Abstract
Herbal medicines are widely accepted as a primary source of healthcare due to their natural origin. However, this widespread popularity is counterbalanced with the lack of relevant research. The need to account for this deficiency motivated the present study which aims at (1) assessing physicians’ knowledge and attitude toward herbal medicines, (2) determining to what extent herbal medicines are utilized by physicians in the Kingdom of Bahrain, and (3) highlighting the main factors that may facilitate or hinder the utilization of herbal medicines. A cross-sectional study was conducted to cover 96 physicians conveniently sampled from different departments among one public and two private hospitals. The main tool that was used to gather the required data was a self-administered questionnaire that has been specifically developed by the researchers to address the study objectives. The collected data were processed by the statistical package for social sciences SPSS (version 18). The study found that 64.6% of the participated physicians have generally basic knowledge on herbal medicines, and half of them acquired their knowledge from experience. Moreover, the results showed a tendency by physicians to use herbal medicines personally more frequently than prescribing them to the patients. Interestingly, the majority (91.7%) of the participants showed a desire to enhance their knowledge with regard to herbal medicines. They ascertained that the rational use of herbal medicines is hindered by poor quality control (65.6%) and limited information on their adverse events (62.5%). The physicians claimed that the availability of sufficient knowledge (68.8%) beside the low cost (66.7%) are major facilitating factors toward utilizing herbal medicines.
1 Introduction
Complementary and alternative medicine (CAM) is widely used worldwide. According to WHO guidelines (Citation2004) and NIH (Citation2010) then CAM is defined as a group of diverse medical and healthcare systems, practices, and products that are not currently considered to be part of conventional medicine. This popularity of CAM is basically derived from the wishes for non-pharmacological treatment. One important example of CAM is herbal medicines which constitute the focus of this study, and defined as medicines originate from plant-based ingredients which are produced by extraction, fractionation, purification, concentration, steeping, heating or any other physical or biological processes with no chemically defined substances. Herbal medicines have been used since the beginning of human history. There are four basic systems known for herbal medicines: Traditional Chinese, Traditional Indian (Ayurvedic), Western, and Traditional Arab. Then it comes as no surprise that herbal medicines play an increasingly important role in healthcare and their use at the hope of tackling diseases is widespread (CitationAd’hiah et al., 2013; CitationAmin and Mousa, 2007; CitationGratus et al., 2009). Indeed, several studies found that herbal medicines are the most commonly used CAM among pharmacy/medical students (Awad et al., Citation2012; Freymann et al., Citation2006; James and Bah, Citation2014).
WHO guidelines (Citation2004) on safety monitoring of herbal medicines in pharmacovigilance systems stated that there is a widespread misconception that natural remedies are harmless and carry no risk. This common belief was confirmed by several studies (Ernst, Citation1998; Saad et al., Citation2005) which ascertained that one main reason behind the interest in herbal medicines is the notion that all herbal products due to their natural origin are safe and effective. As a consequence of this belief, side effects (unintended effect of a drug related to its pharmacological properties) of herbal medicines and adverse events (unwanted medical occurrence that may present during treatment with a drug) that may arise from their consumption are often overlooked (Bent, Citation2008; De Smet, Citation2002). There is also the possibility of interaction between herbal medicines and the conventional medicines which might cause serious health problems (Neustadt, Citation2006). On the other hand, patients have very limited reliable resources concerning the use of herbal medicines and the most common sources of advice on herbal medicines are friends and relatives (Gratus et al., Citation2009; Suleiman, Citation2014).
As far as the herbal medicines are concerned, then physicians are not in a better situation than patients since physicians themselves lack the relevant knowledge and hence they are unable to give informed advice to their patients (Ameade et al., Citation2015; Xu and Levine, Citation2008). Indeed, Suleiman (Citation2014) and Vickers et al. (Citation2006) found that the majority of patients are not disclosing the use of herbal medicines to their physicians. This lack of communication between patients and physicians is a serious problem that supports the need for healthcare professionals to be aware of herbal medicines use alongside conventional medicines. The same assertion was confirmed by several studies (Awodele et al., Citation2012; Clement et al., Citation2005; Ghia and Jha, Citation2012) which reported that the gap between acceptance of herbal medicines and the poor knowledge that healthcare professionals have about these remedies reflects the need for educational intervention.
The aforementioned problems raise the need for further research to provide adequate information concerning the use of herbal medicines toward integrating them into the healthcare system. Despite the fact that the Arabian Gulf region has a long tradition of herbal therapies (Amin and Mousa, Citation2007), the number of relevant studies is very limited. The interest here lies in the Kingdom of Bahrain, which is known to be a pioneer among the Arabian Gulf countries regarding healthcare. According to WHO report (Citation2005), Bahrain regulates herbal medicines using the same, or partly the same, legal framework as is used for conventional pharmaceuticals. Moreover, herbal medicines are sold in pharmacies as over-the-counter medicines and in special outlets in the Kingdom of Bahrain. A few studies have been conducted in Bahrain concerning CAM in general (Khalaf and Whitford, Citation2010) and herbal medicines in specific (Al-Khuzai et al., Citation2010). However, the intention of these studies was not the physicians. To the best of our knowledge, there is no previous study conducted in the Kingdom of Bahrain to assess physicians’ knowledge and attitude toward herbal medicines as well as the extent of their utilization.
2 Methods
A cross-sectional study was conducted to assess physicians’ knowledge and attitude toward herbal medicines. The study determined to what extent herbal medicines are utilized by physicians in the Kingdom of Bahrain with respect to the category of utilization (prescription or personal-use) and purpose of utilization (complementary or alternative). It also highlighted the main facilitating factors that might encourage physicians to utilize herbal medicines, and the main hindering factors that might preclude the rational use of herbal medicines from physicians’ perspective.
According to the Central Informatics Organization, Bahrain has 27 health centers, 3 public hospitals and 16 private hospitals in 2013. All physicians working in the healthcare system of the Kingdom of Bahrain represented by the health centers and general hospitals (excluding specialized hospitals such as maternity and psychiatric hospitals) were eligible to participate in the study. A convenience sampling method was implemented on which the inclusion of both public and private hospitals was taken into account at the attempt to gain a general understanding about the research topic of interest. More specifically, the Salmaniya Medical Complex was included as the largest public hospital. The complex dates back to the 1950s and has around 900 beds. As for the private hospitals, the American Mission Hospital was included since it is the oldest hospital in the Kingdom of Bahrain (dates back to 1902) and it is also the longest-standing hospital in the Arabian Gulf. Moreover, the International Hospital of Bahrain was considered in the study as one of the major private hospitals. It is worth mentioning that, according to the Health Statistics 2013–2014 published by the Health Information Directorate – Ministry of Health, the selected private hospitals are among the largest private hospitals in the Kingdom of Bahrain in terms of the medical and allied health manpower. Once the hospitals have been specified, a number of physicians were conveniently selected from different departments within each of the three hospitals to participate in the study. We note that the study design detailed above was mainly adopted from Suleiman (Citation2014).
The researchers developed a self-administered questionnaire that was specifically designed to address the study objectives after reviewing the relevant literature (Ameade et al., Citation2015; Awodele et al., Citation2012"; Clement et al., Citation2005; Gaul et al., Citation2011; Hasan et al., Citation2011; James and Bah, Citation2014; Xu and Levine, Citation2008). The developed questionnaire has four sections. Section 1 concerns with the physicians’ profile including gender, qualification, position, experience, and the department in which the physician works. With regard to the physicians’ knowledge on herbal medicines, then Section 2 covers questions about knowledge level, source, and enhancement. Section 3 consists of 5-point likert scale questions that evaluate physicians’ utilization of herbal medicines in terms of prescription, personal-use, complementary-usage, and alternative-usage. The point descriptors are never, rarely, sometimes, often and always. Section 4 consists of yes–no questions that explore the facilitating and hindering factors of herbal medicines utilization. A graphical representation for the four sections of the developed questionnaire are presented in .
The developed questionnaire was initially piloted among sixteen physicians from two health centers (Jidhafs Health Center and Al-Naim Health Center). We elected to conduct the pilot study in health centers instead of hospitals for simplicity in distributing and collecting the questionnaire. The received feedback was incorporated into the revised version of the questionnaire to ensure its validity before embarking on the fieldwork. The corresponding Cronbach-alpha coefficient was 0.779 and hence the reliability of the questionnaire was established. Then a total of 150 copies of the revised version of the questionnaire were distributed among the three selected hospitals. Each copy of the questionnaire was accompanied with a cover page stating the purpose of the study and giving clear instructions to the respondents. Moreover, voluntary participation and confidentiality were assured. The questionnaires were handled personally to the administrators in the selected hospitals who signed a letter confirming their consent to take a role in the study. Afterward, the questionnaires were distributed to the physicians from the available departments and collected back (after three weeks) by the administrators in order to be returned to the researchers.
The collected data were processed by the statistical package for social sciences SPSS (version 18). More concretely, the data have been analyzed using both descriptive and inferential statistics (non-parametric tests: chi-square test for association, Kruskal–Wallis test and Mann–Whitney test for differences).
3 Results
3.1 Physicians’ profile
Out of the 150 distributed copies of the questionnaire, 100 were returned back to represent a response rate of 66.7%. However, four of the returned copies were invalid due to a noticeable number of non-answered questions to left with a net total of 96 participants that constituted the study sample as shown in .
Table 1 The study sample.
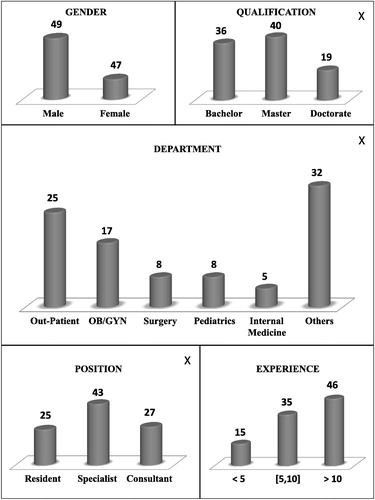
Some demographic information of the participated physicians is summarized in . Nearly 51% of the participated physicians were males. With regard to the five major departments, the majority of the participants were from the out-patient and OB/GYN with 26.0% and 17.7% respectively. Only 5.2% of the participants were from the internal medicine department, while 8.3% of the participants were from each of the surgery and pediatrics departments. The rest of the participants (33.3%) distributed among other departments (not specified). About 37.5% of the participants have a bachelor degree and 41.7% of them have a master degree, while those holding a PhD degree constitute 19.8% of the study sample. There were only 15.6% of the participants having less than five years of experience in the medical field, while about 36.5% of the participants experiencing five-to-ten years and about 47.9% whose experience exceeds ten years. The majority of the participants were specialists (44.8%) and the rest of them were either residents (26.0%) or consultants (28.1%).
Fig. 2 The profile of the participated physicians (X means missing data due to non-answered questions). As per the position of the participants: the resident is a physician who spends a number of training years in a certain medical department after graduation; the specialist is a board certified physician who has successfully completed the residency period in the intended medical specialty and passed a comprehensive test given by a recognized medical organization; the consultant is a physician who has an additional training in his/her medical specialty and hold a fellowship from a recognized medical agency.
3.2 Knowledge on herbal medicines
summarizes physicians’ responses regarding knowledge on herbal medicines. It reveals that the level of knowledge on herbal medicines is considered to be basic for the majority (64.6%) of the participated physicians. In contrast, there were only two out of 96 participants (2.1%) having an advanced level of knowledge on herbal medicines. The experience was found to be the main source of knowledge on herbal medicines among three options provided in the questionnaire by half of the participants, followed by the academic study (28.1%) and other resources such as the internet (21.9%). Interestingly, 91.7% of the participated physicians showed a desire to enhance their knowledge regarding herbal medicines compared to only 8.3% who did not want to do so. Furthermore, reports a significant association (using chi-square test) between physicians’ position and the source of knowledge on herbal medicines. It was found that 61.7% of the physicians in the study who acquired their knowledge from experience were specialists, while 55.6% of those having academic-based knowledge were consultants.
Table 2 Summary of physicians’ responses regarding knowledge on herbal medicines.
Table 3 Results of chi-square test for association.
3.3 Utilization of herbal medicines
The results obtained regarding the utilization of herbal medicines by the physicians in the study are presented in . The overall conclusion that emerged from the corresponding results is that physicians’ utilization of herbal medicines was found to be limited. More specifically, about 18.8–33.3% of the participated physicians never used herbal medicines and that a small percentage (does not exceed 11.5%) of the participants “often” or “always” use herbal medicines, while the majority of the participants ranked their utilization of herbal medicines as either “rarely” or “sometimes”. Furthermore, the presented results seem to indicate that the participated physicians tend to use herbal medicines personally more than prescribing them to their patients. Interestingly, the results regarding the complementary-usage and the alternative-usage of herbal medicines are comparable in the sense that almost the same percentage of the participants ranked their utilization of herbal medicines to complement or to replace conventional medicines as “never”, “rarely” or “sometimes”.
Table 4 Summary of physicians’ responses regarding utilization of herbal medicines.
3.4 Facilitating and hindering factors
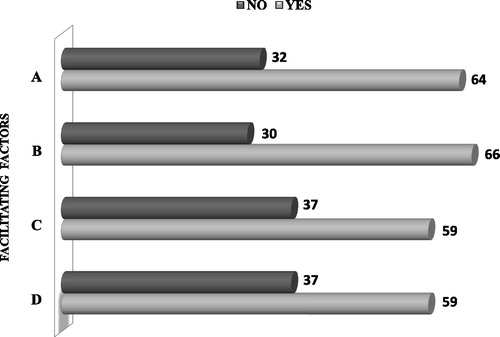
As far as the facilitating factors are concerned, shows that the majority of the participants considered sufficient knowledge on herbal medicines (68.8%) as well as the low cost of herbal medicines (66.7%) as major factors that encourage physicians toward utilizing these remedies. Moreover, deficits and unfulfilled goals of conventional medicines as well as side effects and adverse events of conventional medicines were considered to be as facilitating factors by 61.5% of the participated physicians.
Fig. 3 The facilitating factors from the perspective of the participated physicians. These factors are represented by the letters on the vertical axis as follows. A: Low cost of herbal medicines, B: Sufficient knowledge on herbal medicines, C: Deficits and unfulfilled goals of conventional medicines, D: Side effects and adverse events of conventional medicines.
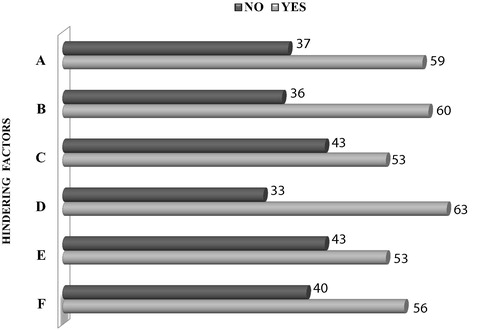
With regard to the hindering factors, shows that about two third of the participated physicians asserted that the most important factor is the poor quality control (lack of safety and efficacy monitoring) of herbal medicines. Moreover, physicians claimed that the other hindering factors are the limited information on the adverse events of herbal medicines (62.5% of the participants) and the absence of formal regulation such as standardized terms, definitions, classification of herbal medicines (61.5% of the participants). The least important hindering factors (according to 55.2% of the participants) were found to be the lack of effective communication with health authorities regarding herbal medicines and the fear of formal liability with regard to utilizing herbal medicines.
Fig. 4 The hindering factors from the perspective of the participated physicians. These factors are represented by the letters on the vertical axis as follows. A: Absence of formal regulation on herbal medicines, B: Limited information on adverse events of herbal medicines, C: Not effective communication with health authorities regarding herbal medicines, D: Poor quality control of herbal medicines, E: Fear of professional liability with regard to utilizing herbal medicines, F: Lack of availability of herbal medicines.
3.5 Testing for differences among participants
The interest here lies in testing for statistically significant differences among the participated physicians with respect to their utilization of herbal medicines (prescription, personal-use, complementary, alternative). The overall comparisons were performed using the Kruskal–Wallis test and the corresponding results are summarized in . The bivariate comparisons were performed using the Mann–Whitney test and the corresponding results are summarized in .
Table 5 Results of the overall comparisons using Kruskal–Wallis test (p-value).
Table 6 Selected results of the bivariate comparisons using Mann–Whitney test.
The personal-use of herbal medicines was found to be significantly more by female-physicians than male-physicians. In contrast, no significant differences were found among physicians from the five major departments (those fall under the title “Others” were excluded from the analysis). The same conclusion can be drawn when looking at the qualification or the experience in the medical field. Similarly, utilizing herbal medicines did not significantly differ between physicians with basic knowledge and those having moderate knowledge. We note that the only two physicians enjoying an advanced level of knowledge on herbal medicines were excluded from these comparisons. On the other hand, when prescription for herbal medicines was concerned, then specialists generally used herbal medicines more than other physicians in the study sample and this realization was found to be statistically significant. Furthermore, it seems to be that physicians with knowledge on herbal medicines sourced from experience prescribed herbal medicines to their patients significantly more than those who acquired their knowledge from other sources (apart from academic-source). Interestingly, when comparing specialists with consultants with respect to the complementary-usage of herbal medicines then the former physicians used these remedies significantly more than the latter physicians.
4 Discussion
The results revealed that the physicians who took place in the study have basic knowledge on herbal medicines. In light of this realization, it might be argued that patients will not be provided with the necessary advice and guidance regarding herbal medicines. Nevertheless, the participated physicians showed positive attitude toward herbal medicines that was demonstrated by the overwhelming tendency to enhance their knowledge. This seems to represent a strong desire by physicians to be better equipped to serve their patients. Our findings are consistent with those reported by other studies such as Awodele et al. (Citation2012) for resident doctors in Nigeria, Clement et al. (Citation2005) for physicians in Trinidad, and Ghia and Jha (Citation2012) for healthcare professionals in India. Moreover, physicians’ desire to enhance their knowledge on herbal medicines supports the need for incorporating herbal medicines into the undergraduate curricula of medicine. A similar conclusion was drawn by Ghia and Jha (Citation2012) for herbal medicines, and by Hasan et al. (Citation2011) as well as James and Bah (Citation2014) for CAM.
It was expected that physicians’ poor knowledge on herbal medicines would have an impact on their utilization of these remedies. Indeed, the utilization of herbal medicines by the participated physicians was found to be limited, and that experience was the main source consulted regarding herbal medicines. This comes as no surprise since practical experience itself proves to be a useful source of knowledge given that the majority of the participants had no formal training on herbal medicines during their academic study. Furthermore, when comparing the personal-use with the prescription of herbal medicines then a tendency to the former category of utilization was realized. A possible explanation for this tendency might be the poor knowledge that the physicians have on herbal medicines which makes experience, in spite of its importance, not an authorized source of information on which physicians can refer to in order to be confident when prescribing such remedies to their patients. Interestingly, a significant difference was found between genders when personal-use of herbal medicines was considered with female physicians recording higher percentage of utilization than male counterparts. This comes in line with the results of the study conducted by Risberg et al. (Citation1999).
It was found that physicians’ position and knowledge on herbal medicines are significantly associated. Specifically, specialists constituted the majority of the participants who have experience-based knowledge on herbal medicines, while consultants constituted the majority of the participants who have academic-based knowledge on herbal medicines. Furthermore, the study reported comparable results with regard to utilizing herbal medicines as complementary or alternative to the conventional medicines. This skeptical perception by physicians is possibly due to the limited information available on herbal medicines. It is likely that physicians who used herbal medicines along with the conventional ones had doubt on their effectiveness. It is worth mentioning that Awodele et al. (Citation2012) found that none of the 300 doctors in their study thought that herbal medicines alone could completely treat a patient. It is also interesting to note that PhD-holders and those having more than 10 years experience in the medical field believed that herbal medicines should not be used to replace the conventional ones unless the efficacy of the former medicines has been proved by well-known accredited scientific research centers such as FDA in USA. This note was taken from the comments provided by the participated physicians (not reported). On the other hand, physicians who used herbal medicines instead of the conventional ones probably tried to avoid unexpected consequences caused by possible risk of interaction between the two types of medicines. This risk was addressed in detail by Neustadt (Citation2006). In general, our findings regarding the complementary or alternative usage of herbal medicines emphasize the need for constructing a reliable database about herbal medicines, a point that was also highlighted by Suleiman (Citation2014).
In agreement with Xu and Levine (Citation2008), the participants believed that being equipped with the necessary knowledge is the main factor that would encourage physicians to use herbal medicines rationally. On the other hand, poor quality control of herbal medicines with respect to their safety and efficacy was considered by the majority of the participants as the main hindering factor. Therefore, the National Health Regulatory Authority in the Kingdom of Bahrain has an essential role to take with this regard.
A valuable contribution of the study is enhancing awareness about herbal medicines by providing primary information on the knowledge, attitude and utilization of herbal medicines by physicians in the Kingdom of Bahrain. However, there are issues pertaining to the study design that may limit its generalization including the small sample size and the implemented sampling method. In particular, no permission was given by the administration of the selected hospitals to distribute and collect the questionnaires under the researchers’ control and hence the process has been managed by the administrative staff at those hospitals. For this reason, the convenience sampling method was found to be the most appropriate method to be implemented. Another issue that is worth mentioning is the relatively high percentage of PhD holders in the study sample which is probably reflected by the fact that the majority of the participants were working in well-known private hospitals that usually employ highly-qualified physicians. Therefore, future research should take these issues into consideration. Moreover, the present study can be improved by several considerations. One direction of improvement is considering other factors that might influence physicians’ knowledge, attitude and utilization of herbal medicines. The environment and the cultural background are two important examples of such factors. In addition, it would be interesting to investigate which diseases that herbal medicines are commonly used for.
5 Conclusion
This study revealed that the participated physicians have generally basic knowledge on herbal medicines and that the main source of this knowledge was the experience. However, almost all the participants showed a desire to enhance their knowledge about herbal medicines. It was found that the utilization of herbal medicines by the participated physicians was limited and mainly for personal-use. The low cost of herbal medicines and the availability of sufficient knowledge on these remedies were the two major facilitating factors that encourage physicians toward utilizing herbal medicines. On the other hand, poor quality control of herbal medicines, limited information on their adverse events as well as the absence of formal regulation were found to be the three major hindering factors that obstacle physicians from utilizing herbal medicines.
In light of the study findings, it is recommended to incorporate herbal medicines into the undergraduate academic study of medicine. Moreover, the decision makers in the Ministry of Health, National Health Regulatory Authority and Supreme Council of Health are recommended to construct a research unit concerns with health issues in relation with herbal medicines in an effort to promote an integrated healthcare system in the Kingdom of Bahrain.
Ethical approval
The original work on which the present study is based is the graduation project of the first author. The relevant ethical approval was obtained from the School of Medicine at the AMA International University, BAHRAIN.
Authors’ contribution
MH (physician) conceived the idea for the study, took part in the design, acquisition of data, interpretation and analysis of data. SH (statistician) was mainly involved in the preparation of the study questionnaire and the relevant statistical analysis of the collected data. Both authors involved in the writing of the manuscript; they read and approved its final version.
Conflicts of interest
The authors declare no personal or financial interests that could inappropriately influence the study.
Acknowledgements
We are grateful to the administrators and physicians who took interest in the research and we would like to thank them for the time they have devoted to participate in this study.
Notes
Peer review under responsibility of University of Bahrain.
References
- A.H.Ad’hiahO.N.H.Al-BederiK.W.Al-SammarraeCytotoxic effects of Agrimonia eupatoria L. against cancer cell lines in vitroJAAUBAS1420138792
- J.Al-KhuzaiQ.MandeelA.A.Al-LaithKnowledge, attitude, and practice of medicinal plants use by native people in BahrainArab Gulf J. Sci. Res.282010105125
- E.P.K.AmeadeA.AmalbaG.K.HelegbeB.S.MohammedHerbal medicine: a survey on the knowledge and attitude of medical students in Tamale, GhanaPeak J. Med. Plant Res.3201518
- A.AminM.MousaMerits of anti-cancer plants from the Arabian Gulf regionCancer Therapy520075566
- A.I.AwadS.Al-AjmiM.A.WaheediKnowledge, perceptions and attitudes toward complementary and alternative therapies among Kuwaiti medical and pharmacy studentsMed. Principles Pract.212012350354
- O.AwodeleE.O.AgbajeO.O.AbiolaD.F.AwodeleD.C.DolapoDoctor’s attitudes towards the use of herbal medicine in Lagos, NigeriaJ. Herbal Med.220121622
- S.BentHerbal medicine in the United States: review of efficacy, safety and regulationInt. J. Gen. Med.232008854859
- Y.N.ClementA.F.WilliamsK.KhanT.BernardS.BholaM.FortuneO.MedupeK.NageeC.E.SeaforthA gap between acceptance and knowledge of herbal remedies by physicians: the need for educational interventionBMC Complement. Altern. Med.52005520
- P.A.De SmetHerbal remediesN. Engl. J. Med.347200220462056
- E.ErnstHarmless herbs? A review of the recent literatureAm. J. Med.1041998170178
- H.FreymannT.RennieI.BatesS.NebelM.HeinrichKnowledge and use of complementary and alternative medicine among British undergraduate pharmacy studentsPharm. World Sci.2820061318
- C.GaulT.SchmidtR.EismannS.ZierzAttitudes towards complementary and alternative medicine in chronic pain syndromes: a questionnaire-based comparison between primary headache and lower back painBMC Complement. Altern. Med.112011
- C.J.GhiaR.K.JhaInfluence of knowledge on attitude and practice of health care professionals regarding use of herbal medicines in a tertiary care teaching hospital: a cross-sectional surveyInt. J. Res. Pharmaceut. Biomed. Sci3201212151219
- C.GratusS.WilsonS.M.GreenfieldS.L.DameryS.A.WarmingtonR.GrieveN.M.StevenP.RoutledgeThe use of herbal medicines by people with cancer: a qualitative studyBMC Complement. Altern. Med.92009
- S.S.HasanC.S.YongM.G.BaberA.HameedM.R.BaigS.M.IqbalT.KairuzUnderstanding, perceptions and self-use of complementary and alternative medicine (CAM) among Malaysian pharmacy studentsBMC Complement. Altern. Med.112011
- P.B.JamesA.J.BahAwareness use attitude and perceived need for complementary and alternative medicine (CAM) education among undergraduate pharmacy students in Sierra Leone: a descriptive cross-sectional surveyBMC Complement Altern Med142014
- A.J.KhalafD.L.WhitfordThe use of complementary and alternative medicine by patients with diabetes mellitus in Bahrain: a cross-sectional studyBMC Complement. Altern. Med.102010
- National Institutes of Health (NIH), National Center for Complementary and Alternative Medicine (NCCAM), 2010. What is complementary and alternative medicine (CAM)? [Online; accessed April 2014]. URL: http://nccam.nih.gov/health/whatiscam/
- J.NeustadtHerb-drug interactions: what clinicians need to know?J. Integr. Med.520061626
- T.RisbergA.KolstadA.JohansenK.VingerhagenOpinions on and use of alternative medicine among physicians, nurses and clerks in northern NorwayIn Vivo131999493498
- B.SaadH.AzaizehO.SaidTradition and perspectives of Arab herbal medicine: a reviewCAM Complement. Altern. Med.22005475479
- A.K.SuleimanAttitudes and beliefs of consumers of herbal medicines in Riyadh, Saudi ArabiaJ. Community Med. Health Edu.42014
- K.A.VickersK.B.JollyS.M.GreenfieldHerbal medicine: women’s views, knowledge and interactions with doctors: a qualitative studyCAM Complement. Altern. Med.62006
- World Health Organization (WHO), 2004. Guidelines on safety monitoring of herbal medicines in pharmacovigilance systems. [Online; accessed April 2014]. URL: http://apps.who.int/medicinedocs/index/assoc/s7148e/s7148e.pdf
- World Health Organization (WHO), 2005. National policy on traditional medicine and regulation of herbal medicines, a global survey. [Online; accessed April 2014]. URL: http://apps.who.int/medicinedocs/en/d/Js7916e/
- S.XuM.LevineMedical residents’ and students’ attitudes towards herbal medicines: a pilot studyCan. J. Clin. Pharmacol.15200814

