Abstract
Introduction
Fentanyl induced cough (FIC) often follows bolus fentanyl administration in 18% up to 65% of cases. Several researches have been done to reduce such side effect. Our hypothesis is that pretreatment with intravenous dexmedetomidine–magnesium sulfate could effectively suppress fentanyl induced cough.
Patients and methods
200 patients of (ASA) I and I aged 18–60 years, weighting from 40 to 90 kg, undergoing elective surgeries, were randomized into four groups using sealed envelope system. Patients belong to (D) group received DEX 0.5 μg/kg. Patients belong to group (M) received magnesium sulfate 20 mg/kg, and those of group (D + M) received DEX 0.5 μg/kg + magnesium sulfate 20 mg/kg. The above preparations were reconstructed by saline to reach a volume of 20 ml. Patients belong to group (S) received 20 ml normal saline. Patients of each group received their cross bonding drug one minute before fentanyl bolus injection (2 μg/kg within 5 s). The primary end points were the onset time, frequency and severity of cough from time of fentanyl injection till 1 min. According to four point scale, severity of cough was graded as follows: grade 0 = no cough; grade 1 = single cough; grade 2 = more than one attack of non-sustained cough; grade 3 = repeated and sustained cough with head lift.
Results
Nineteen (38%) cases had cough in group (S), 8(16%) in group (D) and 14(28%) cases in group (M). No patients in group (D + M) experienced any cough. Patients of groups (D) and (D + M) showed a significantly lower incidence of cough compared with group (S) (P < 0.05). There was no significant difference regarding the onset time or severity of cough between groups.
Conclusion
Pretreatment with dexmedetomidine–magnesium sulfate could effectively suppress fentanyl induced cough following injection of 2 μg/kg fentanyl injected within 5 s.
Introduction
Due to some sympathetic and psychological side effects that may occur during induction of general anesthesia, opioids and particularly fentanyl are used for analgesia and to relieve anxiety [Citation1,Citation2]. Fentanyl is characterized by the rapid onset, short duration, effective analgesia, less histamine release, no negative inotropic action plus it can be titrated easily [Citation3]. However, fentanyl induced cough (FIC) often follows bolus fentanyl administration in 18% up to 65% of cases [Citation4]. Several researches have been done to reduce such side effect which is a critical issue in those suffering from intracranial hypertension, cerebral or aortic aneurysm, increased intra-abdominal or intraocular pressure, pneumothorax or hyperactive air way diseases [Citation5,Citation6]. FIC may be simple or may be severe enough to cause upper air way obstruction that necessitates immediate intervention [Citation6]. Bronchoconstriction was expected to be the engine of this cough reflex, so bronchodilators (selective β2 agonist) inhalation was used. Others such as lidocaine, N-methyl-D-aspartate (NMDA) receptor antagonists, atropine, propofol, midazolam and slow administration of fentanyl were tried [Citation7,Citation8]. Dexmedetomidine (DEX) is a specific α2-receptor agonist, used to reduce anxiety and tension and to promote relaxation and sedation with hemodynamic stability [Citation9]. Magnesium (Mg) is a major cation in the human body that antagonizes calcium influx into the cell through a noncompetitive mechanism at N-methyl-D-aspartate (NMDA) receptor [Citation10] and helps to increase flaccidity [Citation11], as well; it inhibits contraction of smooth muscle and may be helpful in treatment of asthma [Citation12]. This study aims to investigate the efficacy of DEX–Mg SO4 to prevent or suppress FIC. The hypothesis of this study is that DEX–Mg SO4 complex is a powerful and effective regimen for suppression of FIC.
Patients and methods
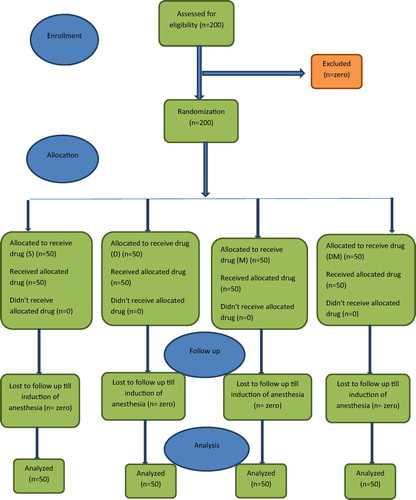
This prospective, randomized, double blind, controlled study took approval of Mansoura Medical Research Ethics Committee. The study was conducted in Mansoura University Hospital (Oncology center) and after obtaining written informed consent. 200 American Society of Anesthesiologists (ASA) physical status I and I patients with age range from 18 to 60 years and body weight from 40 to 90 kg who were undergoing general anesthesia for different elective surgeries were included in our study. Patients suffering from hyperactive airway, upper respiratory tract infection, expected difficult airway, hepatic or renal impairment, uncontrolled hypertension, coronary artery disease, and diabetes and those receiving anesthetic premedication were excluded from the study. Patients were randomly assigned to one of the four following groups using sealed envelope system: Group S (control group), Group D (DEX group), Group M (magnesium sulfate group) and Group D-M (DEX–magnesium sulfate group). I used sealed envelope system through prepared randomly generated treatment allocations within sealed envelopes. Once a patient has consented to enter the trial an envelope is opened and the patient is offered the allocated treatment regimen. The anesthetics were prepared by an anesthesiologist, who was no further involved in data collection. Patients included in this study didn’t receive any premedication before surgery. On arrival to the operating room, pressure cuff, pulse oximetry probe and ECG electrodes were connected to the patient. An intravenous access (20 G cannula) was inserted. Patients belong to (D) group received DEX 0.5 μg/kg+ normal saline to reach a volume of 20 ml. Patients belong to group (M) received magnesium sulfate 20 mg/kg+ normal saline to reach a volume of 20 ml, and those of group (S) received normal saline of 20 ml volume. Patients belong to group (D-M) received DEX 0.5 μg/kg + magnesium sulfate 20 mg/kg+ normal saline to reach a volume of 20 ml. Patients of each group received their cross bonding drug by steady rate over 10 min-one minute before fentanyl bolus injection (2 μg/kg within 5 s).
The primary end points were the onset time (time from end of bolus injection of fentanyl till beginning of cough), frequency and severity of cough. These parameters were recorded by an anesthesiologist blind to group assignment, from time of fentanyl injection till 1 min. According to four point scale, severity of cough was graded as follows: grade 0 = no cough; grade 1 = single cough; grade 2 = more than one attack of non-sustained cough; grade 3 = repeated and sustained cough with head lift. Later, by 1–2 mg propofol, anesthesia was induced and maintained with inhalational agent and/or propofol infusion plus air/oxygen mixtures.
Statistical analysis
Data were analyzed using SPSS (Statistical Package for Social Sciences) version 22.0. Qualitative data were presented as number, proportion or percentage. Comparison between groups was done by Chi-square test or Fisher’s exact test with Bonferroni correction. Quantitative data were tested for normality by Kolmogrov–Smirnov test. Normally distributed data were presented as mean ± SD. F test (ANOVA) was used to compare between groups. P ⩽ 0.05 was considered to be statistically significant.
Post hoc power analysis was done using G power program (version 3.0.10) to calculate the power of this study. Chi-square (χ2) test (contagency tables) was used with effect size = 0.3 (medium), α error = 0.05, total sample size = 200 and degree of freedom = 3. Calculated power was 0.95.
Results
No significant differences were recorded regarding the demographic data in the four groups (). Nineteen (38%) cases had cough in group (S), 8(16%) in group (D) and 14(28%) cases in group (M). No patients in group (D + M) experienced any cough. Patients of groups (D) and (D + M) showed a significantly lower incidence of cough compared with group (S). There was no significant difference regarding the onset time or severity of cough between groups (see and ).
able 1 Demographic data in four groups. Values are in means ± SD.
able 2 Incidence, the onset time and severity of cough after intravenous fentanyl administration. Values are in mean ± SD or number (%).
Discussion
Multiple mechanisms are thought to be involved in occurrence of FIC during induction of anesthesia. Fentanyl could inhibit central sympathetic outflow leading to vagal predominance, causing cough and reflex bronchoconstriction [Citation13,Citation14]. Another possible explanation is pulmonary chemo reflex as fentanyl-induced tracheal smooth muscle constriction leads to stimulation of irritant receptors in the upper pulmonary mucosa or vagal C-fiber receptors located proximal to pulmonary blood vessels [Citation15]. Also, it’s suspected that intravenous fentanyl through its action on prejunctional μ-opioid receptors leads to release of histamine and neuropeptides that contribute to coughing [Citation16].
Various studies have shed light on the potential harmful effects of FIC [Citation5,Citation17–Citation19,Citation20]. Therefore, many agents such as intra-venous ephedrine, lidocaine, dexamethasone or inhalation of sodium chromoglycate, salbutamol or beclomethasone have been tried and were documented as successful agents in suppressing FIC [Citation21].
In this study, a dose of 2 μg/kg fentanyl fits the usual daily administration in our theaters. Interestingly, this study demonstrated that a priming dose of DEX–magnesium sulfate could suppress FIC completely in comparison with 38%, 16% and 28% in placebo, DEX and magnesium sulfate groups, respectively.
None of patients in this study received premedications, and this could explain higher incidence of cough in control group (38%) compared to 16%, 28%, 0% in DEX, magnesium sulfate and DEX–magnesium sulfate groups, respectively. But the incidence of cough in our control group was lower than that was documented by Yu et al. [Citation22]. This can be attributed to a lower dose of fentanyl used in current study (2 μg/kg) compared to 3 μg/kg in the study of Yu, in addition to a slower injection of fentanyl over a duration of 5 s in this study compared to a duration of less than 2 s in the study of Yu. So, it seems wise not to inject fentanyl over duration less than 5 s.
Regarding the onset time of cough, the control group showed a shorter onset time than recorded for groups D and M but without significant difference between groups. Similarly the severity of cough didn’t carry any significant difference between these groups.
DEX is a specific α2-receptor agonist, used to reduce anxiety and tension, and to promote relaxation and sedation with hemodynamic stability [Citation9]. In the current study, DEX was used successfully in a dose of 0.5 μg/kg to suppress FIC with a significant lower incidence of cough (16%) compared to (38%) in control group.
The effectiveness of DEX in suppressing FIC was reported by He et al. using two doses (0.5 μg/kg and 1 μg/kg) [Citation23]. DEX was used successfully in combination with other agents such as midazolam and ketamine to suppress FIC [Citation4,Citation22].
Cough induced by opioid mostly is self-limited as reported by Baily [Citation2]. But Yu et al., in their pilot study reported that some patients had to restrain themselves from cough after receiving fentanyl intravenously [Citation22]. The sedative effect of DEX resembles that happen in normal sleep through inhibition of norepinephrine release from locus ceruleus that leads to stimulation of the release of GABA and galanin by ventrolateral preoptic nucleus (VLPO). These neurotransmitters cause further suppression of norepinephrine release from locus ceruleus and inhibit histamine release by tuberomamillary nucleus (TMN) leading to hypnotic state [Citation23,Citation24]. So, sedative effect of DEX not alters self-control ability of FIC. And this is an advantage for DEX if we know that midazolam in a dose of 0.06 mg/kg altered the self-control ability and can’t suppress FIC as reported by Yu et al. [Citation22].
Another explanation, in a study conducted in dogs by Groeben et al., they reported the ability of intravenous DEX to block histamine induced bronchoconstriction completely [Citation25].
On the other hand, magnesium sulfate can increase depth of anesthesia through suppression of central nervous system and can increase flaccidity by its calcium antagonist properties [Citation11]. Beside this, asthmatic patients can get benefit from magnesium sulfate through its inhibitory effect on smooth muscle contraction [Citation12].
Shideh et al. reported that magnesium sulfate in a dose of 15 mg/kg induced non-significant reduction in incidence of cough and laryngospasm in those undergoing tonsillectomy after tube removal. However incidence of cough and laryngospasm was lower than control group [Citation26].
A dose of 40 mg /kg magnesium sulfate was reported by Fuch-Buder et al. to be safe for clinical use. Either by clinical examination or by electromyography, it didn’t cause marked neuromuscular block or symptoms of muscle weakness [Citation27]. In the current study, a dose of 20 mg/kg was selected but it failed to achieve significant decrease in incidence of cough compared with control group. However, the combination of magnesium sulfate and dexmedetomidine can suppress FIC completely that can be attributed to the combined effects of both drugs as explained before.
One limitation in this study is that we select a dose of 20 mg/kg of magnesium sulfate which reduced the incidence and severity of cough compared to control group but failed to register a significant difference. So, I recommend trying higher doses of magnesium sulfate that may be more effective in controlling cough.
In conclusion, this study shows that pretreatment with dexmedetomidine–magnesium sulfate could effectively suppress fentanyl induced cough following injection of 2 μg/kg fentanyl within 5 s during induction of general anesthesia. So, this technique could be an effective alternative for attenuating FIC.
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.G.BovillP.S.SebelT.H.StanleyOpioid analgesics in anesthesia: with special reference to their use in cardiovascular anesthesiaAnesthesiology611984731755
- P.L.BailyPossible mechanism(s) of opioid induced coughingAnesthesiology901999335
- F.L.GrellR.A.RoomsFentanyl in anesthesiaAnesth Analg491970523
- AminSalehLiangbinZhangSally M.HadiWenOuyangA priming dose of intravenous ketamine-dexmedetomidine suppresses fentanyl-induced coughing: a double-blind, randomized, controlled studyUpsala J Med Sci1192014333337
- S.P.AmbeshN.SinghK.SrivastavaFentanyl induced coughing caused life-threatening airway obstruction in a patient with arteriovenous malformation of tongue and hypopharynxInt J Anesthesiol2020097
- Ji EunKimSang KeeMinYun JeongChaeYeon JuLeeBong KiMoonPharmacological and non-pharmacological prevention of fentanyl-induced cough: a meta-analysisJ Anesth2013 1695-4
- J.E.KimS.K.MinY.J.ChaeY.J.LeeB.K.MoonJ.Y.KimPharmacological and no pharmacological prevention of fentanyl-induced cough: a meta-analysisJ Anesth.282014257266
- K.C.HungC.W.ChenV.C.LinH.C.WengS.W.HsiehThe effect of pre-emptive use of minimal dose fentanyl on fentanyl-induced coughingAnesthesia65201047
- N.OhtaniK.KidaK.ShojiRecovery profiles from dexmedetomidine as a general anesthetic adjuvant in patients undergoing lower abdominal surgeryAnesth Analg1076200818711874
- S.BegonG.PickeringC.DubrayMagnesium increases morphine analgesic effect in different experimental models of painAnesthesiology962002627632
- N.GulhasM.DurmusS.DemirbilekT.TogalE.OzturkM.O.ErsoyThe use of magnesium to prevent laryngospasm after tonsillectomy and adenoidectomy: a preliminary studyPediat Anaesth13120034347
- B.H.RoweJ.A.BretzlaffC.BourdonG.W.BotaC.A.CamargoJr.Intravenous magnesium sulfate treatment for acute asthma in the emergency department: a systematic review of the literatureAnn Emerg Med3632000181190
- A.AgarwalA.AzimS.AmbeshN.BoseS.DhirajD.SahuU.SinghSalbutamol, beclomethasone or sodium chromoglycate suppress coughing induced by IV fentanylCan J Anaesth502003297300
- J.KameiY.NakanishiM.AsatoH.IkedaFentanyl enhances the excitability of rapidly adapting receptors to cause cough via the enhancement of histamine release in the airwaysCough920133
- H.BohrerF.FleischerP.WerningTussive effect of a fentanyl bolus administered through a central venous catheterAnesthesia4519901821
- Q.AiY.HuY.WangPentazocin pretreatment suppresses fentanyl-induced coughPharmacol Rep622010747750
- W.A.TweedD.DakinExplosive coughing after bolus fentanyl injectionAnesth Analg92200114421443
- A.AgarwalS.GautamS.S.NathD.GuptaU.SinghComparison of incidence and severity of cough induced by sufentanil and fentanyl: a prospective, randomized, double blind studyAnesthesia62200712301232
- J.A.LinC.C.YehM.S.LeeC.T.WuS.L.LinC.S.WongProlonged injection time and light smoking decrease the incidence of fentanyl-induced coughAnesth Analg1012005670674
- H.C.HorngC.S.WongK.N.HsiaoB.K.HuhC.P.KuoC.H.CherngPre-medication with intravenous clonidine suppresses fentanyl-induced coughActa Anaesthesiol Scand512007862865
- S.AmbeshN.SrivastavaFentanyl induced coughing caused life-threatening airway obstruction in a patient with arterio-venous malformation of tongue and hypo pharynxInt J Anesthesiol2012008
- J.YuY.LuC.DongH.ZhuR.XuPremedication with intravenous dexmedetomidine-midazolam suppresses fentanyl-induced coughIr J Med Sci2012
- J.H.RyuS.W.LeeJ.H.LeeE.H.LeeS.H.DoC.S.KimRandomized double-blind study of remifentanil and dexmedetomidine for flexible bronchoscopyBr J Anaesth1082012503511
- A.JoanaR.FlavioDexmedetomidine: current role in anesthesia and intensive careAnestesiol6212012
- H.GroebenW.MitznerR.H.BrownEffect of the alpha 2-adrenoreceptor agonist dexmedetomidine on bronchoconstriction in dogsAnesthesiology1002004359363
- S.MarzbanS.HaddadiM.R.NaghipourZ.Sayah VargB.Naderi NabiThe effect of intravenous magnesium sulfate on laryngospasm after elective adenotonsillectomy surgery in childrenAnesth Pain Med412014e15960
- T.Fuch-BuderO.H.Wilder-SmithA.BorgeatE.TassonyiInteraction of magnesium sulphate with vecuronium-induced neuromuscular blockBr J Anaesth7441995405409