Abstract
Background
Epidural opiate analgesia carried by gelfoam in the epidural space is to improve the quality of perioperative pain relief. The aim of this study was to compare the analgesic efficacy of gelfoam soaked in morphine with crystalloids versus colloid versus direct application of morphine in epidural space in patients undergoing lumbar laminectomy under general anesthesia.
Methods
This study was a prospective, randomized, double-blinded trial. 75 male and female patients aged from 18 to 65 years from ASA class I or II scheduled for Lumbar laminectomy surgery were randomly divided into three equal groups: group A: (control group): 5 ml of 1 mg/ml morphine was directly instilled over intact epidural space, group B (crystalloid group): apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml crystalloid (0.9% sodium chloride) placed in intact epidural space; and group C (colloid group): apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml hydroxyethyl starch 6% (HES 6%) placed in intact epidural space by the neurosurgeon. Total analgesics, time to first analgesic request, visual analogue scale (VAS), hemodynamics, respiratory rates and adverse effects were recorded.
Results
As regards Patient’s characteristics, age, gender, weight, ASA class and operative time were comparable in all studied groups, and groupsB and C showed less amount of analgesia, long time to analgesic request, and less main VAS. No statistically significant differences are in hemodynamics, and the incidences of side effects showed no statistically significant differences among the three groups of study.
Conclusion
Epidural use of gelfoam soaked by morphine in HES 6% is an effective method for post operative analgesia after lumbar laminectomy.
1 Introduction
Parenteral opioids have been the mainstay for treatment of postoperative pain after lumbar laminectomy. The main drawback of parenteral opioids is that these drugs are usually given with relatively large time lapses, so that there are wide fluctuations in clinical effect. Ideal postoperative analgesia should provide continuous pain relief, in an alert patient who can be mobilized early [Citation1] alternatives to standard pain management include, epidural administration of narcotics as a single dose at the time of the surgery or via an epidural catheter postoperatively [Citation2]. Epidural catheters are difficult to manage and maintain after spine surgery. In addition, there is always a concern of infection, restricting its widespread application [Citation3]. The easy access to epidural space during laminectomy surgery was utilized safely for applying morphine directly over the exposed dura mater in earlier studies but has limited application due to short duration of action (3–24 h) [Citation4]. The routine use of surgical gelfoam in the epidural space at the completion of surgery prompted the use of gelfoam as an extended release drug delivery system to prolong the effect of epidural morphine [Citation5]. Earlier studies have compared application of gelfoam soaked in saline with morphine in epidural space to directly applicated morphine [Citation6], but no definitive conclusions can show the differences between each of colloids and crystalloids with gelfoam soaked morphine compared to direct morphine application and for this the present study was designed. Many studies applied colloid in the epidural space either for management of post spinal headache or as epidural volume expansion to augment intrathecal block, and the study by Amira et al. [Citation21] was designed to examine the effects of colloid (6% HES) versus normal saline (0.9%) for epidural volume expansion in combined spinal epidural anesthesia for elective cesarean delivery and to assess the quality of block and hemodynamic stability. Also, several studies recommend dextran 40 colloid as an infusion or as a bolus in the epidural space in the management of post dural puncture headache, and conclude that the high molecular weight and viscosity of Dextran 40 slow its removal from the epidural space [Citation22].
Table 3 The incidences for different complications.
The aim of this study was to compare the analgesic efficacy of gelfoam soaked in morphine with crystalloids versus colloid versus direct application of morphine in epidural space in patients undergoing lumbar laminectomy under general anesthesia.
2 Patients and methods
This study was approved by institutional ethics committee of El-Minia University Hospital, and carried out in duration from March to December 2015. A written consent was obtained from 75 male and female patients aged from 18 to 65 years from ASA class I or II undergoing lumbar laminectomy. The patients were randomly allocated into three equal groups using a computer-generated sequence of random numbers and a sealed envelope technique. Study drugs were prepared by an anesthetist who did not participate in the operation; this study was conducted in a random double-blind manner (neither the administrator of the drug nor the patient knows the nature of drugs given). We exclude with sepsis or coagulopathy, patients undergoing cervical laminectomy, spine-fixation surgery, patient with herniated sequestered disk, previous history of spine surgery, patients having significant medical diseases especially neuromuscular disease or psychological disease and sever bronchial asthma, history of drug abuse and accidental dural tear during surgery. Preoperative assessment and preparation: A careful medical history was taken, general examination including pulse, arterial blood pressure and respiratory rate, local examination including chest, heart, and abdomen. Routine investigations including hemoglobin concentration, coagulation profile, renal function test, liver function test, random blood sugar and electrocardiogram (ECG). Technique of the study of Standard monitoring (i.e. electrocardiogram with two derivations, pulse oximetry (SpO2), non-invasive arterial pressure measurement, end tidal CO2(EtCO2), body temperature) was employed, and baseline parameters were recorded. This monitoring was done using Datex-Ohmeda (made by GE Healthcare Co., USA) continued till extubation. Then 20F I.V catheter was inserted for administration of drugs and fluids and all patients received fluid preload (ringer’s lactate solution or isotonic saline 10 ml/kg) and antibiotic. All patients were premedicated with 3 mg midazolam, 50 mg ranitidine and 10 mg metoclopramide before induction of anesthesia. Induction of anesthesia was done for all patients with fentanyl (1 μg/kg), propofol (2 mg/kg) and atracurium (0.5 mg/kg) followed by insertion of endotracheal tube. Anesthesia was maintained by isoflurane (1.2 MAC), atracurium (0.15 mg/kg intermittent every 20–30 min) and propofol infusion if needed to keep mean arterial blood pressure between 60 and 65 mmHg and ventilation was adjusted to maintain end tidal CO2 between 30 and 35. Our work was started after the end of laminectomy stage and after making sure that there was no accidental Dural injury before final closure and the patient not operated for spinal fixation, and patients were divided randomly into 3 equal groups by computer generated randomization: Group A (control group): 5 ml of 1 mg/ml preservative-free morphine sulfate (astramorph, FRESENIUS KABI, USA) was directly instilled over intact epidural space by the neurosurgeon; Group B (crystalloid group): apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml crystalloid (e.g. saline) placed in intact epidural space by the neurosurgeon; and Group C (colloid group): apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml colloid (hydroxyethyl starch 6%) placed in intact epidural space by the neurosurgeon. After surgery was over, patients turned supine, isoflurane stopped and neuromuscular blockade was reversed by I.V Neostigmine (0.05 mg/kg) with 1 mg atropine, after return of spontaneous respiration, trachea extubated and patients remain under continuous monitoring. All patients received supplemental oxygen for the first 30 min. After this time, oxygen was administered only when patient had saturation below 92%.
2.1 Parameters assessed
Hemodynamic parameters (heart rate, blood pressure), oxygen saturation (SPO2), respiratory rate, VAS (visual analogue scale: subjective pain was measured by VAS on a scale of 0–10 with 0 representing no pain and 10 worst imaginable pains [Citation5]. At first 48 h postoperative opioids and other analgesic were prohibited except if subjective pain measured by VAS was more than 3 diclofenac sodium 75 mg ampule infused, and the time to first analgesic request was recorded as the time from the end of operation till the time to first analgesic request - total analgesic consumptions in the initial 24–48 h post operative. Sedation score: Level of sedation was assessed by 5-point ordinal scale [Citation7], where, 0 means alert patient, 1 stands for patient who is drowsy, 2 is for frequently drowsy and disoriented, 3 is very drowsy and disoriented, and 4 is stupors and difficult to arouse. Time of ambulation: patients were encouraged to ambulate 6 h after surgery if they felt comfortable, and it was counted from the time at which patients were discharged from operative room until the time that the patients could be ambulated and it was recorded in all cases - postoperative complications or adverse effects such as respiratory depression, nausea, vomiting, pruritus, bradycardia, pressure symptoms and need for supplemental oxygen. For the purpose of study, bradycardia was defined as heart rate less than 50 beats per minute. Respiratory depression was defined as respiratory rate less than 10 per minute, need of oxygen supplementation was recorded if patients had oxygen saturation of less than 92%, and urinary retention was labeled as absence of spontaneous voiding more than 7 h after removal of bladder catheter [Citation8]. Severity of pruritus was graded as follows: 0 = absent; 1 = mild – restricted to one area not troubling the patient and reported only on prompting the patient; 2 = Moderate – affecting a large area, not disturbing the patient and not requiring treatment; and 3 = Severe – generalized, often disturbing the patient and requiring treatment [Citation9]. All parameters were assessed hourly in the first 6 h postoperative then every 2 h in the next 12 h and 4 h interval in the remaining period of follow-up time.
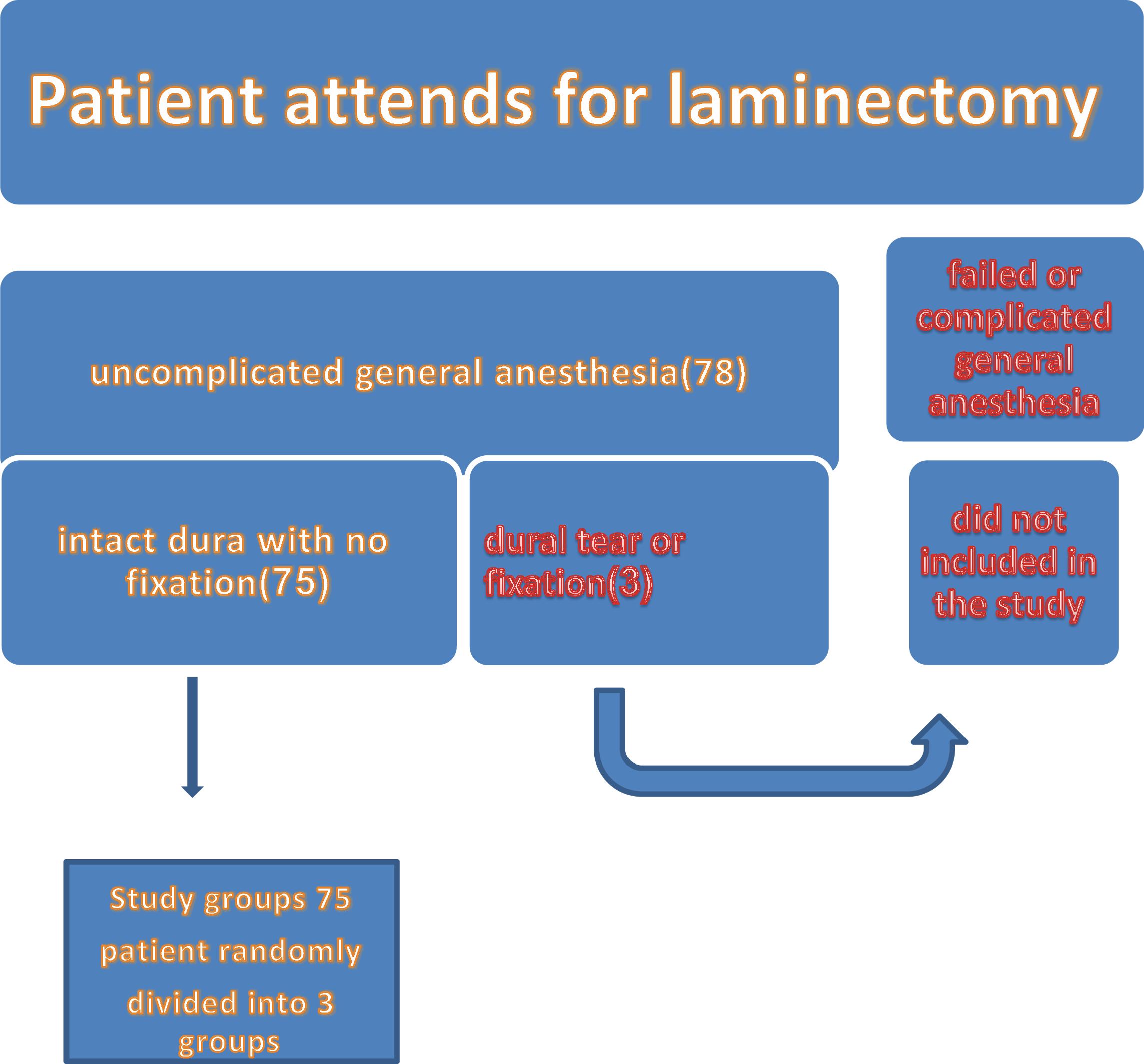
Flowchart for patient allocation in the study
2.2 Statistical analysis
Based on prior study, the sample size was calculated to detect 20 h difference in the time to first analgesia between study and control groups at power of 0.80, confidence interval of 95% and significance level of 0.05. Calculating for a 20% dropout rate, 25 patients in each group were appropriate to detect this difference. Data were analyzed using Statistical Package of Social Sciences (SPSS) software and expressed as mean ± standard deviation and median (minimum-maximum) for numerical data or as number and percent (%) for categorical data. Intergroup comparisons of continuous numerical variables were done using ANOVA test for parametric data or Kruskal-Wallis one way test for non-parametric data. Intragroup comparisons to baseline values were done using paired t-test for parametric data or Wilcoxon test for non-parametric data. The level of significance was fixed at a minimum of 0.05%.
3 Results
We started laminectomy by 78 patients, and we excluded 3 patients before administration of study drugs (2 cases of dural tears and one case the surgeon decided to fix his spine), so, our study included 75 patients, 25 in each group, who were scheduled for laminectomy surgery). All allocated patients completed the study. As regards Patient’s characteristics, age, gender, weight, ASA class and operative time were comparable in all studied groups. Regarding the changes in HR in group A baseline value was 87.64 ± 8.77 beat/min, and this value was significant reduced at 2, 4 and 6 h postoperative while there was significant increase in mean values at 38 and at 48 h postoperative; in group B baseline value was 84.28 ± 12.18 and this value was significantly reduced at 2, 4, 6 and 10 h postoperative, while in group C baseline value was 8652 ± 12.22 and this value was significantly reduced throughout the study period at 2, 4, 6, 10, 14, 18, and 22. Between group comparisons P1 (p value of comparison between A and B) baseline values were comparable up to 6 h post operative (P1 was >0.05) but there were significant reductions in mean values of group B in comparison with group A from 10 to 48 h postoperative; P2 (P value of comparison between A and C) baseline values were comparable up to 4 h (P2 > 0.05) but there were significant reductions in values of group C from 6 to 48 h postoperative; and P3 (P value of comparison between B and C) baseline values were comparable between group B and C throughout the study period. Regarding the changes in MAP, in group A, baseline value was 90.84 ± 10.29, and all values reported throughout the study period were comparable to the baseline values; there were significant reductions in mean values at 2 and 4 h postoperative while it was significantly increased at 38 and 48 h postoperative. In group B baseline value was 93.16 ± 10.12 and all recorded values were significantly lower than baseline throughout all the study period postoperative; in group C baseline value was 94.28 ± 8.88 and there were significant reductions in mean values from 2 h up to 30 h. Between group comparisons, in group B, (MAP) were significantly lower than in group A from 2 to 48 h, and in group C there were significant reductions in values of group C from 2 h up to 38 h when compared to group A. Regarding respiratory rate, mean changes of respiratory rate RR are expressed in ; in group A there were significant reductions of mean values up to 6 h postoperative, in group B were significantly reductions up to 18 h while in group C there were significantly reductions up to 30 h postoperative.
Table 1 Comparison of respiratory rate (RR) (breath/min).
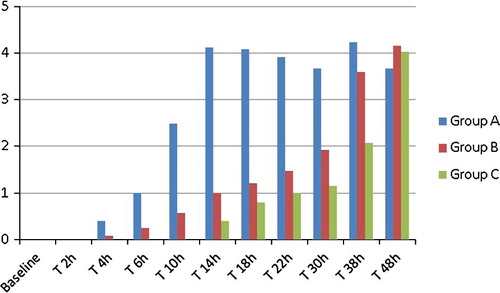
3.1 Visual analogue scale
Mean changes in visual analogue scale (VAS) are represented in . VAS score was higher in group A than in group B and C at most time points of the study, and in comparison between B and C mean VAS score was significantly lower in group C from 6 h till the end of study period (48 h).
The sedation scores were comparable in the 3 groups at all set time points and there were insignificant differences in their values throughout the studied times in the 3 groups except at 4 h and 6 h in which sedation score values were significantly higher in group B than in the 2 other groups.
shows time to ambulation (hours) in group C was (6 ± 1.25) significantly earlier than in group A, and time to first analgesic request (hours) showed that group C has 43.04 ± 2.13 which was significantly longer than both other groups A and B have, i.e. 11.88 ± 1.33 and 38.04 ± 2.05 respectively. Patients in group A significantly required higher doses of analgesia during first 48 h postoperative (192 ± 48.7 mg). When compared to group B (57 ± 39.2 mg) P1 was 0.0001 and also when compared to group C (48 ± 36.7 mg) P2 was 0.0001, but there were insignificant differences when we compare group B to group C (P3 was 0.40). There were insignificant differences in time to discharge between the studied groups.
Table 2 Time to ambulation, time to first analgesic requirement, total postoperative analgesic consumption and time to discharge.
3.2 Side effects ()
As regards postoperative nausea and vomiting (PONV), 8 patients (32%) in group A developed postoperative nausea only versus 4 patients (16%) in each other group and P-value was 0.28 whereas 3 patients (12%) in group A were observed to have vomiting versus 2 patients (8%) in each other group and P-value was 0.58. Only one patient in each group develops repeated vomiting and was treated by I.V ondansetron 100 μg/kg. Ten patients in group A developed itching versus 7 patients in group B and 6 patients in group C (24%). In all patients itching was of mild intensity except that one patient in group A was of moderate intensity; however, none of them was disturbed or required any treatment and P-value was 0.63 with mild itching and 0.36 with moderate itching. Incidence of urinary retention in group A was occurred in 7 patients versus 6 patients in group B and 4 patients in group C and also P-value was 0.58; all patients developed retention treated by insertion of urinary catheter for 24 h and then catheter was removed without any residual complaint.
5 Discussion
In our study 75 male and female patients aged from 18 to 65 years from ASA class I or II undergoing lumbar laminectomy under general anesthesia randomly were divided into three equal groups 25 in each group. Anesthetic technique was standardized in all the groups and at the completion of laminectomy group A 5 mg morphine (1 mg/ml) was instilled over the intact epidural space whereas in group B apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml crystalloid (sodium chloride 0.9%) placed in intact epidural space and in group C apiece of gelfoam 5 cm × 1 cm soaked in 5 mg morphine diluted with 5 ml colloid (HES 6%) placed in intact epidural space, and we found that epidural administration of morphine using gelfoam is an effective method for post operative analgesia after lumbar laminectomy; in addition, soaking of gelfoam in HES 6% resulted in longer duration of analgesia, lesser analgesic consumption postoperative with minimal side effects, as we observed that the mean VAS score in the group C remained less as compared to group B and group A at most times of study. This implies that patients in group C had less pain as compared to other two groups, and total analgesic consumption was greater in group A than in gelfoam groups and time to first analgesic request was longer in groups B and C than in group A, with earlier ambulation in gelfoam groups in than group A. The explanation of earlier ambulation in both groups in which gelfoam soaked morphine was used makes most patients pain-free and this is important because earlier ambulation lifts the morale of the patient, relieves the surgeon’s anxiety and also reduces the chances of postoperative complications. While better control of pain in groups B and C and rapid fading painkilling effect of morphine in group A because of free opiates placed at the time of the surgery are diluted by blood and tissue fluids, they are lost into the disk space, and are absorbed systemically, thus limiting its duration of action [Citation14]. Morphine was the first opioid approved by the Foods and Drugs Administration (FDA) for spinal administration and it is the epidural opioids that have been the most widely used and with which others are compared [Citation4]. After spine surgery epidural catheters are difficult to manage and maintain. In addition, there is always a concern of infection, restricting its widespread application [Citation3]. Other investigators have attempted to prolong the duration of analgesic action by morphine-adon L compound, Oxiplex/SP gel-morphine [Citation10] and Vaseline-Sterile-Oil-Morphine [Citation11] and many of these techniques lack wider applicability. Liposomal based extended release epidural morphine (EREM) has been recently introduced and successfully used extending the duration of analgesic action of morphine. However, this preparation is costly and not easily available [Citation12]. The easy access to epidural space during laminectomy surgery can be utilized for applying morphine directly over the exposed dura mater and the routine use of surgical gelfoam in the epidural space at the completion of surgery encouraging us to use gelfoam as an extended release drug delivery system in our study. Earlier studies have tried application of gelfoam soaked in saline with opiates in epidural space. Mishra et al. tried 0.3 mg buprenorphine diluted to 5 ml with normal saline soaked into an absorbable gelatin sponge was placed in the epidural space under direct vision as a technique for extended ambulatory epidural pain control after lumbar discectomy [Citation5]. Another study by Gibsons, et al. tried another technique in which an absorbable gelatin sponge (Gelfoam) is contoured to the laminectomy defect, placed in methylprednisolone acetate (40–80 mg), and then injected with 2–4 mg of preservative-free morphine (a small needle was used to fill the sponge). The sponge is placed over the defect before closure [Citation13]. While Kundra et al. compared the effect gelfoam soaked in morphine to direct epidural application of morphine [Citation6] but in these studies morphine was diluted by saline, efficacy and duration of action of morphine when diluted with colloid like hydroxyethyl starches (HES 6%) were not compared when applicated via gelfoam to other methods mentioned before, so no definitive conclusions can show the differences between each of colloids and crystalloids with gelfoam soaked morphine compared to direct morphine application. When we compare our study with other studies we find that the dose of epidural morphine used in our study corresponds to the doses used in earlier studies. Gibson Kevin used single dose of 4 mg in lumbar spine surgery [Citation13]. Chen used 3 mg epidural morphine in lumbar laminectomy surgery [Citation15], Carvalho et al. used 5 mg epidural morphine in obstetric patient [Citation16], and gambling used 5 mg morphine in epidural space for lower abdominal surgeries [Citation17]. Some authors have tried using even smaller doses of epidural morphine in an attempt to reduce the incidence and severity of adverse effects. Wu et al., used 1 mg doses of morphine using a microfibrillary paste; however, using such smaller doses also reduces duration of analgesic effect [Citation14]. Study done by Kundra et al. was in agreement with our study that compares gelfoam soaked morphine with crystalloid. This was in conformity with our work in group B and group A respectively, and they reported that mean VAS score in group 1 (gelfoam morphine) remained less as compared to group 2 (direct epidural morphine) at most time intervals studied. This implies that patients in group 1 had less pain as compared to group 2. The mean duration of action of a single dose epidural instillation of morphine was 10.25 h in group 2 and it prolonged to 30.25 h in group 1. In group 2, total analgesic consumption was almost greater than 3.5 times and supplemental analgesia was required almost 20 h earlier as compared to group 1, with short time to ambulation and higher sedation scores in gelfoam group. Carvalho et al. reported the single dose of epidural morphine to provide analgesia for 3 h and this difference could be due to the fact that the study was performed in post-cesarean patients, and pregnant state is known to alter pain perception [Citation16]. Yaddanapudi et al., reported that the effect of single dose of epidural morphine lasted 10.1 h and this was in agreement with our result in group A and we have clear prolongation in gelfoam groups bearing in mind that this study compares epidural morphine by conventional method to epidural tramadol [Citation18]. Gibson et al., reported that 60% of patients did not require supplemental analgesia on the day of surgery when gelfoam soaked in morphine was placed in the epidural space [Citation13]. However, in that study, dose of morphine injected in the gelfoam was not standardized (2–4 mg) and methylprednisolone was also injected in the gelfoam. Although there was statistically significant reduction in values of MAP and HR and RR in varying degrees when compared with their base line values, there was no clinically symptomatic hypotension, bradycardia or respiratory depression required any treatment with naloxone or supplemental oxygen. The incidence of other adverse effects in our study was small with insignificant differences in incidences of postoperative nausea and vomiting (PONV), itching and urinary retention between the studied groups. Kundra et al. reported that incidence of postoperative nausea only when in group 1 was 26.7% vs. 33.3% in group 2 while incidence of vomiting was 8% vs. 13.33% respectively whereas incidence of itching was 30.66% within group 1 vs. 38.66% in group 2 and incidence of urinary retention was 8% in group 1 vs. 0% in group 2 [Citation6]. In comparison with our study the incidence of PONV and itching was convergent but our study still has lower incidences clearly noticed in group C; this can be explained by smaller doses of morphine released from gelfoam soaked in colloid. As regards urinary retention higher incidences were observed in our study in all groups. We cannot explain this as clearly as there was no clear explanation for the lack of retention with directly applicated morphine in the study done by Kundra et al. There are many theories that explain the effect of epidural opioids in general on the urodynamic function. In a nationwide follow-up survey in Sweden, anesthesiologists reported a greater incidence of postoperative urinary retention (POUR) with epidural morphine (38%) compared with intrathecal morphine (13%) [Citation19]. However, at close analysis, the patients who developed POUR had bladder catheterization as a result of the type and the duration of surgery, making assessment of POUR more difficult. The incidence of POUR after epidural opioids may also be related to the level at which opioids are injected. Administration of opioids in the lumbar epidural space is associated with higher rate of urinary retention compared to thoracic [Citation20]. Detrusor strength starts to decrease within 5–15 min after 4 mg of epidural morphine, and its maximum effect reached between 30 and 120 min and lasting 10–15 h [Citation19]. Left to point out, there were several limitations to the current study and further studies are needed to compare the effect of different doses of morphine aiming to detect the optimal dose that provides longer duration of analgesia with least side effects.
In conclusion, epidural administration of morphine using gelfoam is an effective method for post operative analgesia after lumbar laminectomy using gelfoam soaked in HES 6% resulted in longer duration of analgesia and lesser postoperative analgesic consumption with minimal side effect.
5.1 Recommendation
We recommend routine use of epidural gelfoam soaked morphine with colloid in our hospital, but we encourage further studies that conducted blindly and involving larger sample size of population of different ASA classifications and try different doses of morphine aiming to detect the optimal dose that provides longer duration of analgesia with least side effects. Also, we can try other adjuvant to improve the quality of analgesic effect of morphine in gelfoam carrier as using steroids such as methylprednisolone that can reduce postoperative radiculopathy due to its anti-inflammatory effect that reduces inflammation around nerve root and also reduces usage of systemic steroids post operative. It remains to point out that we did not have long term follow-up of patients to evaluate chronic post-surgical pain (CPSP) and it was a weak point in current study as occurrence of CPSP may be one of pressure symptoms due to epidural gelfoam. This is extremely important because compression of nerve roots can cause motor or sensory deficits in the area of distribution.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- D.A.RawJ.K.BeattieJ.M.HunterAnaesthesia for spinal surgery in adultsBr J Anaesth912003886904
- Y.IshikawaY.ImashukuH.KitagawaEvaluation of the side effects of intravenous patient controlled analgesia after spine surgeryMasui602011920923
- T.KlubaF.HofmannS.BredangerEfficacy of post-operative analgesia after posterior lumbar instrumented fusion for degenerative disc disease: a prospective randomized comparison of epidural catheter and intravenous administration of analgesicsOrthop Rev (Pavia)220102730 e9
- B.Mugabure BujedoS.González-SantosA.Uría AzpiazuA review of epidural and intrathecal opioids used in the management of postoperativeJ Opioid Manage832012177192
- L.D.MishraS.S.NathR.L.GairolaBuprenorphine-soaked absorbable gelatin sponge: an alternative method for postlaminectomy pain reliefJ Neurosurg Anesthesiol162004115121
- S.KundraV.GuptaH.BansalComparative study of epidural application of morphine versus gelfoam soaked in morphine for lumbar laminectomyJ Anaesthesiol Clin Pharmacol3020144652
- K.S.VoraV.R.ShahB.PatelPostoperative analgesia with epidural opioids after cesarean section: comparison of sufentanil, morphine and sufentanil-morphine combinationJ Anaesthesiol Clin Pharmacol282012491495
- B.CarvalhoE.RileyS.E.CohenSingle-dose, sustained-release epidural morphine in the management of postoperative pain after elective cesarean delivery: results of a multicenter randomized controlled studyAnesth Analg100200511501158
- W.ChiravanichM.OofuvongN.KovitwanawongSingle dose of gabapentin for prophylaxis of intrathecal morphine-induced pruritis in orthopedic surgery: a randomized controlled trialJ Med Assoc Thai952012186190
- L.MastronardiM.PappagalloC.TattaThe oxiplex/SP gelmorphine compound after lumbar microdiscectomy in the management of postoperative pain. Report of 20 casesSurg Neurol6420057578
- L.MastronardiM.PappagalloC.TattaR.RopertoA.ElsawafL.FerrantePrevention of postoperative pain and of epidural fibrosis after lumbar microdiscectomy: pilot study in a series of forty cases treated with epidural vaseline-sterile-oil-morphine compoundSpine (Phila Pa 1976)33200815621566
- S.C.OffleyE.CoyneM.HorodyskiRandomized trial demonstrates that extended-release epidural morphine may provide safe pain control for lumbar surgery patientsSurg Neurol Int4Suppl 22013S51S57
- K.J.GibsonsA.P.BarthA.AhujaLumbar discectomy: use of an epidural morphine sponge for postoperative pain controlNeurosurgery36199511311135
- M.H.WuC.H.WongC.C.NiuA comparison of three types of postoperative pain control after posterior lumbar spinal surgerySpine (Phila Pa 1976)36201122242231
- T.Y.ChenEfficacy of topical microfibrillar collagen mixed with steroid hormone and morphine for postoperative pain control during lumbar laminectomy: a preliminary reportChang Gung Med J2520028188
- B.CarvalhoL.M.RolandL.F.ChuSingledose, extended-release epidural morphine (DepoDur) compared to conventional epidural morphine for post-cesarean painAnesth Analg1052007176183
- D.GamblingT.HughesG.Martincomparison of Depodur, a novel, single-dose extended release epidural morphine, with standard epidural morphine for pain relief after lower abdominal surgeryAnesth Analg100200510651074
- L.N.YaddanapudiJ.WigB.SinghM.K.TewariComparison of efficacy and side effects of epidural tramadol and morphine in patients undergoing laminectomy: a repeated dose studyNeurol India482000398400
- G.BaldiiH.BagryA.AprikianAnesthesiology1105200911391157 May
- Patrick Y.WuethrichFiona C.BurkhardTrends Anaesthesia Crit Care232012138144
- Amira A.ShabanMohamed Abd-AllahAminHoria A.FarranEffect of epidural volume extension on characteristics of bupivacaine spinal block on cesarean deliveryAAMJ1032012 Suppl-2
- V.SouronJ.HamzaTreatment of postdural puncture headaches with colloid solutions: an alternative to epidural blood patchAnesth Analg199913331334 89