented at any congress before.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- Ahmed Abdelaal AhmedMahmoudHazem AbdelwahabHusseinKarimGirgisAhmed MostafaKamalThe novel use of spinal anesthesia at the mid-thoracic level: a feasibility studyEgypt J Cardiothor Anesth820142126
- A.K.ExadaktylosD.J.BuggyD.C.MoriartyE.MaschaCan anesthetic technique for primary breast cancer surgery affect recurrence or metastasis?Anesthesiology1052006660664
- A.SchnabelS.U.ReichlP.KrankeE.M.Pogatzki-ZahnEfficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trialsBr J Anaesth1052010842852
- R.BlancoT.ParrasJ.McDonnellA.Prats-GalinoSerratus plane block: a novel ultrasound-guided thoracic wall nerve blockAnaesthesia68201311071113
- R.A.LeeA.A.Van ZundertW.A.VisserL.M.LatasterThoracic combined spinal-epidural (CSE) anaesthesiaSouth Afr J Anaesth Analg1420086369
- A.A.van ZundertG.StultiensJ.J.JakimowiczD.PeekLaparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: a feasibility studyBr J Anaesth982007682686
- A.GrewalDexmedetomidine: new avenuesJ Anaesthesiol Clin Pharmacol272011297302
- E.AbdElrazekN.B.ScottA.VohraAn epidural scoring scale for arm movements (ESSAM) in patients receiving high thoracic epidural analgesia for coronary artery bypass graftingAnaesthesia54199911041119
- P.R.BromageA comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesiaActa Anaesthesiol Scand Suppl1655196569
- J.KatzR.MelzackMeasurement of painSurg Clin North Am791999231235
- R.BlancoThe ‘pecs block’: a novel technique for providing analgesia after breast surgeryAnaesthesia662011847848
- S.S.WahbaS.M.KamalThoracic paravertebral block versus pectoral nerve block for analgesia after breast surgeryEgypt J Anaesth302014129135
- G.M.BashandyD.N.AbbasPectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trialReg Anesth Pain Med4020156874
- M.S.DasS.GuptaT.R.GhoshS.R.BasuParavertebral block can be an alternative to unilateral spinal anaesthesia for inguinal hernia repairIndian J Anaesth5562011584589
- M.H.ElakanyS.A.AbdelhamidSegmental thoracic spinal has advantages over general anesthesia for breast cancer surgeryAnesth Essays Res72013390395
- R.BlancoM.FajardoT.Parras MaldonadoUltrasound description of Pecs II (modified Pecs I) novel approach to breast surgeryRev Esp Anestesiol Reanim2012
- L.E.ImbelloniM.B.QuiriciJ.R.FerrazFilhoJ.A.CordeiroThe anatomy of the thoracic spinal canal investigated with magnetic resonance imagingAnesth Analg110201014941495
- R.A.LeeA.A.van ZundertC.P.BothaL.M.LatasterThe anatomy of the thoracic spinal canal in different postures: a magnetic resonance imaging investigationReg Anesth Pain Med352010364369
- L.A.Sopena-ZubiriaL.A.Fernández-MeréC.Valdés AriasF.Muñoz GonzálezJ.Sánchez AsherasThoracic paravertebral block compared to thoracic paravertebral block plus pectoral nerve block in reconstructive breast surgeryRev Esp Anestesiol Reanim5920121217
- J.E.KimN.Y.KimH.S.LeeH.K.KilEffects of intrathecal dexmedetomidine on low-dose bupivacaine spinal anesthesia in elderly patients undergoing transurethral prostatectomyBiol Pharm Bull3662013959965
