ABSTRACT
Background: Rapid shallow breathing index (RSBI) is a well-known weaning index. However; its diagnostic performance is less than satisfactory. Recently, diaphragmatic rapid shallow breathing index (DRSBI) is proposed as a promising tool in weaning outcome prediction. The aim of this study was to evaluate if DRSBI is more accurate than RSBI for weaning outcome prediction.
Patients and methods: This prospective, randomized clinical trial was carried out on 106 mechanically ventilated patients for more than 48 h and ready to wean at their first spontaneous breathing trial (SBT). After one minute of SBT, RSBI and DRSBI were calculated. According to the decision to continue SBT patients were divided into: Group I (53 patients) the decision depends on the RSBI. Group II (53 patients) the decision based on DRSBI. 30 min later, patients were reevaluated for tolerance of SBT then RSBI and DRSBI were calculated. Outcome of the weaning attempt was recorded and ROC analysis was done to evaluate the diagnostic accuracy.
Results: 106 patients were enrolled. Trauma was the commonest diagnosis on ICU admission and traumatic brain injury was the main indication for initiation of mechanical ventilation in the two groups. 33 patients (31.1%) failed to wean (19 patients in group I and 14 patients in group II). RSBI at 1 min and 30 min as well as DRSBI at 1 min and 30 min were highly statistical significant higher in weaning failure patients. RSBI and DRSBI at 30 min were highly statistical significant increased compared to at 1 min. DRSBI at 30 min was the parameter with the best diagnostic accuracy for predicting weaning success with a cutoff value <1.6 breaths/min/mm.
Conclusion: DRSBI has a better diagnostic accuracy than the traditional RSBI in predicting weaning outcome specially when monitored at 30 min from the start of SBT.
Trial registration: this clinical trial was registered with ClinicalTrials.gov (NCT03561792)
1 Introduction
Minimizing the duration of mechanical ventilation (MV) is of a paramount importance for all critical care physicians. Therefore, deciding the appropriate time of weaning from MV is crucial as delayed weaning and extubation is associated with longer intensive care unit (ICU) stay, inappropriate utilization of health care resources, and greater morbidity and mortality [Citation1–Citation3].
Although rates of weaning and extubation failure differ considerably among ICUs, Approximately 15% of patients in whom mechanical ventilation is discontinued require reintubation within 48 h. Consequently, it is fundamental for critical care physicians to differentiate between readiness for discontinuation of ventilation and successful spontaneous breathing trials [Citation4].
The rapid shallow breathing index (RSBI), calculated from respiratory rate divided by tidal volume (RR/VT), is a well-known weaning index and one of the most clinical indices used to predict weaning outcome. However, it has some limitations in predicting weaning outcomes [Citation5]. Several previous studies have defined different sensitivities and specificities for RSBI less than 105 to predict weaning success which may lead to errors in predicting successful weaning [Citation6–Citation8].
On the other hand, weaning failure is likely to occur if there is an imbalance between the load on the inspiratory muscles and their neuromuscular capacity, the imbalance between the mechanical load imposed on the diaphragm which is the major muscle of inspiration and its ability to cope with it. Therefore, evaluating the function of diaphragm before any weaning trial could be useful in predicting weaning outcome [Citation9].
Bedside ultrasonography is an easy, fast, noninvasive, and accurate maneuver for evaluating diaphragmatic function. Diaphragmatic displacement (DD) reflecting the ability of diaphragm to produce force and subsequently tidal volume during inspiration and defined as displacement of less than 10 mm has been found to be a predictor of weaning failure among patients in medical ICUs [Citation5,Citation10].
Spadaro et al. proposed that Diaphragmatic Rapid shallow breathing index (RR/DD) is a more accurate index than the traditional RSBI for prediction of weaning outcome from mechanical ventilation [Citation5].
The aim of this study was to evaluate the accuracy of the new index DRSBI compared to traditional RSBI for predicting successful weaning in ready to wean patients.
2 Patients and methods
2.1 Study population and design
This prospective, randomized clinical trial was carried out on one hundred and six patients admitted to Surgical Intensive Care Unit, Zagazig University Hospitals from December 2017 to July 2018 and it was done after approval of Institutional Review Board (IRB) and the patient’s or relatives’ written informed consent was obtained. Our clinical trial was registered with ClinicalTrials.gov (NCT03561792).
All patients included in this study aged more than 18 years and were intubated and mechanically ventilated for more than 48 h. They were ready to wean at their first spontaneous breathing trial (SBT) meeting all the following weaning criteria: clinically resolved underlying cause for initiation of mechanical ventilation, FiO2 ≤ 40%, positive end-expiratory pressure (PEEP) level ≤ 5 cmH2O, respiratory rate ≤ 30 cycle/min, PaO2/FiO2 ratio ≥ 200 mmHg, and hemodynamic stability (heart rate ≤ 100 beat/min and mean arterial pressure ≥ 65 mmHg) in the absence or minimal dose of vasopressors (e.g. Norepinephrine ≤ 0.05 µg/kg/min), normal levels of electrolytes, blood glucose, hemoglobin level ≥ 10gm/dl, and normal body temperature < 38 °C. Minimal dose of sedatives and analgesics was allowed to keep the patient calm and cooperative with the Richmond Agitation Sedation Scale (RASS) score range ±1 [Citation11].
Patients with a history of any neuromuscular disease, diaphragmatic palsy, cervical injury, or with a current chest trauma i.e. pneumothorax, rib fracture, flail chest, or thoracotomy for any reason were excluded from the study. Also, patients in whom neuromuscular blockers were used in the last 48 h before the study as well as patients for whom aminoglycosides were prescribed during their course in ICU were excluded from the study.
Patient assessment:
Patients were included when they fulfill all weaning criteria mentioned above and undergo their first SBT that consists of pressure support ventilation (PSV) trial by decreasing PSV to 5–8 cmH2O with 5 cmH2O or less positive end-expiratory pressure (PEEP). The ICU team on charge takes the decision about the readiness for weaning and the time to initiate the SBT.
After one minute of PSV trial, traditional RSBI was calculated from the tidal volume (VT) delivered by the ventilator and respiratory rate (RR) as RR/VT (in liters) and diaphragmatic ultrasound was performed to obtain diaphragmatic displacement (DD) and calculate the DRSBI as RR/DD (in mm).
According to the decision to continue weaning trial patients were randomly allocated by a computer-generated randomization table into two groups:
Group I (53 patients): The ICU team on charge takes the decision to continue SBT according to the local practice protocols which depends on the traditional RSBI (RSBI < 105 predicts successful weaning). The ICU team wasn’t allowed to know the results of diaphragmatic ultrasound.
Group II (53 patients): The investigator takes the decision about SBT continuation based on the result of DRSBI (DRSBI < 1.3 predicts successful weaning) [Citation5]. The investigator was blinded about the result of traditional RSBI.
30 min later, patients of both groups were reevaluated for tolerance of SBT then traditional RSBI and diaphragmatic ultrasound were repeated with calculation of DRSBI.
The decision to extubate the patients of both groups was performed if the following criteria are satisfactory after 120 min SBT: good tolerance to SBT with respiratory rate < 30 cycle/minute, hemodynamic stability (heart rate and blood pressure variability ≤ 20% of baseline), oxygen saturation ≥ 90%, and absence of increased work of breathing, conscious level (GCS ≥ 10), adequate cough reflex and, scanty tracheobronchial secretions [Citation12].
Weaning success was defined as the ability of the patient to maintain his or her own breathing for at least 48 h without any level of ventilatory support. While weaning failure is the inability to maintain spontaneous breathing for at least 48 h, Patients who required reintubation or noninvasive positive pressure ventilation within 48 h of discontinuation of MV were considered failed to wean [Citation13]. Reintubation decision or the decision to use noninvasive ventilation were left up to the ICU team.
2.1.1 Measurement of diaphragmatic displacement
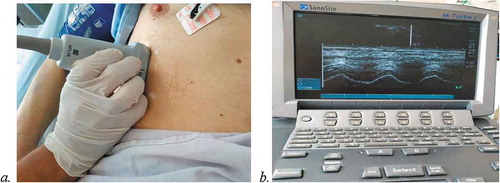
In the semi-sitting position with the head of bed elevated at an angle between 30° and 45° ultrasonography for diaphragmatic displacement were performed by the same intensivist who had a good experience in diaphragmatic sonography.
Diaphragmatic movement was evaluated by using 2–5 MHz US probe (Sonosite M-Turbo machine). The right hemidiaphragm was examined by two-dimensional (2D) and M-mode to record diaphragm excursion (displacement). The probe was placed immediately below the right costal margin in the midclavicular line in longitudinal scanning plane with the angle in cephalad direction to make the ultrasound beam perpendicular to the posterior third of the right hemidiaphragm and with the liver serving as an acoustic window, a two-dimensional mode was used to identify the line of the right hemidiaphragm. Then in M-mode, the diaphragmatic displacement (cm) was measured on the vertical axis tracing from the beginning to end of inspiration () [Citation14,Citation15].
2.2 Sample size calculation
Sample size was calculated by EPI info program at power of test 80% and confidence interval 95% after a conduction of a pilot study which revealed that the mean of DRSBI in weaning success patients was 1.2 ± 0.93, while in weaning failure patients was 1.7 ± 0.9, so the sample size was 106 patients, 53 patients in each group.
2.3 Statistical analysis
Data collected throughout the study were coded, entered and analyzed using Microsoft Excel software. Data were then imported into Statistical Package for the Social Sciences (SPSS version 20.0) (Statistical Package for the Social Sciences) software for analysis. Qualitative data were represented as number and percentage, while quantitative data were represented by mean ± SD; the following tests were used to test differences for significance; difference and association of qualitative variable by Chi square test (X2). Differences between quantitative independent groups by t-test or Mann Whitney, multiple by ANOVA or Kruskal Wallis correlation by Pearson’s correlation or Spearman’s. P value was set at <0.05 for significant results & <0.001 for high significant results.
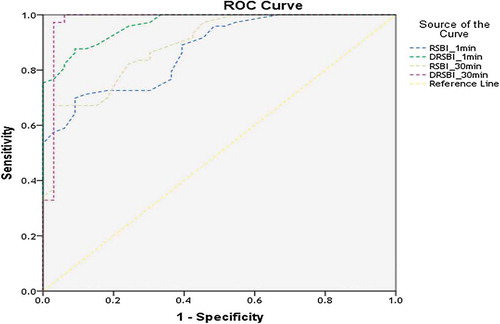
The accuracy of DRSBI and RSBI for predicting weaning outcome was studied using receiver operator characteristic (ROC) curves. For each ROC curve, the accuracy, sensitivity, specificity, positive and negative predictive values were calculated as well as the optimal cut-off point of DRSBI and RSBI with maximal sensitivity and specificity for predicting weaning success.
3 Results
There were no statistically significant differences between the patients’ characteristics (age, weight, height, and sex) ().
Table 1 Patients’ characteristics among the studied groups.
Trauma was the commonest diagnosis in both groups followed by sepsis and postoperative care for major surgeries (e.g. craniotomy). Traumatic brain injury (TBI) was the main indication for initiation of mechanical ventilation in the two groups followed by sepsis due to other causes than pneumonia (e.g. fecal fistula, surgical site infection) then postoperative respiratory failure and pneumonia. Statistically the two groups did not differ significantly as regard the diagnosis on ICU admission and the indications of mechanical ventilation ().
Table 2 Diagnosis on ICU admission and indications of mechanical ventilation among the studied groups.
A total of 33 patients (31.1%) in the two groups failed to wean and required ventilatory support within 48 h after extubation. They were 19 patients in group I versus 14 patients in group II while there were 73 patients (68.9%) shows weaning success (34 and 39 patients in group I and II respectively) ().
Table 3 Weaning failure and success in the two studied groups.
There was no statistical significant difference among both groups regarding the mean ventilatory hours till SBT (). Also, no statistically significant differences in the association between weaning failure in each group and patients’ pre-weaning data were detected, except for sepsis which was associated with a significant difference in both groups ().
Table 4 The ventilator hours till SBT in the studied groups.
Table 5 the association with weaning failure in each group.
The ventilator hours till SBT, RSBI at 1 min and 30 min as well as DRSBI at 1 min and 30 min in weaning failure patients were statistically high significant different than in weaning success patients in each group. They were higher in weaning failure patients while the DD was statistically high significant different as it was lower in weaning failure patients ().
Table 6 Comparison between weaning success and failure in each group.
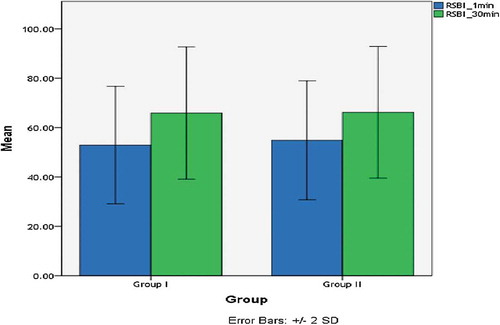
On assessing the change of RSBI and DRSBI at 1 min and 30 min in each group they were markedly increased at 30 min showing high significant difference ().
The overall results of the Receiver operating characteristic (ROC) analysis of RSBI and DRSBI at 1 and 30 min. for predicting weaning outcome showed that DRSBI at 30 min resulted in the parameter with the best diagnostic accuracy for predicting weaning success with a cutoff of DRSBI < 1.6 breaths/min/mm at 30 min. yielded 97.3% sensitivity, a specificity of 93.9% specificity, 97.1% positive predictive value (PPV), 93.9% negative predictive value (NPV) and 96.2% accuracy (, ).
Table 7 Accuracy of RSBI and DRSBI at 1 and 30 min in predicting weaning success.
4 Discussion
Determining the optimal timing to wean and extubate a critically ill patient is still a challenging process. As, both early and delayed weaning are linked to a lot of complications including higher mortality and increased ICU length of stay [Citation16]. Weaning outcome may be affected by several factors such as hemodynamic stability, muscle weakness, electrolyte imbalances, pulmonary function, and the ability of the patient to generate a good cough and expectorate endotracheal secretions [Citation17]. As a consequence, single weaning index is insufficient to make an accurate decision about the prediction of the outcome. Multiple indices and parameters have been proposed as predictors but the prognostic accuracy of these indices is still questioned [Citation18,Citation19].
RSBI which depends on the ratio between RR and VT with a cutoff value of 105 to predict weaning failure is now widely used in clinical practice. In contrast to the original study of Yang and Tobin [Citation20] our results showed that weaning failure patients had a lower RSBI at 1 min it was 63.68 ± 10.99 and 66.78 ± 12.3 in group I and II respectively and at 30 min it was 78.94 ± 9.6 in group I and 78.64 ± 14.2 in group II. The predictive value of RSBI was variable in different studies that could be attributed to differences in study populations, ventilator settings, underlying illness, body position, and size of endotracheal tube [Citation21–Citation26].
It was reported that RSBI is not a good predictor for patients whose primary problem was related to poor cough, increased secretions and compromised airway protection [Citation27,Citation28]. Also, early measured RSBI was inaccurate in predicting weaning success in chronic obstructive pulmonary disease patients [Citation29].
The results of the present study showed that there was a significantly higher RSBI measured at 30 min compared to that at 1 min. Patients may show a normal breathing pattern at the beginning of a SBT, but later on deterioration can occur. In the study conducted by Chatila et al they found that RSBI measured at 30 min after initiation of SBT was superior to that measured at the start of the SBT as a weaning predictor [Citation30]. Another study by Krieger et al, they concluded that serial measurement of RSBI was more consistent to predict weaning outcomes [Citation24]. Kuo et al, also found that RSBI measured at the end of SBT had better diagnostic accuracy [Citation31]. Segal et al demonstrated that the percent change of RSBI during SBT was better in predicting the weaning outcome [Citation32].
Therefore, assessing the change in RSBI as a marker of the dynamic changes that occur during weaning could improve the ability to predict weaning outcome but the relationship between RSBI and inspiratory muscle fatigue is still questioned. As, this index reflects the involvement of all inspiratory muscles, not only the diaphragm. So, diaphragmatic dysfunction could be hidden by other inspiratory muscles compensation [Citation33].
Many studies have shown that diaphragmatic dysfunction could lead to weaning failure. Thus, an early diagnosis of diaphragmatic dysfunction is compulsory to avoid weaning failure. Recently, diaphragmatic ultrasound has emerged as a safe bed-side tool for assessing diaphragmatic excursion and thickening fraction that could reflect diaphragmatic function and predict weaning outcome [Citation34].
Spadaro et al proposed that substituting VT in calculation of RSBI by DD producing a new index DRSBI could be better than the traditional RSBI and they found that the DRSBI was more accurate because DD strongly reflects the diaphragmatic function compared to VT [Citation5].
In this study, we investigated the diagnostic accuracy of DRSBI as a predictor of weaning outcome and we attempted to investigate the timing of diaphragmatic function assessment and calculation of DRSBI which has the best diagnostic performance.
Our results support the evidence that the new index DRSBI is superior to traditional RSBI in predicting weaning outcome with a cutoff of DRSBI < 1.6 breaths/min/mm monitored at 30 min. with the best diagnostic accuracy for predicting weaning success. Although, the cutoff value for the DRSBI reported by Spadaro et al was lower (1.3) [Citation5] and the cutoff value reported by Abbas et al was higher (1.9) [Citation35]. This could be attributed to the difference in the study population, Spadaro et al study was carried out on mixed medical and surgical ICU patients [Citation5] while Abbas et al study included only chronic obstructive pulmonary disease (COPD) patients [Citation35] and the present study included trauma and surgical critically ill patients. Also, the method of performing the SBT which was different in the three studies could add an explanation, as in our study SBT was done by PSV trial while in Spadaro et al and Abbas et al trials SBT was performed by spontaneous ventilation through a T-tube circuit [Citation5,Citation35].
Our results also confirm that assessing the dynamic changes in the diaphragmatic function over time during SBT could have a better predictive value over a single measurement at the start of SBT that need a further studies on larger populations to be verified.
Several limitations of our study should be addressed. First, data on DRSBI are still scarce compared to traditional RSBI in ICU. Second, to the best of our knowledge, there is no report on the timing of DRSBI calculation and its impact on weaning outcomes. Ultrasound assessment timing may affect the diaphragmatic displacement change. Third, both trauma and surgical critically ill patients were included without focusing on specific disease pathology to evaluate diaphragmatic displacement and DRSBI so, further research regarding ultrasonographic evaluation of diaphragm and DRSBI evaluation in different pathologies such as sepsis, prolonged ventilation, and ICU myopathy are anticipated with great interest. Last, the cutoff of DRSBI (1.6) for predicting weaning success we found in our patients requires validation in large-scale studies.
One of the strengths in our study was the inclusion of traumatic brain injury patients, considering improved conscious level (GCS ≥ 10) and no airway compromise so, we could evaluate the respiratory mechanics to predict weaning outcome in these patients.
5 Conclusion
We conclude that using DRSBI to guide clinical decision about patient liberation from mechanical ventilation has a better diagnostic accuracy than the traditional RSBI in predicting weaning outcome specially when monitored at 30 min from the start of SBT. A cutoff value of 1.6 is associated with the best diagnostic accuracy. Further large prospective randomized controlled studies are warranted to assess if these findings hold true in a larger number of patients with different disease pathologies.
6 Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Kulkarni AP, Agarwal V. Extubation failure in intensive care unit: predictors and management. Indian J Crit Care Med 2008;12(1):1.
- Peñuelas O, Frutos-Vivar F, Fernández C, Anzueto A, Epstein SK, Apezteguia C, et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med 2011;184(4):430–7.
- Thille AW, Harrois A, Schortgen F, Brun-Buisson C. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med 2011;39(12):2612–8.
- McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med 2012;367:2233–9.
- Spadaro S, Grasso S, Mauri T, Dalla Corte F, Alvisi E, Raggazi R, et al. Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? the role of diaphragmatic rapid shallow breathing index. Criti Care 2016;20(1):305.
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445–50.
- Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequencytidal volume ratio) did not predict extubation outcome. Chest 1994;105(2):540–3.
- Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care 2018;6:6.
- Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrello A. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med 2017;43:29–38.
- Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 2011;39(12):2627–30.
- Yoo J-W, Lee SJ, Lee JD, Kim HC. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med 2018;33(2):331–9.
- Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033–56.
- MacIntyre NR, Cook DJ, Ely Jr EW, Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001;120:375–95.
- Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by M-mode ultrasonography: methods, reproducibility, and normal values. Chest 2009;135(2):391–400.
- Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F, et al. Sonographic evaluation of the diaphragm in critically ill patients: technique and clinical applications. Intensive Care Med 2013;39:801–10.
- Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest 1997;112(1):186–92.
- Burns SM, Fisher C, EarvenTribble SS, Lewis R, Merrel P, Conaway MR, et al. Multifactor clinicalscore and outcome of mechanical ventilation weaning trials: BurnsWean Assessment Program. Am J Crit Care 2010;19:431–9.
- Meade M, Guyatt G, Cook D, Griffith L, Sinuff T, Kergl C, et al. Predicting success in weaning from mechanical ventilation. Chest 2001;120(6):400–24.
- Conti G, Montini L, Pennisi MA, Cavaliere F, Arcangeli A, Bocci MG, et al. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med 2004;30(5):830–6.
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324(21):1445–50.
- Vallverdu I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clinical characteristics, respiratory functional parameters, and outcome of a two hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med 1998;158(6):1855–62.
- Yan S, Lichros I, Zakynthinos S, Macklem PT. Effect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathing. J Appl Physiol 1993;75(3):1364–70.
- Epstein SK. Etiology of extubation failure and the predictive valueof the rapid shallow breathing index. Am J Respir Crit Care Med 1995;152:545–9.
- Krieger BP, Isber J, Breitenbucher A, Throop G, Ershowsky P. Serial measurements ofthe rapid-shallow-breathing index as a predictor of weaning outcomein elderly medical patients. Chest 1997;112:1029–34.
- Johannigman JA, Davis Jr K, Campbell RS, Branson RD, Luchette FA, Hurst JM. Use of the rapid/shallow breathing index as an Indicator of patient work of breathing during pressure support ventilation. Surgery 1997;122:737–41.
- Barrera R, Melendez J, Ahdoot M, Huang Y, Leung D, Groeger JS. Flow triggering added to pressure support ventilation improves comfort and reduceswork of breathing in mechanically ventilated patients. J Crit Care 1999;14:172–6.
- dos Reis HF, Almeida ML, da Silva MF, Moreira JO, Rocha MD, et al. Association between the rapid shallow breathing index and extubation success in patients with traumatic brain injury. Rev Bras TerIntensiva 2013;25(3):212–7.
- Karthika M, Al Enezi FA, Pillai LV, Arabi YM. Rapid shallow breathing index. Ann Thorac Med 2016;11(3):167–76.
- Boutou AK, Abatzidou F, Tryfon S, Nakou C, Pitsiou G, Argyropoulou P, et al. Diagnostic accuracy of the rapid shallow breathing index to predict a successful spontaneous breathing trial outcome in mechanically ventilated patients with chronic obstructive pulmonary disease. Heart Lung 2011;40(2):105–10.
- Chatila W, Jacob B, Guaglionone D, Manthous CA. The unassisted respiratoryratetidal volume ratio accurately predicts weaning outcome. Am J Med 1996;101(1):61–7.
- Kuo PH, Wu HD, Lu BY, Chen MT, Kuo SH, Yang PC. Predictive value of rapid shallowbreathing index measured at initiation and termination of a 2-hourspontaneous breathing trial for weaning outcome in ICU patients. J Formos Med Assoc 2006;105(5):390–8.
- Segal LN, Oei E, Oppenheimer BW, Goldring RM, Bustami RT, Ruggiero S, et al. Evolution of pattern ofbreathing during a spontaneous breathing trial predicts successfulextubation. Intensive Care Med 2010;36(3):487–95.
- Zhou P, Zhang Z, Hong Y, Cai H, Zhao H, Lin S, et al. The predictivevalue of serial changes indiaphragm function during the spontaneous breathingtrial for weaning outcome: astudy protocol. BMJ Open 2017;7.
- Li C, Li X, Han H, Cui H, Wang G, Wang Z. Diaphragmatic ultrasonography for predictingventilator weaning A meta-analysis. Medicine 2018;97(22):e10968.
- Abbas A, Embarak S, Walaa M, Lutfy SM. Role of diaphragmatic rapid shallow breathing index in predicting weaning outcome in patients with acute exacerbation of COPD. Int J COPD 2018;13:1655–61.