Abstract
Background
This study evaluated the efficacy of transdermal fentanyl (TDF) delivery system (50 μg/h) or transdermal melatonin (TDM) delivery system (7 mg) 2 h preoperatively for acute postoperative pain after lumbar laminectomy compared to placebo group (C).
Methods
Seventy-five patients of both sexes, aged 18–50 years, ASA I and II undergoing elective single level lumber laminectomy under general anesthesia were included in this randomized controlled double-blind study. Patients were randomly divided into 3 groups 25 each, C group patients received transdermal placebo patch, TDF group (50 μg/h) and TDM group (7 mg). Assessment of postoperative pain, sedation, hemodynamic variables such as HR and MAP, postoperative monitoring of arterial SpO2 and side effects (e.g. nausea, vomiting, pruritis, respiratory depression and hemodynamic instability) was done 30 min, 1, 2, 6 and 12 h postoperatively. Postoperative Patient‘s and Surgeons‘ satisfaction, Intraoperative bleeding and plasma cortisol (μg/dl) postoperatively were also assessed.
Results
There was a significant reduction in the VAS score, total pethidine requirements and significantly higher Patient‘s satisfaction in TDF and TDM groups when compared with the C group 6 h postoperatively. The sedation score and Surgeons‘ satisfaction were significantly higher associated with a significant decrease in MAP and Intraoperative bleeding in TDM group compared to groups C and TDF 6 h postoperatively. Significant nausea and vomiting in TDF group and significant sedation in TDM group were recorded.
Conclusion
The use of preoperative TDF 50 μg/h or TDM 7 mg was an effective and a safe adjuvant for acute pain after surgery.
Introduction
“Freedom from pain should be a basic human right, limited only by our knowledge to achieve it” [Citation1]. Central sensitization and hyperexcitability develop after the surgical incision resulting in amplification of postoperative pain [Citation2]. Kissin introduced the term ‘preventive analgesia’ to emphasize the fact that central sensitization is induced by noxious preoperative and postoperative inputs [Citation3,Citation4]. McCaffery and Ferrell showed that over 50% of surgical patients experienced inadequate pain relief following surgery with negative physiological and psychological consequences [Citation5]. Surgical injury elicits a well‐known stress response involving activation of inflammatory, endocrine, metabolic and immunologic mediators [Citation6]. Preventing the establishment of altered central processing by analgesic treatment may result in short-term (e.g., reduction in postoperative pain and accelerated recovery) and long-term (e.g., reduction in chronic pain and improvement in health related quality of life) benefits during a patient’s convalescence [Citation2]. These concepts suggest a possible study design; effective analgesia starts before incision and covers both the period of surgery and the postoperative period.
Transdermal drug delivery offers the potential benefits of simplicity, efficacy and patient acceptance. In theory, a transdermal delivery system can provide a stable serum concentration for an extended period of time with acceptable interpatients variability [Citation7].
Fentanyl citrate is a potent synthetic narcotic with physicochemical characteristics that are suitable for rate controlled transdermal delivery. These characteristics include high potency, skin compatibility, low molecular weight, and appropriate solubility [Citation8]. Transdermal delivery system for fentanyl (TDF) has been developed and approved for the treatment of cancer and chronic pain and it has been demonstrated that transdermal fentanyl provides effective analgesia for acute postoperative pain. TDF does not require I.V. access and the risk of infection is decreased [Citation9]. Fentanyl patches are designed to deliver fentanyl at four constant rates: 25, 50, 75, and 100 μg/h for a period of 72 h. The steady-state serum concentration is reached after 24 h and maintained as long as the patch is renewed [Citation10]. The choice of the transdermal delivery system of fentanyl with a predicted delivery rate of 50 μg/h was based on a previous study characterizing the relationship between serum fentanyl concentrations and analgesic effects in patients undergoing abdominal surgery. Some studies demonstrated a non-significant reduction in opioid requirements using delivery rates of 25 μg/h [Citation11–Citation14]. On the other hand, up to 9% of patients were at risk of respiratory depression when being treated with TDF 75 μg/h (administered 8 h prior to surgery) [Citation14]. For management of postoperative pain, it may be desirable to apply transdermal fentanyl several hours before completion of surgery so that minimal effective concentration (MEC) can be achieved prior to or concomitant with the end of surgery [Citation15].
Melatonin (N-acetyl-5-methoxytryptamine, MT) is a hormone secreted primarily by the pineal gland in a circadian fashion. The synthesis and secretion of MT is induced by darkness and suppressed by light through retinal nerve fibers projecting to the suprachiasmatic nucleus of hypothalamus, then to the superior cervical ganglion and finally to the pineal gland. During the night, the mean endogenous plasma concentration of MT is ∼50–70 pg/mL (216–302 pmol/L) in young adults. In daylight hours, the mean MT plasma concentration is typically <10 pg/mL (43 pmol/L). Plasma MT levels typically begin to increase at ∼2100 h, peak between 0200 and 0400 h, and return to baseline at 0700–0900 h [Citation16]. MT has a short plasma elimination half-life, ∼45 min, and, when administered orally, shows low and variable bioavailability, presumably due to extensive first-pass metabolism and/or variable absorption [Citation17]. Transdermal delivery system for melatonin (TDM) results in sustained plasma MT levels that can be tailored to the normal physiological range and avoid the first-pass metabolism. TDM is intended to be worn for 8 h [Citation18]. Melatonin has sedative, anxiolytic, analgesic, antihypertensive, anti‐inflammatory, chronobiotic and oncostatic effects and potent antioxidant properties [Citation19]. Melatonin exerts its analgesic effects through augmentation of GABA-ergic systems and morphine anti-nociception, enhancing GABA-induced currents and inhibiting glycine effects [Citation20]. Melatonin may enhance the levels of β-endorphins and the anti-nociception induced by delta opioid receptor agonists and could activate MT2 melatonin receptors in the dorsal horn of the spinal cord [Citation21,Citation22].
Spine surgery may range from minimal invasive discectomy surgery to extended scoliosis fusion. Both an anterior approach and posterior approach are possible. The most commonly used technique to anesthetize patients scheduled for thoracic or lumbar spine surgery is general anesthesia followed by conventional pain therapy [Citation23]. Controlling the hemodynamic situation of patients who have spinal operation is of prime importance and maintaining the heart rate and blood pressure in normal or low-normal levels in these patients can reduce bleeding in the surgical field, particularly in congested, small and limited areas such as spine [Citation24].
Surgical trauma elicits endocrine and metabolic changes characterized by an increase in the secretion of catecholamines. Pain and other afferent neurogenic stimuli from the site of the operation are known to play a dominant role in this mechanism [Citation25,Citation26]. The stress response to surgery is characterized by increased secretion of pituitary hormones and activation of the sympathetic nervous system. The changes in the pituitary secretions have secondary effects on hormone secretion from target organs (increased secretion of cortisol from the adrenal cortex) [Citation27].
In this randomized, double-blind, placebo-controlled study, our primary goal was to compare the transdermal fentanyl patches to transdermal melatonin patches for relieving postoperative pain after single level lumber laminectomy under general anesthesia to detect a mean difference of total analgesic (pethidine) consumption. And our secondary goal was to compare the effects of the transdermal fentanyl patches to transdermal melatonin patches on prolongation of first analgesic requirement time, pain score, sedation score, stress response, patient satisfactory score, surgeon satisfactory score, postoperative monitoring of heart rate, mean arterial blood pressure, arterial SpO2 and side effects (e.g. nausea, vomiting, pruritis, respiratory depression and hemodynamic instability).
Methods
This study was designed to be a randomized, placebo-controlled, double-blind parallel study in which the patients, investigators, anesthesiologists and the surgeons were blinded to the given treatment. This study was conducted in Ain-Shams University Hospitals, from March 2013 to April 2015 on 75 patients aged between 18 and 50 years of both sexes of ASA physical status I and II of 70–90 kg body weight and height 160–180 cm undergoing elective single level lumber laminectomy under general anesthesia. The study protocol was approved by the institutional ethical committee and written informed consent was obtained from all the patients.
Patients with impaired kidney or liver functions, history of cardiac or central nervous system disease, history of drug or alcohol abuse, history of chronic pain or daily intake of analgesics, uncontrolled medical disease (diabetes mellitus and hypertension), history of intake of non-steroidal anti-inflammatory drugs or opioids within 24 h before surgery or allergy to the used medications, coagulation defect, local infection at the site of application of transdermal patch, patient refusal or duration of surgery more than 120 min were excluded from the study.
Patients were randomly divided into 3 groups, C group, (n = 25) each patient received transdermal placebo patch, TDF group, (n = 25) each patient received transdermal therapeutic system-fentanyl 50 μg/h and TDM group, (n = 25) each patient received transdermal therapeutic system containing 7 mg of melatonin. Randomization was done using computer-generated number table of random numbers in a 1:1 ratio and conducted using sequentially numbered, opaque and sealed envelope (SNOSE). All patches were placed 2 h preoperatively and were applied to the skin in the subclavicular area and the area was not shaved to maintain the integrity of the skin to maintain normal absorption (if necessary hair was only clipped from the patch site prior to application). The patch was removed 12 h postoperatively. In this study we used identical placebo patches assembled by the hospital pharmacy, and we used fentanyl patches [Durogesic® D-Trans® (matrix) from Janssen-Cilag] with delivery rate of 50 μg/h patch and we used melatonin sleep patch from Respro Labs™ containing 7 mg of melatonin. Active patches containing fentanyl or melatonin were indistinguishable from placebo patches, covered with adhesive plaster to confirm fixation and to blind the anesthetists and observers for the type of the used patches. The study drugs were prepared by the anesthesia resident not involved in any other part of the study.
Before any patch placement a preoperative visit was done to all patients to assess patient fitness for operation, to alleviate anxiety, to inform them about transdermal patches (its efficacy in the treatment of postoperative pain, its possible side effects and method of application) and to make them familiarized with 10 cm marked visual analog scale (VAS) for postoperative assessment of pain, where 0 cm defines no pain and 10 cm defines the maximum intolerable pain. The patients were also assured that they would receive intramuscular injection (IM) of pethidine 0.5 mg/kg once they start to first experience pain postoperatively (Patients with VAS > 3). Time to the first request for analgesic and the total pethidine consumption were recorded 12 h postoperatively.
The general anesthesia technique was standardized for all the patients as well as monitored including 5 lead ECG, non-invasive blood pressure (NIBP) monitor, pulse oximetry and capnography after intubation using Datascope monitors. Neuromuscular function was also monitored using a peripheral nerve stimulator. After establishing an intravenous (IV) line, induction of general anesthesia with fentanyl (2 μg/kg) and sleeping dose of propofol followed by rocuronium (0.6 mg/kg) to facilitate orotracheal intubation was done. Anesthesia was maintained using sevoflurane in oxygen and air. Granisetron (1 mg IV) was given as a prophylactic antiemetic. At the end of the surgery, the residual neuromuscular paralysis was antagonized with neostigmine (0.05 mg/kg) and atropine (0.01 mg/kg). After satisfactory recovery, patients were extubated and transferred to the post-anesthesia care unit (PACU) where they were monitored with ECG, NIBP and pulse oximetry.
Assessment of postoperative pain, sedation, hemodynamic variables such as heart rate (HR) and mean arterial pressure (MAP), postoperative monitoring of arterial SpO2 and side effects (e.g. nausea, vomiting, pruritis, respiratory depression and hemodynamic instability) were done 30 min, 1, 2, 6 and 12 h postoperatively.
Postoperative pain was evaluated based on visual analog scale, first time to ask for rescue analgesia and total pethidine requirements in 12 h (mg) postoperatively were also recorded. Assessment of sedation was according to sedation score (Ramsay sedation score) [Citation28] (see ).
able 1 Ramsay sedation score.
Hypotension was considered if there was 20% decrease below the baseline for mean arterial blood pressure, and it was treated with intravenous ephedrine (3–6 mg IV bolus). Bradycardia (heart rate <55 beats/min) was treated with intravenous atropine (0.6–1 mg). If there was a decrease in arterial SpO2 (<90%), it was treated with oxygen through a transparent face mask. Severe nausea or vomiting was treated with dexamethasone 5 mg and severe pruritus was treated with clemastine (Tavegyl®) 2 mg/ampoule i.v. as required. If any of the patients developed respiratory depression, the transdermal patch was removed and intermittent doses of naloxone 40 mg i.v. were administered.
Patient‘s satisfaction was done by asking the patient to answer the question, ‘How would you rate your experience after the surgery?’ using a 7-point Likert verbal rating scale () [Citation29]. Surgeons were also asked to rate their satisfaction with operative conditions, using the 7-point Likert verbal rating scale at the end of surgery, acceptable satisfaction score of both the patient and surgeon being 5–7. Intraoperative bleeding was assessed by bleeding scale (0–5) () [Citation30], acceptable bleeding score being 0–2.
able 2 Intraoperative bleeding score classification.
Hormonal stress response was assessed through recording plasma cortisol (micrograms/dl) 2 h postoperatively. Serum cortisol was measured by a Fluorescence Polarization Immunoassay (FPIA) Technology by the Abbott AXSYM system with the following reference ranges (morning serum cortisol 4.2–38.4 μg/dl and evening serum cortisol 1.7–16.6 μg/dl).
.1 Analysis of data
Using PASS 13 for sample size calculation, in a one-way ANOVA study it was calculated that a sample size of 22 patients per group will achieve 80% power to detect a mean difference of 50 mg in total Pethidine consumption with a SD of 25 between the three groups using an F test with a 0.05 significance level. 25 patients per group were intended to be included to replace any dropouts.
Data were analyzed using SPSS 18.0 for Windows (SPSS, Chicago, IL, USA). Analysis of variance was used to compare quantitative parametric data with Tukey’s test as a post hoc test. Kruskal–Wallis test was used for quantitative nonparametric data. Chi square test was used for comparison of qualitative data. Continuous parametric data were presented as mean ± SD, non-parametric data as median (IQR) and categorical data as number of patients. P-values of <0.05 were considered statistically significant.
Results
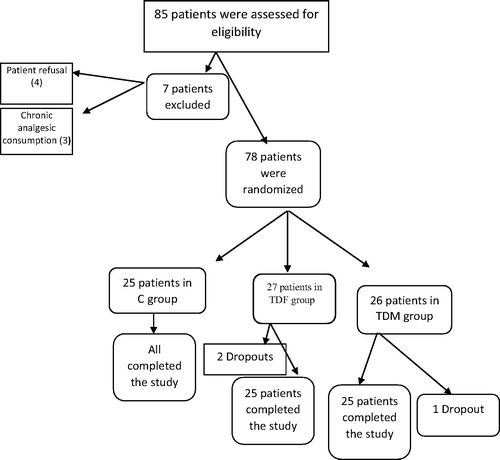
A total of 85 patients were assessed for eligibility from March 2013 to April 2015 (), out of which 78 patients received study medication after randomization, 75 patients completed the study (25 patients for each group) and their data were included in the final analysis (). Seven patients were not included in this study on account of patient’s refusal (4 patients) and history of chronic analgesic consumption (3 patients). Three patients were considered as dropouts after initial randomization and were therefore not subjected to further statistical analysis (three patients needed re-exploration on account of the postoperative bleed).
Results of the current study did not show significant difference in the demographic data of the groups of patients regarding age, sex (male to female ratio), body weight, height, ASA physical status and the length of surgery in minutes as shown in .
able 3 The demographic data.
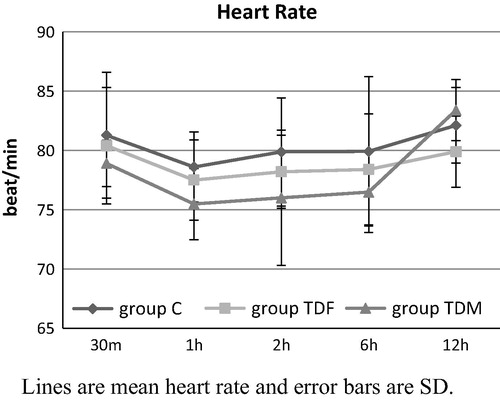
No significant differences in HR between the three groups were recorded at any time. There were lower recorded values in the mean heart rate in the TDF and the TDM groups compared to C group, 30 min, 1 h, 2 h and 6 h postoperatively and this was not significant. There was a decrease in the mean heart rate in the TDF group compared to the C and the TDM groups, 12 h postoperatively and this was not significant as shown in .
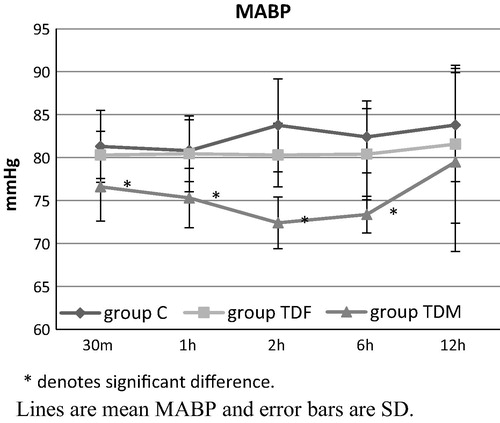
There was a significant decrease in the mean arterial blood pressure in the TDM group compared to the C and the TDF groups, 30 min, 1 h, 2 h and 6 h postoperatively as shown in .
No significant changes were noted in the SpO2 between the studied groups throughout the study period (P > 0.05).
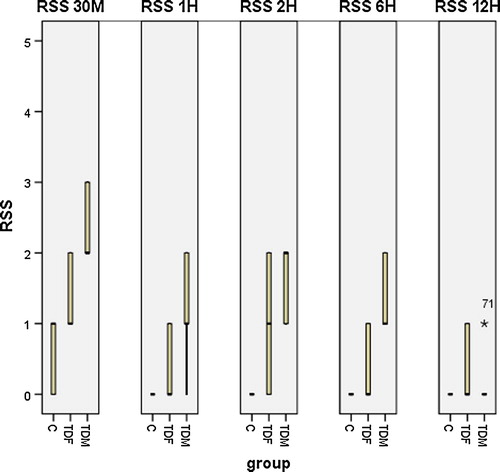
The sedation score was significantly higher in TDM group compared to the C and the TDF groups, 30 min, 1, 2, and 6 h postoperatively as shown in .
The middle black solid line represents the median RSS score, and the upper and lower margins of the boxes are IQR and the whiskers are minimum and maximum.
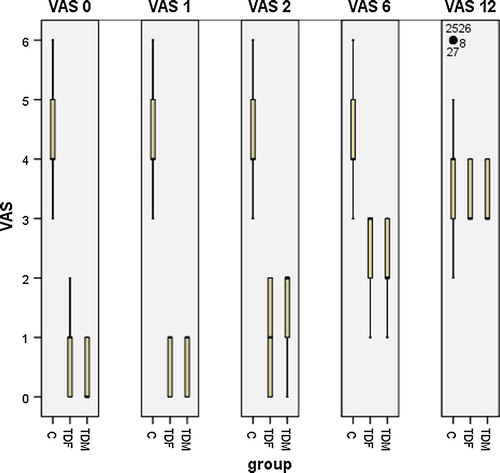
There were significant lower recorded values in visual analog scale in the TDF group and TDM group in comparison with C group, 30 min, 1, 2 and 6 h postoperatively. Pain score was lower in the TDF group compared to the C and the TDM groups, 12 h postoperatively and this was not significant as shown in .
The middle black solid line represents the median VAS score, the upper and lower margins of the boxes are IQR and the whiskers are minimum and maximum.
Regarding side effects in our study, all cases of the 3 groups were hemodynamically stable, no patient developed hypoxia and there were no reported intraoperative complications interfering with the course of surgery or interrupting the surgeons. Two patients in the C group suffered from nausea (p = 0.08). In the TDF group, nausea and vomiting occurred only in 25% of cases (n = 6/25) (p = 0.01) in spite of the fact that preoperative granisetron (1 mg IV) was given as a prophylactic antiemetic and there were no reported cases of erythema, respiratory depression or pruritus. In the TDM group, two patients were dizzy (p = 0.08).
There was significant difference postoperatively between the TDF and the TDM groups in comparison with C group as regards the time for 1st rescue analgesic (minutes) postop, the total pethidine requirements (mg) 12 h postop, the serum cortisol (μg/dl) 2 h postop and the patient‘s satisfaction score. Intraoperative bleeding measured by bleeding scale was statistically significantly less in the TDM group than in the C and the TDF groups. The surgeon‘s satisfaction score was significantly higher in the TDM group compared to the C and the TDF groups as shown in .
able 4 Postoperative data.
Discussion
In the present study, there was an overall significant reduction in the VAS score in the TDF and TDM groups when compared with the C group in the 1st 6 h postoperatively. Even in the next 6 h where there was no significant reduction of the VAS, it was still lower in the TDF group than the C and TDM groups. This reduction in the VAS score was associated with significant delay in the postoperative time for 1st rescue analgesic (minutes), significant reduction in the postoperative total pethidine requirements (mg) 12 h postoperatively, significant reduction in the 2 h postoperative serum cortisol (μg/dl) and the significant increase in the postoperative patient‘s satisfaction score as compared with the group C.
Also, this study revealed that the sedation score was significantly higher in the TDM group compared to the C and the TDF groups, 30 min, 1, 2, and 6 h postoperatively.
These results are in agreement with the findings of Radwan et al. (2010) who reported that pre-emptive oral dose of 6 mg of melatonin reduced the pain scores and pethidine requirements in the first postoperative 24 h in patients undergoing abdominal surgery [Citation31].
Borazaa et al. (2010) also reported that preoperative oral melatonin 6 mg, the night before and 1 h before surgery, decreased pain scores and tramadol consumption and enhanced sleep quality and sedation scores during the postoperative period in patients undergoing elective prostatectomy [Citation32].
These results were consistent with Caumo et al. (2010) who found that 5 mg oral melatonin, the night before and 1 h before surgery in patients undergoing abdominal hysterectomy, decreased pain and anxiety during the first 24 h after surgery [Citation33].
These results are in agreement with the findings of Sevarino et al. (1992), who compared TDF in two different delivery rates 25 μg/h and 50 μg/h with placebo for postoperative analgesia after abdominal gynecologic surgery (the patches were applied one hour before surgery and removed after 72 h) and found that there was only a significant reduction in the rescue analgesia in the TDF group with a delivery rate of 50 μg/h [Citation13].
Our results were consistent with the findings of Kilbride et al. (1994), who compared TDF with delivery rate of 50 μg/h applied six hours before surgery and removed after 72 h with placebo for the management of post-hemorrhoidectomy pain and found that there was significant reduction in the pain intensity and rescue analgesia in the TDF group when compared with the placebo group [Citation34].
These results were partially consistent with the findings of Sandler et al. (1994), who compared TDF in two different delivery rates 50 μg/h and 75 μg/h with placebo for postoperative analgesia after abdominal hysterectomy (the patch was applied two hours before surgery and removed after 72 h) and found that there was significant reduction in the pain intensity and rescue analgesia in the TDF group with delivery rate of 75 μg/h when compared with the placebo group while in the TDF group with delivery rate of 50 μg/h there was only a significant reduction in rescue analgesic consumption when compared with the placebo group [Citation35].
Our results were supported with the findings of Siafaka et al. (2004), who studied pharmacokinetic profile and efficacy of a transdermal fentanyl delivery system 50 μg/h for Acute Postoperative Pain after Intra-abdominal Gynecologic Surgery for Cancer and found that Transdermal fentanyl provided effective analgesia for acute postoperative pain and the VAS pain scores were consistently better in the fentanyl group compared with the placebo group; a better indication of the efficacy of fentanyl was the significant 50–65% reduction in the requirement for bupivacaine among these patients compared with the placebo group (pain control was supplemented with a nonopioid drug, bupivacaine 0.125–0.25%, administered through an epidural catheter via patient-controlled epidural analgesia) [Citation9].
These results are in agreement with the findings of Minville et al. (2008), who compared the preoperative transdermal fentanyl patch (TFP) 50 μg/h applied approximately 10 h before induction of general anesthesia for the postoperative pain management of patients undergoing primary total hip arthroplasty with patient-controlled analgesia (PCA) and found that Preoperative TFP application decreases pain scores and morphine consumption in the postanesthesia care unit (PACU) [Citation36].
Our results were supported with the findings of Lauretti et al. (2009), who reported that TDF 25 μg/h placed 10 h preoperatively and removed 24 h later combined with IV ketoprofen was effective in controlling postoperative pain after posterior laminectomy [Citation37].
These results are in agreement with the findings of Barrera et al. (2009), who concluded that transdermal fentanyl provided effective postoperative analgesia and reduced analgesic consumption in patients undergoing dorsal and lumbar spine arthrodesis [Citation38].
Our results were supported with the findings of Amr et al. (2012) who found that there was significant reduction in the VAS scores and rescue analgesia in the TDF group with a delivery rate of 50 μg/h when compared with the placebo group during transdermal administration of fentanyl 50 μg/h 10 h preoperatively for postoperative pain relief after major abdominal surgery. Sedation occurred only in the 1st 8 h postoperatively and it was only in the form of drowsiness that was resolved spontaneously [Citation39].
These results were supported by the study of Ismail and Mowafi (2009) who concluded that oral melatonin premedication (10 mg tablet) for patients undergoing cataract surgery under topical anesthesia provided anxiolytic effects, enhanced analgesia and decreased IOP resulting in good operating conditions (22).
These results were partially consistent with Khezri and Merate (2013) who reported that sublingual melatonin 3 mg premedication (60 min before surgery) for patients undergoing cataract surgery under topical anesthesia reduced the anxiety scores in patients and they could not demonstrate that melatonin has a decreasing effect on pain scores [Citation40].
The significant increase in the postoperative patient’s satisfaction score in TDM group as compared with group C could be a consequence of melatonin’s effects on pain and anxiety which enhance sleep wake cycle disruption in stressful situations such as surgeries, providing better recovery quality [Citation32]. Clinical trials on the effect of melatonin on delirium in hip fracture patients are going on. Melatonin has been used successfully to treat and prevent post-operative delirium [Citation40].
No significant differences in HR between the three groups were recorded at any time. There was a significant decrease in the mean arterial blood pressure in the TDM group compared to the C and the TDF groups, 30 min, 1 h, 2 h and 6 h postoperatively.
These results were supported by the study of Ismail and Mowafi (2009) who found that the mean arterial pressure was decreased after melatonin pre-medication and extended to the early post-operative period. This mild hypotensive effect of melatonin may be beneficial in elderly patients, particularly those at cardiovascular risk [Citation22].
Previous studies showed that melatonin could decrease MAP in healthy women [Citation41] and men [Citation42]. The mechanism of action of melatonin on circulation is complex and unclear. Melatonin may bind to specific melatonin receptors in the blood vessels, interfering with the vascular response to catecholamine [Citation43]. Furthermore, melatonin may interfere with the peripheral and central autonomic system, causing a reduction in adrenergic outflow and catecholamines levels [Citation44]. In addition, it may induce relaxation of the smooth muscle of the arterial walls via increasing nitric oxide availability [Citation45,Citation46].
Intraoperative bleeding was significantly less in TDM group as compared to C and TDF groups. Intraoperative hypotension effectively decreases surgical blood loss and improves surgical field exposure which is essential for spinal surgeries. This result explained significant increase in the surgeon‘s satisfaction score in the TDM group compared to the C and the TDF groups.
As regards the TDF, these results are in agreement with the findings of Amr et al. (2012) who reported that there were no statistically significant differences between the TDF and control (C) groups in the hemodynamic parameters [systolic blood pressure (SBP), diastolic blood pressure (DBP) and heart rate (HR)] throughout the period of the study [Citation39].
As regards side effects in our study, all cases of the 3 groups were hemodynamically stable, no patient developed hypoxia and there were no reported intraoperative complications interfering with the course of surgery or interrupting the surgeons. Two patients in the C group suffered from nausea (p = 0.08). In the TDF group, nausea and vomiting occurred only in 25% of cases (n = 6/25) (p = 0.01) in spite of the fact that preoperative granisetron (1 mg IV) was given as a prophylactic antiemetic and there were no reported cases of erythema, respiratory depression or pruritus. In the TDM group, two patients were dizzy (p = 0.08).
These results are in agreement with the findings of Amr et al. (2012) who reported that nausea and vomiting occurred only in 32% of cases (16/50 patients) during transdermal administration of fentanyl 50 μg/h 10 h preoperatively for postoperative pain relief after major abdominal surgery [Citation39].
In the TDF group with delivery rate of 75 μg/h the incidences of respiratory depression, sedation and nausea/vomiting were 11%, 22% and 83% respectively [Citation47]. Another study showed that, the incidence of respiratory depression was higher in the TDF group with delivery rate of 75 μg/h (15%) than in the TDF group with delivery rate of 50 μg/h [Citation35]. The results of our study were partially consistent with Minville et al. (2008) who reported that in the TDF group (15 patients) with delivery rate of 50 μg/h, there were no reported cases of sedation, respiratory depression or erythema; pruritus occurred in one patient and nausea/vomiting occurred in 7 patients; and the only prominent adverse event was the occurrence of local erythema in 30% of patients received transdermal fentanyl [Citation36].
Regarding adverse effects in patients who received TDM, patients were more sedated (P < 0.05) and two patients were dizzy (p = 0.08). These results were nearly similar to the results proved by Ismail and Mowafi (2009) who found that one patient in their melatonin group (n = 20) complained of dizziness [Citation22].
Limitations of the study
Our study presented several limitations. First, the results did not allow for an evaluation of the effectiveness of TDF or TDM in all types of surgery. The second limitation was the small sample size preventing achievement safety conclusions. The third limitation of our study is that we did not measure fentanyl and melatonin plasma levels so the interaction between both agents and endogenous melatonin could not be assessed.
Conclusion
Transdermal administration of fentanyl 50 μg/h or transdermal therapeutic system containing 7 mg of melatonin 2 h preoperatively was an effective, simple, noninvasive, and convenient technique and a safe adjuvant for acute pain after lumber laminectomy. TDF and TDM allowed delivery of a potent analgesic agent providing a stable serum concentration for an extended period of time with acceptable minimal side effects.
Recommendations
The use of the TDF or TDM patches as a component of a multimodal analgesic system (i.e. in conjunction with regional blocks, a non-steroidal anti-inflammatory drug (NSAID), an acetaminophen or an α-agonist) may provide an effective postoperative analgesic regimen.
Clinical trial registration: ClinicalTrials.gov Identifier: NCT02726126
Conflict of interest
None.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- R.MelzackPsychological aspects of pain: implications for neural blockadeM.J.CousinsP.O.BridenbaughNeural blockade in clinical anesthesia and management of pain2nd ed.1989J.B. LippincottPhiladelphia845860
- J.M.DesboroughThe stress response to trauma and surgeryBr J Anesth852000109117
- F.CarliN.MayoK.KlubienEpidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery: results of a randomized trialAnesthesiology972002540
- I.KissinPreemptive analgesiaAnesthesiology93200011381143
- M.McCafferyB.FerrellNurses’ knowledge of pain assessment and management: how much progress have we made?J Pain Symptom Manage1431997175188
- B.KücükakinJ.LykkesfeldtH.J.NielsenR.J.ReiterJ.RosenbergI.GögenurUtility of melatonin to treat surgical stress after major vascular surgery–a safety studyJ Pineal Res442008426431
- B.BernerV.A.JohnPharmacokinetic characterization of transdermal delivery systemsClin Pharmacokinet261994121134
- A.S.MichaelsS.K.ChandrasekaranJ.E.ShawDrug permeation through human skin: theory and in vitro experimental measurementAm Inst Chem Eng J211975985996
- I.SiafakaP.RelliaE.ArgyraN.IakovidouC.SykiotisA.VadaloukaPharmacokinetic profile and efficacy of a fentanyl transdermal delivery system for acute postoperative pain after intra-abdominal gynecologic surgery for cancerPain Practice42200498104
- R.B.R.MuijsersA.J.WagstaffTransdermal fentanyl. An updated review of its pharmacological properties and therapeutic efficacy in chronic cancer pain controlDrugs61200122892307
- C.J.McCartneyA.SinhaJ.KatzA qualitative systematic review of the role of N-methyl-D-aspartate receptor antagonists in preventive analgesiaAnesth Analg98200413851400
- P.M.PleziaT.H.KramerJ.LinfordS.R.HameroffTransdermal fentanyl: pharmacokinetics and preliminary clinical evaluationPharmacotherapy9198929
- F.B.SevarinoJ.S.NaultyR.SinatraTransdermal fentanyl for postoperative pain management in patients recovering from abdominal gynecologic surgeryAnesthesiology7731992463466
- P.R.BromageH.R.ShibataH.W.WilloughbyInfluence of prolonged epidural blockade on blood sugar and cortisol responses to operations upon the upper part of the abdomen and thoraxSurg Gynaecol Obstetr211971330335
- B.DonnerM.ZenzM.TrybaFentanyl TTS zur postoperativen Schmerztherapie. A neue Alternative?Anesthetist4251993309315
- J.ArendtIn melatonin and the mammalian pineal gland1995Chapman & HallLondonp.42, 207
- J.BarrenetxeP.DelagrangeJ.A.MartinezJ Physiol Biochem60200461
- F.WaldhauserM.WaldhauserH.R.LiebermanM.H.DengH.J.LynchR.WurtmanJ Neuroendocrinol391984307313
- B.LeeK.ParrottJ.AyresR.SackRes Commun Mol Path Pharmacol8531994337346
- B.KücükakinModification of surgical stress response by perioperative melatonin administrationDan Med Bull5752010B4144
- P.K.ZahnT.LansmannE.BergerE.SpeckmannU.MusshoffGene expression and functional characterization of melatonin receptors in the spinal cord of the rat: implications for pain modulationJ Pineal Res3520032431
- S.A.IsmailH.A.MowafiMelatonin provides anxiolysis, enhances analgesia, decreases intraocular pressure, and promotes better operating conditions during cataract surgery under topical anesthesiaAnesth Analg108200911461151
- C.X.YuC.B.ZhuS.F.XuX.D.CaoG.C.WuSelective MT2 melatonin receptor antagonist blocks melatonininduced antinociception in ratsNeurosci Lett2822000161164
- N.-M.BenyahiaM.B.BreebaartL.SermeusM.VercauterenRegional analgesia techniques for spine surgery: a review with special reference to scoliosis fusionJ Spine4201520810.4172/2165-7939.1000208
- P.RahimzadehS.H.R.FaizM.AlimianA.Mohammadian ErdiRemifentanil versus dexmedtomidine for posterior spinal fusion surgeryMed J Islam Repub Iran292015215 [6 June]
- H.RutbergE.HakansonL.AnderbergL.JorfeldtJ.MartenssonB.SchildtEffects of the extradural administration of morphine, or bupivacaine, on the endocrine response to upper abdominal surgeryBr J Anesth561984233237
- N.-C.HjortsoN.J.ChristensenT.AndersenH.KehletEffects of the extradural administration of local anesthetic agents and morphine on the urinary excretion of cortisol, catecholamines, and nitrogen following abdominal surgeryBr J Anesth571985400406
- R.R.RikerJ.T.PicardG.L.FraserProspective evaluation of the sedation–agitation scale for adult critically ill patientsCrit Care Med27199913251329
- D.L.StreinerG.R.NormanScaling responsesD.L.StreinerG.R.NormanHealth measurement scales: a practical guide to their development and use1995Oxford University PressOxford2853
- T.RathjenU.BockmuhlC.A.GreimModern anesthesiologic concepts supporting paranasal sinus surgeryLaryngorhinootologie8520062023
- K.RadwanM.YoussefA.El-TawdyM.ZeidanN.KamalMelatonin versus Gabapentin. A comparative study of preemptive medicationsInternet J Anesthesiol2312010 [DOI: https://doi.org/10.5580/265 See more at: http://www.ispub.com/journal/theinternetjournalofanesthesiology/volume-23-number-1/melatoninversusgabapentinacomparativestudyaspreemptivemedications.html#sthash.tGPya1vY.dpuf]
- H.BorazaaS.TuncerN.YalcinA.ErolS.OtelciogluEffects of preoperative oral melatonin premedication on postoperative analgesia, sleep quality and sedation in patients undergoing elective prostatectomy: a randomized clinical trialJ Aesth242010155160
- W.CaumoF.TorresN.L.MoreiraJr.J.A.AuzaniC.A.MonteiroG.LonderoThe clinical impact of pre-operative melatonin on post-operative outcomes in patients undergoing abdominal hysterectomyAnesth Analg105200712631271
- M.KilbrideM.MorseA.SenagoreTransdermal fentanyl improves management of postoperative hemorrhoidectomy painDis Colon Rectum3711199410701072
- A.N.SandlerA.D.BaxterJ.KatzA double-blind, placebo-controlled trial of transdermal fentanyl after abdominal hysterectomy. Analgesic, respiratory, and pharmacokinetic effectsAnesthesiology81199411691180
- V.MinvilleV.LubranoV.BounesA.PianezzaA.RabinowitzC.GrisPostoperative analgesia after total hip arthroplasty: patient-controlled analgesia versus transdermal fentanyl patchJ Clin Anesth202008280283
- G.R.LaurettiA.L.MattosR.AlmeidaI.C.P.R.LimaC.S.ResendeEfficacy of fentanyl transdermal delivery system for acute postoperative pain after posterior laminectomyPost Sess/Euro J Pain132009S55S285
- E.BarreraS.Fernandez-GalinskiM.D.FerrerF.EscolanoM.PuigPostoperative analgesia induced by transdermal fentanyl in dorsal and lumbar spine arthrodesisPost Sess/Euro J Pain132009S255S285
- A.Amr SamyG.Mostafa MostafaA.M.Mostafa MohamedEfficacy and safety of transdermal fentanyl patches on postoperative pain relief after major abdominal surgeryJ Am Sci862012417424
- M.B.KhezriH.MerateThe effects of melatonin on anxiety and pain scores of patients, intraocular pressure, and operating conditions during cataract surgery under topical anesthesiaInd J Ophthalmol612013319324
- A.De JongheB.C.Van MunsterH.E.van OostenJ.C.GoslingsP.KloenC.van ReesThe effects of melatonin versus placebo on delirium in hip fracture patients: Study protocol of a randomized, placebocontrolled, double blind trialBMC Geriatr11201134
- A.CagnacciS.AranginoM.AngiolucciE.MaschioG.B.MelisInfluences of melatonin administration on the circulation of womenAm J Physiol2741998R335R338
- S.AranginoA.CagnacciM.AngiolucciA.M.VaccaG.LonguA.VolpeEffects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy menAm J Cardiol83199914171419
- E.SewerynekMelatonin and the cardiovascular systemNeuro Endocrinol Lett23suppl 120027983
- R.M.BuijsS.E.La FleurJ.WortelC.Van HeyningenL.ZuiddamT.C.MettenleiterThe suprachiasmatic nucleus balances sympathetic and parasympathetic output to peripheral organs through separate preautonomic neuronsJ Comp Neurol46420033648
- M.M.AnwarA.R.MekiH.H.RahmaInhibitory effects of melatonin on vascular reactivity: possible role of vasoactive mediatorsComp Biochem Physiol C Toxicol Pharmacol1302001357367
- F.B.SevarinoD.PaigeR.S.SinatraPostoperative analgesia with parenteral opioids: does continuous delivery utilizing a transdermal opioid preparation affect analgesic efficacy or patient safety?J Clin Anesth931997173178