Abstract
Background
Several adjuvants can be utilized to improve the quality of peribulbar block (PBB). We compared the effects of adding cisatracurium or hyaluronidase to levobupivacaine and lidocaine mixture for PBB on the onset of globe and lid akinesia in cataract surgery.
Methods
105 adult patients scheduled for cataract surgery under PBB were randomly allocated into three groups. Control group received 4 ml 0.5% levobupivacaine plus 3 ml 2% lidocaine diluted in saline to a total volume of 8 ml. Hyaluronidase 15 IU/ml and cisatracurium 1 mg were added to local anesthetics (LAs) mixture in hyaluronidase and cisatracurium groups respectively. Onset and duration of lid and globe akinesia, time for adequate conditions to start surgery and adverse events were recorded. Distribution of LAs solution was evaluated by B-scan ultrasound at 3 min and 10 min after injection of LAs.
Results
Onset of lid and globe akinesia, as well as time to adequate conditions to start surgery, were faster in cisatracurium and hyaluronidase groups compared to the control group (P < 0.05). Cisatracurium group had the fastest onset. At 3 min after injection of LAs, the ultrasound examination revealed that hyaluronidase group had the highest percentage of patients showing intraconal diffusion of LAs solution with the appearance of a characteristic T sign (P < 0.05).
Conclusions
The addition of cisatracurium 1 mg or hyaluronidase 15 IU/ml to levobupivacaine and lidocaine mixture for PBB hastened the onset of lid and globe akinesia without increase the incidence of adverse effects. This effect is more obvious with cisatracurium compared to hyaluronidase.
Keywords:
1 Introduction
The greater part of patients undergoing cataract surgery is older and has multiple co-morbidities making regional anesthetic a more secure contrasting option to general anesthesia. Due to the simplicity of situation, safety, and efficacy, peribulbar block (PBB) is the most common anesthesia used for cataract surgery [Citation1]. In any case, PBB utilizing local anesthetics (LAs) alone may bring about delayed akinesia, delayed corneal anesthesia and frequent need for block supplementation [Citation2,Citation3]. Subsequently added substances, for example, fentanyl [Citation4], sodium bicarbonate [Citation5], and clonidine [Citation6] are utilized to enhance the onset time and quality of PBB.
Neuromuscular blocking drugs have been utilized in PBB as a part of the local anesthetic (LA) mixture to enhance the quality of the PBB [Citation7,Citation8].
Hyaluronidase is supplemental to LAs for ophthalmic blocks causing a wide spread of the injected solution and improved quality of the block [Citation9,Citation10].
So, the aim of our study was to compare the effects of addition of cisatracurium (1 mg) versus hyaluronidase (15 IU/ml) to the LAs solution for PBB on the onset of globe and lid akinesia in patients undergoing cataract surgery.
2 Patients and methods
After obtaining approval from the Institutional Ethics Committee (approval code: 30940/05/16), registration in the Pan African Clinical Trials Registry (PACTR 201606001658235) on 2 June 2016 and written informed consent from all the patients, a prospective double-blind randomized study was carried out on 105 adult patients, American Society of Anesthesiologists (ASA) I-III, scheduled for elective cataract surgery under PBB. The duration of the study was 6 months. All the data of patients were confidential with secret codes and private file for each patient, all the given data was used for the current medical research only. Any unexpected risks may take place during the course of the research were clarified to the participants and the ethical committee.
Exclusion criteria included; previous allergic reaction to studied medications, mental illness, difficulty in communication, extra-ocular muscles or eyelid abnormalities, age younger than 18 years, patients refusing local anesthesia, patients with a single eye, hepatic dysfunction, anticoagulation therapy, active infection, posterior synechia, orthopnea, or severe uncontrolled hypertension, previous intraocular surgery or injury, and patient with ocular axial length more than 25 mm.
The patients were randomized using a computer-generated randomization numbers into the three groups by using sealed opaque envelopes and each patient chose the envelope which determined the group in which the patient was allocated.
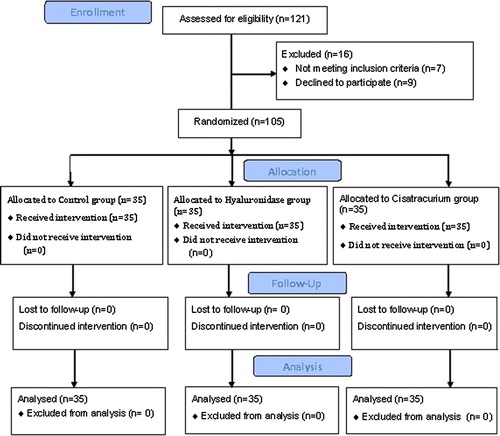
Out of 121 patients were evaluated for the eligibility; 7 patients were not met the inclusion criteria (one patient had a single eye, 2 patients were difficult to comminute, one patient had ocular axial length >25 mm and 3 patients were receiving anticoagulant therapy), 9 patients refused to participate in our study and the remaining 135 patients were randomly allocated into one of three groups (each group was 35 patients) (see ).
The studied groups were:
Control group: Patients received single injection PBB using 4 ml 0.5% levobupivacaine plus 3 ml 2% lidocaine diluted in saline to a total volume of 8 ml.
Hyaluronidase group: Patients received single injection PBB using 4 ml 0.5% levobupivacaine plus 3 ml 2% lidocaine plus hyaluronidase (15 IU/mL) diluted in saline to a total volume of 8 ml.
Cisatracurium group: Patients received single injection PBB using 4 ml 0.5% levobupivacaine plus 3 ml 2% lidocaine plus cisatracurium (1 mg) diluted in saline to a total volume of 8 ml.
The study solution for PBB was prepared by an investigator who has no further role. All patients were sedated with intravenous midazolam (0.03 mg/kg), 5 min before the PBB, in the preparation room. Then they transferred to the operating room. Standard monitoring was conducted; noninvasive arterial blood pressure, electrocardiogram, and peripheral oxygen saturation. A nasal catheter was applied and supplemental oxygen was given throughout the procedure at 2–3 L/min. The operative eye was prepared with a 5% povidone iodine solution. PBB was performed using a single-injection transcutaneous technique [Citation11]. PBB was performed by a senior anesthetist experienced in the technique who was blinded to the kind of LAs solution used. The injection was carried out using a needle (25G) with the length of 25 mm. The globe was maintained in a neutral gaze position. The injection site was identified at the junction of the lateral one-third and medial two-third of the inferior orbital rim in the infero-temporal quadrant. The needle was advanced in an antero-posterior, slightly medial, and cephalad direction in the direction of the optical foramen. The patient was asked to look left, then right to notice free motility and exclude globe perforation. After the aspiration; to be certain that there would be no blood in the aspiration; the LAs solution was injected until the presence of a complete drop and fullness of the upper eyelid. A Honan’s cuff was immediately applied to the eye and inflated to 30 mmHg to produce intermittent compression for a total of 10 min. The cuff was deflated during assessments.
The primary outcome of our study was the onset of globe and lid akinesia. The secondary outcomes were the assessment of LAs distribution by B- scan ultrasound, duration of motor and sensory block and the incidence of side effects.
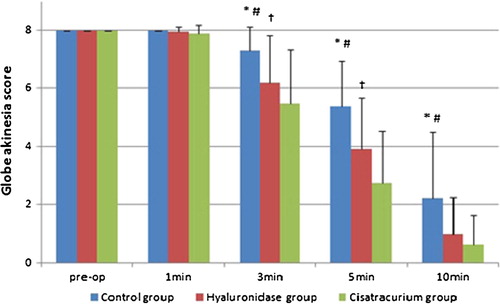
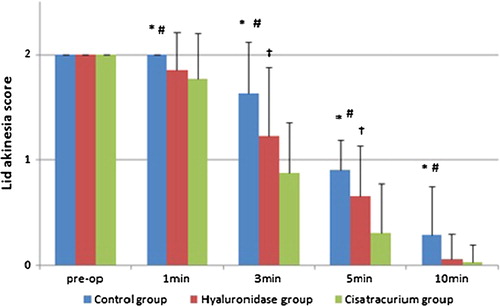
The ocular motility and the eyelid akinesia were evaluated before performing PBB, then at 1 min, 3 min, 5 min, and 10 min after performing the PBB. The eyelid akinesia was evaluated by asking patients to open the eyelids (the levator palpebrae muscle) then squeezing (orbicularis oculi) them. The 4 rectus muscles of the eye and the lid akinesia were evaluated individually using a 3-point scoring system [Citation12], which was categorized as follow: 0 = akinesia, 1 = partial akinesia, and 2 = normal movement. The sum of globe akinesia score in the four cardinal directions ranged from 0 to 8. The onset of corneal anesthesia was evaluated by loss of the corneal reflex.
Time for adequate conditions to start the surgery was defined as the presence of corneal anesthesia and total globe akinesia ≤4 with no eyelid squeezing. If a PBB was inadequate for surgery at 10 min after initial injection, then additional injection with 3 ml of the anesthetics drug mixture was injected according to the site of akinesia. The total volume of LAs solution injected (ml) was noted. B-scan ultrasound was done to evaluate the localization of LAs solution in the eye. The sonic evaluation was done before injection of LAs, then at 3 min and 10 min after injection of LAs. The major axis of the optic nerve was taken as a reference for ultrasonic evolution. The end point of the ultrasonic examination was the appearance of 'T sign' which formed by the hypoechogenic LA fluid together with the hypoechogenic optic nerve. All ultrasonic evaluation was done by the same ophthalmologist who was blinded to the LA mixture used for the block.
The duration of akinesia was assessed by the recovery of ocular and eyelid movements. During the postoperative period, ocular and eyelid movements were assessed every 30 min until recovery. Postoperative pain was evaluated by utilizing a 5-points verbal rating score (VRS) (0-no pain, 1-mild pain, 2-moderate pain, 3-severe pain, 4-unbearable pain). The pain was evaluated at the end of surgery and every hour up to 2 h and then at 4 h, 6 h and 8 h. Paracetamol tablet 500 mg was given if VRS was ≥2. The time to the first request for analgesic was documented. The incidence of any complications which may be ophthalmic (such as globe perforation, pain on injection and the feeling of back pressure in the eye) or non ophthalmic (such as bradycardia, hypotension, brainstem anesthesia, drowsiness, nausea, vomiting and dizziness) was recorded. The assessments were performed by an investigator who was blinded to the kind of LAs solution used.
Statistical analysis: Calculation of sample size was depended on the onset of globe akinesia. Based on the results of previous studies [Citation13], at least 28 patients were needed to detect the significant difference in the onset of globe akinesia of 1.2 min between groups at α level of 0.05 and the study power of 80%. We utilized SPSS 16 (SPSS Inc., Chicago, IL, USA) for statistical analysis. Numerical data was described as mean ± SD and were analyzed utilizing One-way ANOVA with post hoc Turkey's HSD Test. Kruskal–Wallis test was utilized to analyze and compare postoperative VRS among the studied groups. Categorical data were described as number (n) or percentage (%) and were compared among groups utilizing the Chi-square. Comparison of the numerical data within each group was performed utilizing repeated measures analysis of variance while the non parametric data were analyzed utilizing the Wilcoxon signed-rank test. P-value < 0.05 was considered significant.
3 Results
Each group was composed of 35 patients. Demographic data included age, gender, ASA physical status and body weight were comparable among the three studied groups (P > 0.05) (see ).
Table 1 Demographic data and perioperative patient s' characteristics.
The onset of corneal anesthesia was faster in hyaluronidase group as compared to the other two groups (P < 0.05). Comparison between the control group and cisatracurium group was not statistically different (P > 0.05) (see ).
Table 2 Criteria of the peribulbar block in the three groups; data presented as mean ± SD.
The onset of globe akinesia was faster in cisatracurium group and hyaluronidase group as compared to the control group (P < 0.05). Cisatracurium group had the fastest onset of globe akinesia versus the control group (P < 0.05) and versus hyaluronidase group (P < 0.05) (see ).
Onset of lid akinesia in the three groups was shown in .
Pre-operative globe akinesia score was comparable among the three groups. At 3 min, 5 min and 10 min after PBB, globe akinesia score was significantly lower in cisatracurium group and hyaluronidase group as compared to control group (P < 0.05). Globe akinesia score of cisatracurium group was lower than that of hyaluronidase group (P < 0.05) at 3 min and 5 min after PBB but it was insignificantly different at 10 min after the PBB (P > 0.05) (see ).
Pre-operative lid akinesia score was not significantly different among the three groups. At 1 min, 3 min, 5 min and 10 min after PBB, lid akinesia score was lower in cisatracurium group and hyaluronidase group as compared to the control group (P < 0.05). Lid akinesia score of cisatracurium group was lower than that of hyaluronidase group (P < 0.05) at 3 min and 5 min after PBB but it was insignificantly different at 1 min and 10 min after the PBB (P > 0.05) (see ).
Cisatracurium group provided the fastest time for adequate conditions to start surgery as compared to hyaluronidase group and control group (P < 0.05) (see ).
The number of patients needed supplemental injections of LAs mixture in control group (12 patients) was higher than those of hyaluronidase group (2 patients) and cisatracurium group (1 patient) (P < 0.05).
B-scan ultrasound examination of the eye after injection of LAs solution demonstrated that the LAs solution was seen either in the extraconal fat, sub-tenon's space (b) or intraconal (c). At 3 min after the injection of LAs solution, B-scan ultrasound examination demonstrated that intraconal distribution with the appearance of a characteristic T sign (c) was detected in 18 patients (51.4%) in hyaluronidase group, and 9 patients (25.7%) and 8 patients (22.9%) in cisatracurium and control groups respectively (P = 0.02). At 10 min, T sign was detected in 32 patients (91.4%) in hyaluronidase group, and 28 patients (80%) and 27 patients (77.1%) in cisatracurium and control groups respectively (P > 0.05).

Duration of lid and globe akinesia and time to the 1st analgesic request were comparable among the three groups (P > 0.05) (see ).
Postoperative VRS was comparable among the three groups at all times of assessment (P > 0.05) (see ).
The incidence of pain on injection and dizziness was comparable among the three groups (P = 0.873 and 0.601 respectively) (see ).
4 Discussion
PBB consists of introducing LA solution into the extraconal space of the orbit [Citation14]. The LA solution should be spread inside the intraconal space to provide adequate anesthesia and akinesia of the globe [Citation15].
The results of our research showed that the addition of cisatracurium to LAs solution for PBB provided better akinesia score and hastened the optimal condition for initiation of surgery than the control and hyaluronidase groups. In addition, the utilization of cisatracurium as a part of LAs solution decreased the need for block supplementation. Postoperative analgesia was comparable between the groups. No side effects related to systemic absorption of cisatracurium were noticed. The mechanism of muscle relaxant to improve the akinesia when utilized as a part of LAs solution for PBB is still unclear but it may be explained by the local direct effects at the muscles motor end-plate or through interfering with muscle spindle activity results in decreased muscle tone and spasm [Citation16].
Despite the used dose of cisatracurium was less than 1/10 of the standard dose of cisatracurium needed for intubation, nonetheless, the risk of inadvertent intravascular injection during PBB with LAs containing cisatracurium was the main adverse effects.
Our results as regard the effects of addition of cisatracurium to LAs solution for PBB are on line with the results of Mehrdad et al. [Citation17] who compared the effects of utilizing atracurium (5 mg) versus cisatracurium (1 mg) as a part of LAs solution (marcaine 0.5%, lidocaine 2% and hyaluronidase 90 IU with the volume of 8 ml) for PBB among patients underwent cataract surgery. They concluded that the addition of cisatracurium (1 mg) or atracurium (5 mg) to LA solution improved the quality of akinesia and hastened the onset of akinesia. Messeha et al. [Citation13] studied the effect of addition of rocuronium or hyaluronidase to the LA solution (lidocaine 2%) for PBB on orbital muscle akinesia in 60 patients underwent cataract surgery and they concluded that the addition of rocuronium to lidocaine 2% for PBB provided optimal globe akinesia with a faster adequate conditions to start surgery than that of hyaluronidase.
The effects of the utilizing other muscle relaxants such as atracurium [Citation8,Citation18], rocuronium [Citation7,Citation13,Citation19], and vecuronium [Citation20] as a part of LAs solution for PBB were studied in previous studies.
In our study, the addition of hyaluronidase (15 IU/mL) improved the quality and the onset of PBB as compared to the control group. At 3 min after injection of LAs solution, B-scan ultrasound examination demonstrated that hyaluronidase group had the highest percentage of patients showing intraconal diffusion of the LAs solution. Hyaluronidase performs its action through promoting the depolymerisation of hyaluronic acid to a tetrasaccharide. So it causes breakdown the interstitial cell barriers that enhances the diffusion and improves the efficacy of local LA [Citation21].
The beneficial effects of addition of hyaluronidase to LA solution for PBB are a matter of controversy. Some studies had documented the improvement the quality of ocular akinesia with the utilization of hyaluronidase as a part LA solution for PBB [Citation22–Citation25]. While other studies failed to prove this effects [Citation26,Citation27,Citation21,Citation28].
Localization of the LAs solution following PBB was evaluated in the three groups by using B-scan ultrasound. LAs solution was seen either in the extraconal fat, sub-tenon's space or intraconal. Luyet et al. [Citation29] studied the diffusion of LA solution during the injection of the LA (real time) for PBB by using B-scan ultrasound in 100 patients scheduled for posterior segment surgical interventions and they assessed the incidence of intraconal spread of LA during drug injection for PBB. They demonstrated that instantaneous intraconal diffusion of LA occurred in 61 patients. El Said et al. [Citation30] used B-scan ultrasound to compare the distribution of LAs after classic peribulbar versus single percutaneous injection technique. Initially, they found difficulty to localize the peribulbar LAs then they observed it in the orbital fat posterior to the globe. After 10 min, they found the LAs solution diffused intraconal. Winder et al. [Citation31] studied the localization and distribution of LA solution during sub-Tenon's, peribulbar, and retrobulbar techniques for phacoemulsification by using Kinetic echography during drug administration and B-scan ultrasound examination at 10 min after drug injection. They identified the LA solution for PBB initially in the extraconal fat and at 10 min later the LA identified intraconal.
5 Conclusions
The addition of cisatracurium 1 mg or hyaluronidase 15 IU/ml to LAs solution for PBB hastened the onset of lid and globe akinesia with a faster adequate condition to start surgery as compared to the control group without increased the incidence of adverse effects. This effect is more obvious with cisatracurium compared to hyaluronidase
Funding
The study was funded by Departmental Resources.
Conflicts of interest
None.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- A.P.RubinComplications of local anesthesia for ophthalmic surgeryBr J Anaesth7519959396
- D.H.WongRegional anesthesia for intraocular surgeryCan J Anaesth401993635657
- T.VetteseC.W.BreslinRetrobulbar anesthesia for cataract surgery: comparison of bupivacaine and bupivacaine/lidocaine combinationsCan J Ophthalmol201985131134
- M.YoussefK.GirgisS.M.SoaidaClonidine versus fentanyl as adjuvants to bupivacaine in peribulbar anesthesiaEg J Anaesth302014267272
- J.E.RobertsB.A.MacLeodR.H.HollandsImproved peribulbar anesthesia with alkalinization and hyaluronidaseCan J Anaesth401993835838
- N.BhartiR.MadanH.L.KaulS.K.KhokharS.MishraEffect of addition of clonidine to local anaesthetic mixture for peribulbar blockAnaesth Intensive Care302002438441
- Y.AissaouiL.BelyamaniN.D.KamiliEffect of the addition of rocuronium to local anesthetics for peribulbar blockActa Anaesthesiol Belg6120105154
- Z.KüçükyavuzM.K.AriciEffects of atracurium added to local anesthetics on akinesia in peribulbar blockReg Anesth Pain Med272002487490
- D.WatsonHyaluronidaseBr J Anaesth711993422425
- J.M.NicollB.TreurenP.A.AcharyaK.AhlenM.JamesRetrobulbar anesthesia: the role of hyaluronidaseAnesth Analg65198613241328
- A.ApelR.WoodwardSingle-injection peribulbar local anaesthesia – a study of fifty consecutive casesAust NZ J Ophthalmol191991149153
- P.SarvelaM.D.JohannaComparison of regional ophthalmic anesthesia produced by pH-adjusted 0.75% and 0.5% bupivacaine and 1% and 1.5% etidocaine, all with hyaluronidaseAnesth Analg771993131134
- M.M.MessehaA.E.ElhesyComparison of orbital muscle akinesia caused by rocuronium versus hyaluronidase mixed to the local anesthetic in single injection peribulbar block for cataract surgeryAnesth Essays Res932015374378
- D.B.Davis2ndM.R.MandelPosterior peribulbar anesthesia: an alternative to retrobulbar anesthesiaJ Cataract Refract Surg121986182184
- E.NouvellonP.CuvillonJ.RipartRegional anesthesia and eye surgeryAnesthesiology113201012361242
- F.SztarkM.ThiocoipeJ.F.Favarel-GarriguesP.LassieM.E.PetitjeanP.DabadieThe use of 0.25% lidocaine with fentanyl and pancuronium for intravenous regional anesthesiaAnesth Analg841997777779
- M.GodarziS.BeyranvandS.ArbabiM.SharoughiR.MohtaramA.E.SoltaniComparing the effect of using atracurium and cis-atracurium as adjuvant agents to the local anesthetic substance on peribulbar-induced akinesiaActa Med Iran4982011509512
- M.H.EghbalT.HesamatT.ShojaaR.R.MohammadThe effect of addition of low dose atracurium to local anesthetic in retrobulbar block for cataract surgeryMiddle East J Anasthiol2042010535538
- A.A.AbdellatifM.A.El ShahawyA.I.AhmedW.A.AlmarakbiJ.A.AlhashemiEffects of local low dose rocuronium on the quality of peribulbar anesthesia for cataract surgerySaudi J Anaesth542011360364
- G.ReahA.R.BodenhamP.BraithwaiteJ.EsmondM.J.MenagePeribulbar anaesthesia using a mixture of local anaesthetic and vecuroniumAnaesthesia5361998551554
- R.J.BowmanD.K.NewmanE.C.RichardsonA.B.CallearD.W.FlanaganIs hyaluronidase helpful for peribulbar anaesthesia?Eye111997385388
- H.KallioM.PaloheimoE.MaunukselaHyaluronidase as an adjuvant in bupivacaine–lidocaine mixture for retrobulbar/peribulbar blockAnesth Analg912000934937
- J.SarvelaP.NikkiHyaluronidase improves regional anaesthesia with etidocaineCan J Anaesth391992920924
- G.A.DempseyP.J.BarretI.J.KirbyHyaluronidase and peribulbar blockBr J Anaesth781997671674
- C.MantovaniA.E.BryantG.NicholsonEfficacy of varying concentrations of hyaluronidase in peribulbar anaesthesiaBr J Anaesth862001876878
- M.CrawfordW.KerrThe effect of hyaluronidase on peribulbar blockAnaesthesia491994907908
- D.P.ProsserG.E.RodneyT.MianH.M.JonesM.Y.KhanRe-evaluation of hyaluronidase in peribulbar anaesthesiaBr J Ophthalmol801996827830
- C.W.BrydonM.BaslerW.J.KerrAn evaluation of two concentrations of hyaluronidase for supplementation of peribulbar anaesthesiaAnaesthesia5019959981000
- C.LuyetK.T.EngP.J.KertesA.AvilaR.H.MuniP.McHardyReal-time evaluation of diffusion of the local anesthetic solution during peribulbar block using ultrasound imaging and clinical correlates of diffusionReg Anesth Pain Med3742012455459
- T.M.El SaidM.M.KabeelComparison of classic peribulbar anesthesia and new entry point (single percutaneous injection technique) in vitroretinal surgerySaudi J Anaesth4220108085
- S.WinderS.WalkerH.R.AttaUltrasonic localization of anaesthetic fluid in sub-Tenon’s, peribulbar and retrobulbar techniquesJ Cataract Refract Surg2519995659