Abstract
Objectives
Caudal analgesia is widely used in children; the aim of this trial was to evaluate the efficacy of adding nalbuphine to local anesthetic in pediatric patients undergoing hernia repair.
Patients and methods
This randomized double-blind controlled trial was done in department of anesthesia, Cairo University hospitals, and 40 patients with ASA physical status classification I–II, aged 2–7 years were enrolled in this study and randomly assigned into 2 groups; group L received caudal levobupivacaine 1 ml/kg with concentration of 0.25% and group LN received caudal 0.125% levobupivacaine with volume of 1 ml/kg plus 0.2 mg/kg nalbuphine. Pain was evaluated immediately after emergence (FLACC 0 h), after 1 h in the PACU, after 2, 3, 4, 5, 6 and 12 h by the FLACC pain score (Face, Leg, Activity, Crying, Consolability). First time of rescue analgesic, total dose of rescue analgesic and side effects were observed for 12 h.
Results
FLACC pain scores were much less in LN group compared to L group (p value < 0.001) after the second hour. The first time for postoperative analgesic requirement was significantly longer in LN group (384 ± 23.1 min) compared to L group (202.20 ± 23.42 min) (p value > 0.001). The total dose of postoperative supplementary analgesia (intravenous paracetamol infusion) in the first 12 h was significantly lower in LN group (200.5 ± 65.5 mg) in comparison with L group (355.25 ± 69.9 mg) (P < 0.05).
Conclusions
Combining caudal anesthesia using levobupivacaine and nalbuphine provided prolonged time of analgesia with no reported side effects.
Introduction
It has been demonstrated that caudal analgesia is the most common regional anesthetic block practiced in children [Citation1]. It is proved to be effective, reliable and safe; it can be used as adjunct to general anesthesia to provide perioperative analgesia in procedures below the umbilicus as herniotomy and penile surgeries [Citation2]. Application of single local anesthetic drug for caudal analgesia requires high dose but this may provoke side effects such as respiratory depression, hypotension and local anesthetic toxicity [Citation3]. So more than one agent may be used to solve this problem and help using low doses of local anesthetic. Various drugs have been used with levobupivacaine to prolong its duration of action and to decrease the side effects. Levobupivacaine, a new long-acting amide local anesthetic, is the S (−)-isomer of the racemic bupivacaine. Unlike bupivacaine, it is less toxic to the central nervous system and less likely to cause myocardial depression and fatal arrhythmias [Citation4].
Nalbuphine is a mixed κ-agonist and μ-antagonist opioid of the phenanthrene group; it is related chemically to naloxone and oxymorphone. Nalbuphine leads to activation of spinal and supraspinal opioid receptors which leads to good analgesia with minimal sedation, minimal nausea and vomiting, less respiratory depression and stable cardiovascular functions [Citation5]. Safety and efficacy of nalbuphine have been established in the clinical field [Citation6] and its safety and efficacy also established via the epidural route [Citation7].
Nalbuphine being an agonist antagonist is less likely to cause side effects such as pruritus, respiratory depression, urinary retention, excessive sedation, because of its action at kappa receptors.
The aim of this study was to compare the combination of 0.125% (1 ml/kg) levobupivacaine and nalbuphine (0.2 mg/kg) with levobupivacaine 0.25% (1 ml/kg) administered caudally in young children with hernia repair surgeries for reduction in dose of both agents and prolongation of the duration of analgesia.
It was hypothesized that the addition of nalbuphine to levobupivacaine for caudal analgesia could hasten the onset of action and could prolong the duration of analgesia.
Patients and methods
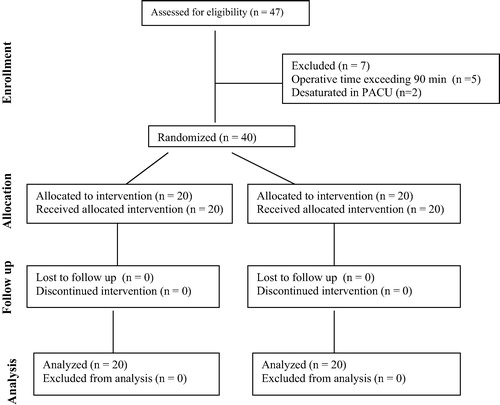
This is a prospective randomized parallel-group controlled study with allocation ratio (1:1) conducted after obtaining written informed consent from the patients’ guardians and obtaining approval from the ethical committee. A total of 40 patients aged 2–7 years, ASA physical status classification I–II undergoing elective hernia repair surgeries were enrolled. Exclusion criteria included cardiac, asthmatic patients, procedures lasting more than 90 min and allergy to any of study drugs, and shows flowchart of the participants in the study. General preoperative fasting guidelines were used. The patients were randomly assigned two groups: L and LN groups. Randomization was done using computer generated random numbers inserted into opaque concealed envelopes; inside these envelopes was a number, which indicates the group to which the patient was assigned. Anesthesia was conducted using Datex-Ohmeda anesthesia workstation (Datex-Ohmeda Aspire 7100), (GE healthcare, Little Chalfont, UK). Standard monitoring including electrocardiogram (ECG), non-invasive blood pressure (NIBP), heart rate (HR) and oxygen saturation was started preoperatively. Anesthesia was induced either with intravenous propofol 1–2 mg/kg or by inhalation of sevoflurane in oxygen. Tracheal intubation was done by using atracurium 0.5 mg/kg body weight. Anesthesia was maintained with 2% sevoflurane in oxygen. A caudal epidural block was performed immediately after induction of anesthesia under complete aseptic conditions; the anesthesiologist who performed the caudal injections took no further part in the study. Both patients and observers were blinded to the treatments. Group LN received 0.125% levobupivacaine 1 ml/kg with nalbuphine 0.2 mg/kg body weight. Group L patients received a 0.25% levobupivacaine 1 ml/kg. The total volume of mixture injected caudally was remained constant in both groups i.e. 1 ml/kg body weight with maximum volume of 20 ml and maximum dose of levobupivacaine of 2 mg/kg. No other perioperative analgesia was given. Anesthesia was discontinued when the surgery was finished; residual neuromuscular block was antagonized with neostigmine 0.05 μg/kg, given with atropine 0.02 mg/kg, and the endotracheal tube was removed after return of spontaneous breathing. At PACU pain scores were evaluated at arrival 0 h, 1, 2, 3, 4, 5, 6 and 12 h by the FLACC pain scale () [Citation8]. For postoperative pain control paracetamol intravenous infusion was given if the recorded FLACC pain score was 4 or more (with minimum 4 h time interval between successive doses of paracetamol and rescue analgesia with meperidine 0.5 mg/kg intravenously if the FLACC pain score was 4 or more within this time interval). The time to first analgesic request [which was defined as the time from extubation till the first complaint of pain (Pain Score ⩾ 4)], the total dose of paracetamol during the first 12 h and the total dose of meperidine rescue analgesic were recorded. Any episode of complication like respiratory depression, vomiting or hypotension was recorded. FLACC pain scale is a measurement used to assess pain in children between the ages of 2 months and 7 years or in individuals who are unable to communicate their pain. The scale is scored in a range of 0–10, with 0 representing no pain while 10 is the worst pain. The scale has five criteria that are each assigned a score of 0, 1, or 2.
able 1 FLACC behavioral pain assessment scale [Citation8].
The primary outcome was the postoperative pain and behavioral scores and the secondary outcome was the changes of hemodynamic variables.
Sample size: Sample size calculation was done using PS Power and Sample Size Calculations software, version 3.0.11 for MS Windows (William D. Dupont and Walton D. Vanderbilt, USA). Assuming that power analysis with α error = 0.05, β = 0.8 showed that we would need to study 15 patients in each arm to reveal a significant change in the duration of analgesia as small as 1.5 times the standard deviation. The sample size was increased by 30% (20 per arm) to account for dropouts.
Statistical analysis: Data were coded and entered using the statistical package SPSS version 22 (IBM Corporation, Armonk, New York, USA). Data were summarized using mean, standard deviation, median, minimum and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between quantitative variables were done using the nonparametric Mann–Whitney U test as the data in the 2 groups were non-normally distributed. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5, and P-values less than 0.05 were considered as statistically significant.
Results
There was no statistically significant difference between the two groups regarding demographic data (age, sex, weight, ASA physical status and duration of anesthesia) ().
able 2 Demographic data and duration of procedure.
No serious adverse effects were recorded in the first 12 h in all patients. No postoperative sedation, hallucination, nausea, vomiting, allergy or significant heart rate and blood pressure changes were reported.
Postoperative FLACC pain scores were significantly less in LN group compared to L group after the second hour and in the next time intervals (p < 0.05) ().
able 3 Postoperative FLACC pain scores.
The first time for postoperative analgesic requirement was significantly longer in LN group (384 ± 23.1 min) compared to L group (202.20 ± 23.42 min) (p value > 0.001). The total dose of postoperative supplementary analgesia (intravenous paracetamol infusion) in the first 12 h was significantly lower in LN group (200.5 ± 65.5 mg) in comparison with L group (355.25 ± 69.9 mg) (P < 0.05) (). Meperidine as a second rescue analgesic was not required by any patient in the two studied groups.
able 4 Time to 1st rescue analgesic (min) and total dose of paracetamol (mg).
Discussion
The present study demonstrated that the use of epidural nalbuphine as adjuvant to levobupivacaine for postoperative analgesia after hernia repair surgeries is safe and effective with reduced postoperative FLACC pain scores and analgesic request during the first 12 h compared to levobupivacaine alone and longer duration of postoperative analgesia. Nalbuphine is a mixed agonist–antagonist opioid which has antagonist effect at mu receptor and agonist at kappa receptors. There are few reports of neuraxial administration of nalbuphine. There are no reports of neurotoxicity of intrathecal nalbuphine since then. Intrathecal nalbuphine was used in pregnant patients, but no neurotoxicity was reported in them [Citation9]. Previous studies also have shown that epidural or intrathecal use of nalbuphine produces a significant analgesia accompanied by minimal itching and respiratory depression [Citation10].
In the present study we have used levobupivacaine with nalbuphine as an adjuvant to assess the duration of analgesia postoperatively and any side effects. After caudal block was given there was no significant difference between onset of sensory and motor block in both of the groups. There was also no significant difference between peak sensory and motor block in both groups but duration of postoperative analgesia in study group with added adjuvant nalbuphine was 6–8 h and in control group with plain levobupivacaine was 2–3 h. This is the first study to evaluate the effect of adding nalbuphine to the caudal epidural route in children.
In line with our study Shin et al. [Citation11] assessed caudal nalbuphine as a postoperative analgesic in a randomized double blind study of 80 patients after perianal surgery. Caudal block was carried out with 1.5% lidocaine; 25 ml (Group 1) in 20 patients, and mixed with nalbuphine 3 mg (Group 2) in 20 patients, nalbuphine 5 mg (Group 3) in 20 patients, and nalbuphine 10 mg (Group 4) in 20 patients. Pain relief was evaluated by the subsequent need for systemic analgesics (Pethidine). In group 4, the use of systemic analgesics was significantly reduced for the first 24 h postoperatively.
Also, in line with our study Lippmann and colleagues [Citation12] studied efficacy of epidural nalbuphine in postoperative pain control. They used 10 mg nalbuphine in 10 ml normal saline compared to 10 ml normal saline in the epidural space during postoperative period after full recovery from effect of anesthesia and at complaining of severe pain. Patients’ pain intensities were evaluated by visual analogue scale (VAS) and numbers of intramuscular analgesics needed were recorded through the 48 h observation period. They found that pain scores were significantly lower in the nalbuphine group (p-value < 0.05) (no patient in the nalbuphine group required intramuscular analgesics in the 1st 6 h, whereas 65% of the patient in the control group required analgesics), no evidence of sensory, motor or autonomic block was observed in any patient, also no pruritus or respiratory depression was noticed in any patient.
Limitation of this study was the duration of follow-up of patients as we followed them for 12 h only as surgeries were done on day case basis. In this study we used doses of nalbuphine comparable to those used for intravenous analgesic therapy. Thus our results may reflect systemic effects. We cannot conclude this with certainty, because we did not estimate blood levels of nalbuphine.
In conclusion we found that addition of nalbuphine to local anesthetic was associated with prolonged duration of analgesia and reduced analgesic requirements and no side effects were observed.
Conflict of interest
The authors declare no conflict of interest about this study.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- T.C.BrownR.L.EyresR.J.McDougallLocal and regional anaesthesia in childrenBr J Anaesth8319996577
- D.A.De BeerM.L.ThomasCaudal additives in children: solutions or problems?Br J Anaesth902003487498
- M.NagiubA.M.SharifM.SerajM.El GammalA.A.DawlatlyKetamine for caudal analgesia in children: comparison with caudal bupivacaineBr J Anaesth671991559564
- G.A.Mc leodD.BurkLevobupivacaineAnaesthesia562001331341
- E.B.De SouzaW.K.SchmidtM.J.KuharNalbuphine: an autoradiographic opioids receptor binding profile in the central nervous system of an agonist/antagonist analgesicJ Pharmacol Exp Ther2441988391402
- C.L.LakeE.N.DuckworthC.A.DiFazioC.G.DurbinM.R.MagruderCardiovascular effects of nalbuphine in patients with coronary or valvular diseaseAnesthesiology571982498503
- J.J.WangM.S.MokM.LipmannComparative analgesic efficacy of epidural nalbuphine, butorphanol, meperidine, and morphineAnesth Analg671988S248
- S.I.MerkelT.Voepel-LewisJ.R.ShayevitzThe FLACC: a behavioral scale for scoring postoperative pain in young childrenPediatr Nurse2331997293297
- T.YakshD.J.BirnbachIntrathecal nalbuphine after cesarean delivery: are we ready?Anesth Analg9132000505508
- R.FournierZ.GamulinM.MacksayE.Van GesselIntrathecal morphine versus nalbuphine for post-operative pain relief after total hip replacementAnesthesiology891998867
- J.S.ShinD.M.YoonK.M.LeeH.K.OhPostoperative analgesia by caudal nalbuphine HCLJ Kor Pain Soc3119904450
- M.S.MokM.LippmannJ.J.WangEfficacy of epidural nalbuphine in postoperative pain controlAnesthesiology613A1984