Abstract
Background and aim
Local anesthesia nowadays became more popular in the ophthalmic surgery, especially in implantable collamer lens (ICL) procedure, with fewer complications and more patient satisfaction. Here we design a study to evaluate deep topical fornix nerve block (DTFNBA) versus topical anesthesia.
Methods
A double blinded randomized prospective controlled study of 107 eyes that were scheduled for implantable collamer lens procedure was included and divided randomly into two groups, group I topical anesthesia (n = 53), group II DTFNBA (n = 54). The two groups were monitored for pain and patient compliance.
Results
In group I, receiving topical anesthesia 27 patients (50.09%) reported pain, especially with implantation of the lens, tucking of the lens footplates and peripheral iridectomy that necessitated intracameral lidocaine injection. The others (n = 26) showed different grades of discomfort that was tolerated without the need for intracameral lidocaine. 40 patients (74.07%) in group II (DTFNBA), tolerated the surgery well, and slight discomfort was reported as a sensation of heaviness during the tucking of footplates. None of the patients had pain strong enough to require intracameral injection of lidocaine (p < 0.05).
Conclusions
Placing the anesthetic in the fornix makes the DTFNBA more effective and reliable block.
Keyword:
Introduction
General anesthesia (GA) recently is not the first choice in phakic intra ocular lens (p IOL) surgery, which is attributed to the short duration of the surgery, potential general anesthesia complications, increased length of hospital stay, and increasing the costs of GA. By the time traditional retro and peribulbar injections recede to newer techniques that are safer and cheaper, sub tenon’s block using a blunt needle took over due to the more safety profile [Citation1–Citation5]. Even though, still serious problems can occur especially in patients with long axial length. Deep topical fornix nerve block anesthesia (DTFNBA) and topical anesthesia gradually took over with promising and successful results, decreasing length of hospital stay and increasing patient satisfaction and fewer margins of complications [Citation6–Citation8].
Hypothetically, adding DTFNBA to topical anesthesia will augment the analgesic effect, improve surgical conditions and increase patient comfort.
In this study, we compared topical anesthesia alone with DTFNBA in patients undergoing posterior chamber phakic IOL surgery (Visian® ICL, V4B, STAAR, California, USA).
Patients and methods
110 patients candidates for elective Visian® ICL implantation surgery, were enrolled in this study after obtaining approval from the institutional ethical committee (Magrabi Hospital) and registered as NCT: 02196441 in the (http://www.clinical%20trials.gov), and all the patients signed consent after complete explanation. We were planning a study of matched sets of patients receiving the case and control treatments with 1 matched control per experimental subject. Prior data indicate that the probability of a treatment failure among controls is 0.05, and the correlation coefficient for exposure between matched experimental and control subject is 0.1. The true odds ratio for failure in experimental subjects relative to control subjects is 0.1, so we needed to study 51 experimental subjects with 1 matched control per experimental subject to be able to reject the null hypothesis that this odds ratio equals 1 with probability (power) 0.7. The probability of type I error linked with the test of this null hypothesis was 0.3. The sample size was increased to 110 patients (55 in each group) to exclude the dropout. Only those who are cooperative in understanding patients who were deemed suitable for topical and DTFNBA were included in the study. We excluded very anxious patients from the study. Group I received topical anesthetic drops and Group II received DTFNBA.
The study was planned to be randomized using a computer random number table, and double blinded for the patient and the surgeon, as the surgeon was not informed about the type of the anesthesia. A cannula was inserted into a peripheral vein and the routine monitor (Pulse, arterial blood pressure and oxygen saturation) was applied. The same surgeon (S.E.) did all the operations.
In group I, only topical anesthesia was applied with 2% tetracaine drops. In group II, after tetracaine drops instillation, DTFNBA was performed using two sponges (2 × 3 mm) soaked with 0.5% bupivacaine, applied deep in the conjunctival fornices – just before surgery-after anesthetising the conjunctiva with bupivacaine local anesthetic drops. The sponges were removed by end of procedure (). The anesthetic effect was tested by grasping the limbus with 0.12 tissue forceps.

Pain was monitored using a simple pain score (no pain = 0; that does not interfere with the surgical technique, discomfort = 1; the surgical technique is performed with difficulty, pain = 2; the surgeon is unable to continue the surgical technique) [Citation9].
A 3.20 mm temporal tunneled clear cornea incision was created, and the anterior chamber was filled with viscoelastic material (Microvisc 1%; Bohus BioTech AB). The PC pIOL (Visian ICL V4B; STAAR Surgical Inc., Monrovia, CA) was loaded into the cartridge and injected intracameral very slowly to allow controlled slow lens unfolding. An iris manipulator (Asico, LLC) was used to tuck the footplate haptics of the lens within the posterior chamber. Pupil constriction was achieved by Miostat 0.01% (Alcon, Texas, USA) intracameral injection, before peripheral iridectomy done with outcome. The viscoelastic material was then removed using the Simcoe irrigation aspirating cannula [Citation10].
We performed the pain scoring during every step of surgery: inserting a speculum, tolerance to the microscope light, 3.2 mm temporal incision of the cornea, intraocular Collamer lens insertion, tucking of ICL footplates, irrigation aspiration (I/A) of viscoelastic and peripheral iridectomy. The operative time and the pain score were recorded for every case. The duration of surgery ranged between 2 min and 43 s minimally, up to 3 min and 55 s maximally, which is considered a procedure of relatively short duration when compared to phacoemulsification surgery, for instance. For pain score 0 or 1, no further management was done. For pain score 2 at any stage, 1% plain lidocaine was injected intracamerally. Whereas analysis of categorical data was done using Chi-square test, non-parametric data were compared using the Mann–Whitney U test. A P value of <0.05 was considered statistically significant.
Results
One hundred and ten patients were originally recruited for the study. However, 2 patients in group I, and one patient in group II refused to share in the study. All the patients with the inclusion criteria (not anxious, comprehensive, agree to sign after explanation) were included (107 patients) and were randomly allocated to each group (53 in group I, and 54 in group II).
There was no statistical difference between the two groups regarding the demographic data (). In group I with patients who were receiving topical anesthesia, 27 (50.09%) of the patients, reported pain which required the use of intracameral lidocaine, especially with implantation of the lens (39.62%), tucking of ICL footplates, and peripheral iridectomy (PI) as shown in . The other 26 patients (49.05%), reported varying degrees of discomfort that was tolerated without the need for intracameral lidocaine. 40 patients (74.07%) in group 2 (DTFNBA), tolerated the surgery well, with only slight discomfort reported as a sensation of heaviness during the tucking of footplates and peripheral iridectomy. However, none of the patients in group 2 had pain strong enough to require intracameral injection of lidocaine. No postoperative pain was reported in either group, after the procedure was completed. The numbers of patients in each group, with different pain scores at each stage of surgery are shown in .
able 1 Demographic data of both the groups (M = mean, SD = standard deviation). 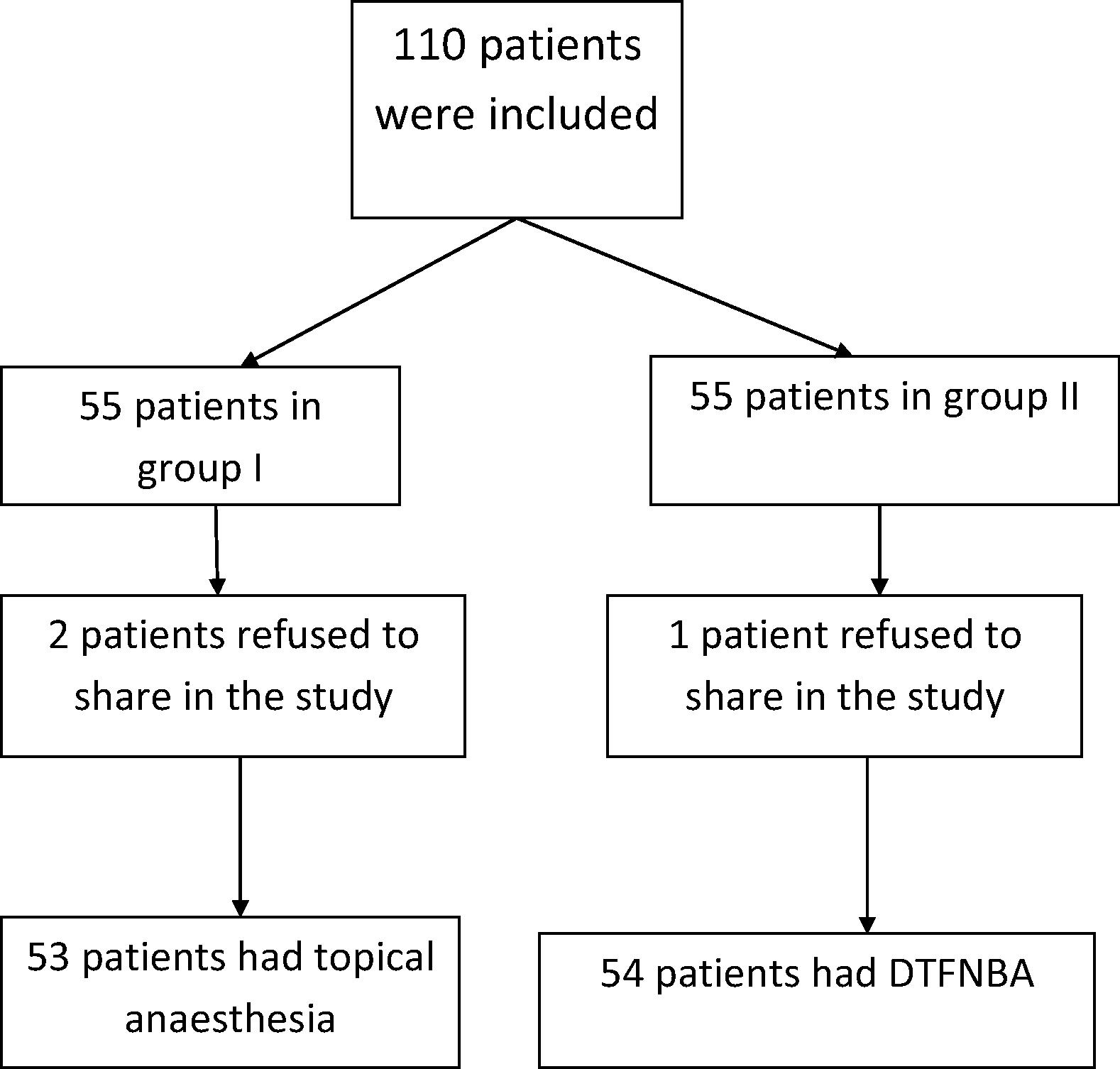
able 2 Number of patients in relation to pain score at different steps of the surgery. Chi-square test used for data analysis. ∗P < 0.0001 between groups.
Discussion
Topical anesthesia has been preferred by many surgeons because of its safety, compared to the sub-Tenon’s block and peribulbar anesthesia.
Topical anesthesia has a higher rate of patient satisfaction and immediate visual rehabilitation [Citation7]. It also has the advantage of better surgical conditions in the form of a softer globe with minimal positive vitreous pressure in comparison with the traditional retro or peribulbar blocks.
The main drawback of the topical block is that some patients squeeze orbicularis oculi muscle (squeezers). Patients cannot tolerate the microscope light and so squeeze their eyes more, limiting the surgical field, and handicapping the surgeon.
The steps of viscoelastic irrigation and aspiration, and intraocular lens insertion usually cause various grades of pain [Citation11,Citation12].
Patients did not squeeze their eyes With DTFNBA and with better tolerance to the microscope light. There were no pain and there was a slight discomfort during ICL implantation, and few patients felt discomfort or pain on the pain scale that makes DTFNBA better than topical anesthesia. Being in continuity with the peribulbar space, placing the anesthetic in the fornix, makes the DTFNBA a more effective and reliable block.
Placement of the sponges with the local anesthetic in the fornix, blocks the nerves supplying the conjunctiva. Peribulbar space absorbs the local anesthetic and blocks the posterior ciliary nerves, which supply the anterior sclera and conjunctiva as well as the iris [Citation13–Citation15].
The fornix is also a good place for direct absorption through the Tenon’s capsule, and in addition absorption into the lid which leads to some degree of lid akinesia or hypokinesia and so gives the ability to manipulate the iris freely.
In a study by Ezzat et al., most patients undergoing phacoemulsification under DTFNBA, tolerated the operation well, with only slight discomfort noted as a sensation of heaviness reported by some patients during the entry of the phacoemulsification probe intracameral and during Irrigation/aspiration. Another moment of discomfort occurred with the IOL implantation. However, none of the patients had pain strong enough to require intracameral injection of lidocaine [Citation9].
In group II where DTFNBA was used in our study, there is a better tolerance to microscope light, which suggests that nerve endings concerned with temperature sensation in the cornea are deeper in the stroma and so more difficult to block than pain fibers [Citation16], and this shows that the DTFNBA provides a deeper and profound degree of anesthesia than topical anesthetic. Bakiye et al. in 2007 concluded that deep-topical anesthesia with either ropivacaine or lidocaine in cataract surgery is safe, and the two anesthetic agents do not present differences in the degree of analgesia achieved. Deep-topical anesthesia with ropivacaine or lidocaine was equally effective in providing anesthesia with sufficient quality for cataract surgery [Citation17].
DTFNBA has many advantages, being placed at the deep conjunctival fornix and does not directly involve cornea penetration, which may reduce the risks of cornea epithelium damage or insult, due to preservative or frequent instillation of anesthesia. Compared to topical anesthesia, DTFNBA provides patient with a deeper level of anesthetic status, which may warrant a better surgical success without interruption. Compared to periocular or retrobulbar block (injection), DTFNBA is a needle free procedure, thus less painful and more acceptable to patients, especially those who seek for an elective simple vision correction; ICL. Of note, general anesthesia, due to systemic cardiovascular side effects, is becoming out of fashion in anterior segment intraocular procedures, such as a quick Phacoemulsification and IOL implantation (less than 10 min), and Visian® ICL procedure, which only involves minimal tissue manipulation.
To conclude, DTFNBA proved to be a safe, effective and non-invasive anesthesia in Phakic posterior chamber IOL implantation procedure, with tolerated intraoperative discomfort and no postoperative pain.
One of the limitations of the study is the relative short time spent in ICL implantation surgery, which does not reflect the duration of anesthetic effect of DTFNBA. Future studies may assess DTFNBA in more prolonged procedures such as deep sclerectomy, or iris-claw lens implantation using both ropivacaine and lidocaine. To our knowledge, this is the first study to assess ICL implantation under DTFNBA vs topical anesthesia alone.
Conflict of interest
The author declares that they have no conflict of interest.
The participation of the authors
More details:
| . | Hassan: sharing in the design data, data analysis, and interpretation, writing the draft, revising and final approval. | ||||
| . | Sherif: sharing in the design data (main designer), collecting (surgery, data collection, patient follow up), data analysis and interpretation, revising and final approval. | ||||
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.P.BarkerP.N.RobinsonG.C.VafidisG.R.HartS.Spased-BymeG.M.HallLocal analgesia prevents the cortisol and glycaemic responses to cataract surgeryBr J Anaesth641990442445
- J.D.StevensA new local anaesthesia technique for cataract extraction by one quadrant subtenons infiltrationBr J Ophthalmol761992670674
- L.BergmanL.BerglinP.V.AlgreveLimbal subtenons administration of retrobulbar anesthesia using a blunt irrigating cannulaOphthalmic Surg Lasers271996106112
- Z.KapranM.UyarK.EltutarOne quadrant sub-tenons capsule anesthesia in anterior segment surgeryEur J Ophthalmol61996131136
- B.-K.KhooT.-H.LimV.YongSubtenon versus retrobulbar anaesthesia for cataract surgeryOphthalmic Surg Lasers271996773777
- R.A.FichmanTopical anaesthesiavol. 111998Ophthalmic Clinics of North America pp. 57–63
- S.C.DinsmoreDrop, then decide approach to topical anaesthesiaJ Cataract Refract Surg211995666671
- I.G.M.DuguidC.M.P.ClaoueY.Thamby-RajahTopical anaesthesia for phacoemulsification surgeryEye91995456459
- S.Aziz EzzatK.NohaProspective evaluation of deep topical fornix nerve block versus topical anaesthesia in patients undergoing phacoemulsification and intraocular lens implantationJ Br Ophthal Anaesth Soc20094449
- ICL technique: Assetto V, Benedetti S, Pesando P. Collamer intraocular contact lens to correct high myopia. J Cataract Refract Surg 1996;22:551–556.09;44–49.
- K.GombosE.JakubovitsA.KolosG.SalaczJ.NémethCataract surgery anaesthesia: is topical anaesthesia really better than retrobulbarActa Ophthalmol Scand852007309316
- M.B.SosisTopical anaesthesia is the technique of choice for routine cataract surgeryAnesthesiology1002004197
- Hustead RF, Kornneef, Zonneveld FW. Anatomy. In: Gills JP, Hustead RF, Sanders DR, editors. Ophthalmic anaesthesia. Thorofare, NJ, Slack; 1993. 63.
- Srinivasan BD, Jakobeic FA, Iwamoto T. Conjunctival. In: Duane TD, Jaeger EA, editors. Biomedical foundations of ophthalmology, vol. 1. Philadelphia: Harper and Row; 1985 [chapter 29:23].
- M.J.ReechThe globeL.T.JonesM.J.ReechJ.D.WirtschafterOphthalmic ANATOMY: A MANUAL WITH SOME CLINICAL APPLICATIONS1970American Academy of Ophthalmology and OtolaryngologyRochester (MN)105149
- S.C.MillerK.J.HimmelsteinT.F.PattonA physiological based pharmacokinetic model for the intraocular distribution of pilocarpine in rabbitsJ Pharmacokinetic Biopharm91981653667
- U.BakiyeO.SemaO.MustafaG.ErdalO.FatihG.FerayRopivacaine versus lidocaine for deep-topical, nerve-block anaesthesia in cataract surgery: a double-blind randomized clinical trialClin Exp Ophthalmol352007148151
