Abstract
This paper raises some troubling questions about the fertility treatments provided to Canadian gestational surrogates, women not genetically related to the child that they carry. Using information published between 2003 and 2012 by Canada’s Assisted Reproduction Registry, the paper traces the growing incidence of births to gestational surrogates. The transfer of more than one embryo increases the chance of pregnancy and the incidence of multiple births, and while the incidence of multiple births has declined overall since 2010, gestational surrogates consistently experience a higher proportion of multiple births and experienced higher levels of multiple embryo transfers. In 2012, just 26% of gestational surrogates received a single embryo transfer compared to 47% of other in vitro fertilisation (IVF) patients. The paper suggests that renewed attention needs to be paid to the counselling provided to gestational surrogates and treatment consenting mechanisms used by IVF clinics and that review of the 2007 Canadian Medical Association surrogate treatment guidelines is warranted. Finally, the paper describes the difficulties in obtaining accurate data about Canadian assisted reproductive medicine. Without good data, it becomes far more difficult to identify the possibility of potentially harmful practices.
Résumé
Cet article soulève des questions troublantes sur les traitements de la fécondité pratiqués sur les mères porteuses (femmes qui ne sont pas génétiquement apparentées à l’enfant qu’elles portent) canadiennes. En utilisant les informations publiées sur une période de dix ans (2003-2012) par le Registre canadien des techniques de procréation assistée, l’article révèle l’incidence croissante des naissances chez des mères porteuses. L’implantation de plus d’un embryon augmente les chances de grossesse et l’incidence de naissances multiples et, s’il est en général moins fréquent qu’elles donnent naissance à plus d’un enfant à la fois depuis 2010, les mères porteuses enregistrent systématiquement une proportion plus élevée de naissances multiples. En 2012, à peine 26% des mères porteuses avaient reçu l’implantation d’un seul embryon,contre 47% des autres patientes de la FIV. L’article suggère qu’il faut accorder davantage d’attention aux conseils prodigués aux mères porteuses et aux mécanismes de consentement au traitement utilisés par les cliniques de FIV. Il note aussi qu’il est nécessaire de réviser les directives de l’Association médicale canadienne sur le traitement des mères porteuses. Enfin, l’article décrit les difficultés rencontrées pour obtenir des données exactes sur la procréation médicalement assistée au Canada. Sans informations solides, il est beaucoup plus difficile de déceler la possibilité de pratiques potentiellement nuisibles.
Resumen
Este artículo plantea algunas preguntas preocupantes acerca de los tratamientos de fertilidad proporcionados a madres gestantes (mujeres que no están emparentadas genéticamente con la criatura que llevan en el vientre) canadienses. Utilizando información publicada en un plazo de diez años (de 2003 a 2012) por el Registro Canadiense de Técnicas de Reproducción Asistida, el artículo rastrea la creciente incidencia de partos a madres gestantes. La transferencia de más de un embrión aumenta la probabilidad de embarazo y la incidencia de partos multiples y aunque la incidencia de dar a luz a más de un hijo a la vez ha disminuido en general desde el año 2010, las madres gestantes experimentan un mayor porcentaje de partos múltiples. En el año 2012, tan solo el 26% de las madres gestantes recibieron una transferencia de un único embrión, comparado con el 47% de otras pacientes de fertilización in vitro (FIV). El artículo sugiere que es necesario prestar atención renovada a la consejería brindada a madres gestantes y a los mecanismos utilizados por las clínicas de FIV para obtener consentimiento para el tratamiento, y que es necesario revisar las directrices de 2007 de la Asociación Médica Canadiense referentes al tratamiento de madres gestantes. Por último, el artículo describe las dificultades para obtener datos exactos sobre la medicina reproductiva asistida canadiense. Sin datos buenos, es mucho más difícil identificar la posibilidad de prácticas posiblemente dañinas.
Introduction
The practice of a woman conceiving and carrying a child for an individual or couple, who for medical or social reasons are unable to have their own children, has been characterized as morally troubling as it breaks the assumed closed link between genetics, gestation, and motherhood.Citation1,2 The discourse and practice of surrogacy raises tensions about contracts, altruism, autonomy, and independence and about its potential to commercialise human reproduction and commoditise the body.Citation3–5
In Canada, both ‘traditional’ surrogacy, where the surrogate is genetically related to the child she bears for the intended parent(s), and ‘gestational’ surrogacy, where the surrogate has no genetic link to the offspring, are lawful provided that the surrogate arrangement is altruistic, though expenses incurred by the surrogate can be reimbursed.Citation6 For an increasing number of childless Canadian couples and individuals including gay men, surrogacy may be the only way to have biological children. A 2012 survey reveals that surrogacy is neither a taboo topic nor an unrealistic reproductive option for many Canadians; one-quarter of childless adult women and 40% of childless adult men would consider using a surrogate should they or their partner not be able to carry and give birth to their biological child.Citation7 Personal testimonials featured in popular magazines,Citation8–10 newspaper articles reporting on out-of-province and out-of-country surrogate births,Citation11–13 and exposés of media celebrities including Joël Legendre and his husband, who forced the Quebec government to pay their surrogacy costs,Citation14 lead one to conclude that surrogacy as practiced in Canada is an acknowledged, albeit controversial, twenty-first century family-making activity.
Despite Canadians’ increased acceptance of surrogacy, comparatively little is known about the practice. Lack of data,Citation15 social stigma associated with infertility,Citation16 perception of legal uncertainty about surrogacy,Citation15–17 and reproductive tourismCitation18,19 have been cited as factors contributing to a shortage of reliable and comprehensive information about Canada’s surrogacy practices.
This paper seeks to fill this knowledge gap, and in so doing, it raises several troubling questions about the fertility treatments gestational surrogates receive. While there are limitations with the data source – the Canadian Assisted Reproduction Technology Registry (CARTR) and Better Outcomes Registry and Network (BORN) – used to analyse gestational surrogacy trends and outcomes, the paper demonstrates that assisted reproduction technology (ART) registry information yields important insights.
Canada’s Assisted Reproduction Technology Registry: CARTR-BORN
The science of embryology, the practice of reproductive medicine, and the regulation of fertility treatment data collection systems play pivotal roles in the structure of ART registries and the management of fertility treatment knowledge.Citation20 These factors shape the medicalised narrative structuring what “we know and do not know”Citation21 about fertility treatment in general and surrogacy in particular.
Unlike their AmericanCitation22 and BritishCitation23 counterparts, Canadian fertility clinics are not required by law to report AR treatment information to a recognised public health authority. When Canada’s Assisted Human Reproduction (AHR) Act 2004 was passed, CARTR, as it was then known, could have been replaced or possibly merged into the federally legislated Personal Health Information Registry, but it was not. The 2010 Reference re AHR Act decisionCitation24 ended the federal government’s ability to establish ART and donor registries when the Supreme Court of Canada ruled ultra vires the sections of the Act regulating areas deemed to be under provincial constitutional authority, namely the practice of medicine and research. In 2010 Quebec regulated the practice of fertility medicineCitation25 and by early 2016, Ontario was funding one stimulated cycle of IVF.Citation26 To date, no provincial government has created fertility treatment or donor registries, though the Canadian Fertility and Andrology Society (CFAS) recently recommended the creation of a national donor registry.Citation27
CARTR-BORN, a voluntary ART registry established and governed by Canada’s IVF clinic directors since 1999, functions as the country’s principle source of information on IVF medical practices. Regarding surrogacy, the registry contains data on the IVF treatments provided to gestational surrogates defined as:
“A woman who carries a pregnancy with an agreement that she will give the offspring to the intended parent(s). Gametes can originate from the intended parent(s) and/or a third party (parties).” Citation28
In instances of conception occurring as a result of donor insemination, a practice more typical of traditional surrogacy, the registry does not record this type of information. While IVF could be performed on traditional surrogates, Canadian fertility clinics like their American counterparts offer IVF services to gestational surrogates,Citation30 thus, Canadian and American ART registries shed no light on traditional surrogacy practices. In contrast the UK Human Fertilisation and Embryology Authority (HFEA) records fertility treatments provided to both traditional (genetic) and gestational surrogates but does not routinely publish this information.Citation31
CARTR-BORN presents a national picture of IVF treatments provided to gestational surrogates, however, its focus and structure contribute to data limitations. It holds no socio-economic information or information on fertility treatments undertaken outside Canada, and little demographic data on patients. Yet, it could tell us about the use of Canadian IVF clinics by non-residents as the address of patients and intended parents is collected, though not all clinics consistently submit this information to CARTR-BORN.Citation32
The organisation of fertility treatment information by IVF cycleFootnote* reflects embryological and ART medical practices, telling us more about gametes, embryos, and fertility procedures than about the patients receiving treatment.Citation20,36 However, by analysing this information over time, the emerging picture of gestational surrogacy practices reveals important differences in fertility treatments provided to surrogate compared to non-surrogate mothers.
Methods
Between 2001 and 2007, Canada’s ART treatment statistics were published in the journal Fertility and Sterility. From 2008 to 2012, annual data reports were made available to CFAS members and disseminated via the organisation’s website.Citation37 Beginning in 2013, only media overviews have been released. Customised tabulations are made available to approved researchers by BORN, the organization now hosting the registry on behalf of IVF clinic directors.Citation28
In response to a need for information on Canadian surrogacy practices,Citation16–18,37 the paper calculates the incidence of IVF births to gestational surrogates for the period 2001-2012 (Table 1). It then focuses on the period 2003-2012, during which most clinics reported in every year and during which important fertility treatment and policy changes took place, including federal legislation, publication of surrogate treatment and embryo transfer guidelines, greater availability of donor gametes (ova and sperm), regulation of fertility medicine by Quebec, and increased reliance on gestational surrogacy by childless couples and individuals including gay men.Citation38–40 Data for 2012 was the most recent that could be made available by BORN. For reasons of confidentiality, only Canada-level information could be obtained.
Table 1 Births in Canada, 2001-2012
Sources: CARTR-BORN. Statistics Canada, CANSIM Tables 102-4509. Live births, by birth weight and sex, Canada, provinces and territories.
Table 1 Births in Canada, 2001-2012
Sources: CARTR-BORN. Statistics Canada, CANSIM Tables 102-4509. Live births, by birth weight and sex, Canada, provinces and territories.
Descriptive statistics showing the number of gestational surrogate treatment cycles, pregnancies, births, and incidence of multiple births were compiled using ART treatment data published in the CARTR-BORN annual reports 2001-2012 and from data requests. Quebec-level data were obtained from the 2014 Quebec Commission Report.Citation41 Author-designed custom tabulations were used to verify previously released information about gestational surrogates and to calculate statistics for the non-gestational surrogate population. Data showing the incidence of one, two, and three plus embryos transferred per gestational surrogate and other IVF patient (non-gestational surrogate) treatment cycle were also obtained.Citation42 Comparative custom tabulations were made available by the Centers for Disease Control and Prevention (CDC) from the National ART Surveillance System.Citation43
Parametric statistics were used to calculate the risk ratios (RR) of gestational surrogates receiving a transfer of one embryo compared to two, and three or more embryos.Citation44 All tests were two-sided and p-values of less than 0.05 were considered statistically significant. Donor and intended mother’s own ova and fresh and frozen embryos were considered in the analysis.
Results
Increase in gestational surrogacy
Between 2001 and 2012, 52,488 live births were reported to CARTR-BORN. In 2012, IVF conceived infants comprised 1.8% of all Canadian birthsCitation45 and over 2.0% of all births occurring in Quebec.Citation41 This compares to 1.5% of American birthsCitation34 and 2.2% of all babies born in the UK in that year.Citation46
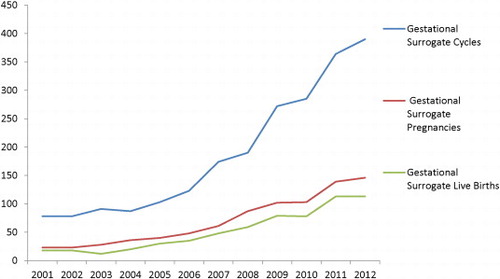
A total of 803 IVF conceived infants were born to gestational surrogates between 2001 and 2012. The 133 babies born to gestational surrogates in 2012 represented 1.9% of all IVF conceived babies born in Canada (1.8% of all IVF cycles). In the US, the CDC estimates gestational surrogates comprised about 2.5 percent all IVF cycles the same yearCitation33 (Table 1).
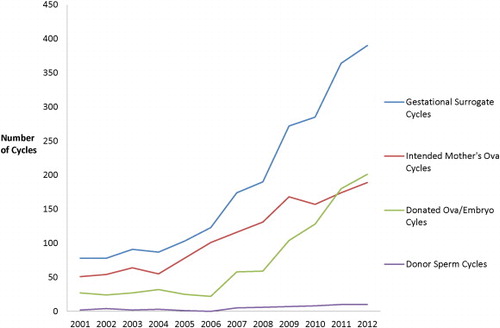
Canadian gestational surrogates were younger than intended mothers (IM); the median age of gestational surrogates was 31.8 years compared with 38.2 years for IM.Citation40 CDC data show a similar age difference: median age of 31.7 years for gestational surrogates compared to 36.5 years for IM.Citation43 Between 2003 and 2009, embryos containing ova obtained from donors other than the intended mother were used in about one-third of gestational surrogate cycles. However, by 2012, 52% of gestational cycles involved embryos containing non-IM ova. In contrast donor ova were used only in 5.5% of other IVF patient cycles that year ().
Gestational surrogates more likely to experience multiple birth
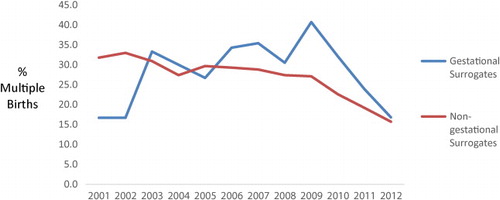
It has long been known that fertility patients experience a higher number of multiple births compared to women who do not conceive using fertility drugs or IVF.Citation47,48 What perhaps has been less understood is that gestational surrogates experience higher levels of multiple births than other IVF patients.Citation33,36,49 As illustrates, the rate of multiple births to Canadian non-surrogate mothers remained at around 27-31% between 2003 and 2009. Beginning in 2010, Quebec regulated the practice of ART medicine, and fertility clinics located elsewhere in Canada began to adopt measures to limit number of embryos transferred.Citation25,41,50 By 2012, the proportion of multiple births experienced by non-gestational surrogate patients dropped dramatically to just under 16% ().
Over the same period, the proportion of multiple births experienced by gestational surrogates remained consistently higher such that by 2009 about 41% of all gestational surrogates gave birth to more than baby at a time. In 2010, multiple births for gestational surrogates began to drop and by 2012, it had declined to 17%, about the same level as the non-gestational surrogate women. However, the gap between the number of surrogacy pregnancies and number of births appears to have widened since 2009. Pregnancy loss increased from 6.6% of surrogate pregnancies in 2009 to 19.2% by 2012.Citation37 Another possible explanation could be inconsistent birth outcome follow up, a known data limitation associated with ART registries.Citation41,48
Transfer of multiple embryos
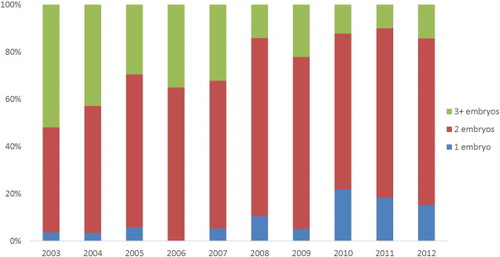
Factors contributing to multiple births include the number of embryos transferred per cycle, ova donor age, use of fresh or frozen human tissues and embryos, and age of patient.Citation33,48 Between 2003 and 2012, Canadian gestational surrogates experienced significantly higher risk of receiving a multiple embryo transfer than did other IVF patients (risk ratio [RR]: 1.08, 95% confidence interval [CI] 1.06-1.10). This occurred even though surrogates were younger and had fewer known fertility problems.Citation40 They were also more likely to receive embryos containing donor ova (non-IM ova) compared to other IVF patients (Table 2).
Table 2 Population characteristics and ART treatment factors of gestational surrogate and non-gestational surrogate cycles, CARTR-BORN, Canada, 2003-2012.
Notes:
| 1. | Residence of patients/intended parents in-and-outside of Canada. Collected by CARTR-BORN for Ontario IVF clinics only. | ||||
| 2. | Gestational surrogate transfers of donor ova (non-IM ova) comprised 13.5% of all donor ova transfers between 2007-2012. During this period, 83-91% of all donor ova was donated by women aged less than 35 years; in 2012, 89% of donor ova used in IVF/ICSI (intracytoplasmic sperm injection) was donated by women aged less than 35 years (617 cycles) and 91% of donor ova used in frozen embryo transfers was donated by women aged less than 35 years (637 cycles). Information on age of ova donor was not consistently reported to CARTR-BORN prior to 2007. | ||||
| 3. | Age of gestational surrogate is not collected by CARTR-BORN. Limited demographic information is collected for the intended parent(s) only. Like the US ART registry NASS, Canada’s CARTR-BORN considers the IVF patient to be the intended parent and not the gestational surrogate as it is the intended parent(s) who experiences infertility problems and who seeks the fertility treatment. Information about transfers to gestational surrogates is collected, however. See Perkins, Boulet, Jamieson et al (2016) and Dar, Lazer, Basilie et al. (2015). | ||||
Source: CARTR-BORN (Canadian Assisted Reproductive Technologies Registry and Better Outcomes Registry & Network Ontario). Ottawa ON, November 2015.
It should be noted that by 2012, while the proportion of multiple births in Canada had declined for both surrogates and non-surrogates, 60% of gestational surrogates received a transfer of two embryos compared to just over 40% of other IVF patients. Moreover, when surrogates received an embryo containing ova from a donor other than the IM, a situation which now comprises the majority of all gestational surrogate transfers, 85% of surrogates received two or more embryos per transfer cycle (). This result raises a troubling question about differing medical treatments being provided to gestational surrogates compared to other IVF patients. It also suggests that embryo transfer guidelines might not have been consistently followed when the patient was a gestational surrogate.
Discussion
During the last five years of the study period, the number of children born to Canadian gestational surrogates increased by 91.5%. For a growing number of childless Canadians, gestational surrogacy has become a more common reproductive option. This finding suggests that the fraud conviction of fertility consultant Leia Picard and continued federal failure to regulate the reimbursement of expenses incurred by surrogates have not served to deter childless couples and individuals from seeking to create families through surrogacy.Citation51,52
While Canada’s AR registry tells us about gestational surrogacy, little is known about other surrogacy practices. This study lacks the insights that would be gained by having information on surrogate and intended parent characteristics, and foreign and traditional surrogacy practices, nonetheless its findings lend weight to the demands made by legal experts,Citation15–18,29,38,54 ethicistsCitation19,52 and intended parentsCitation11–13 for a re-examination of the legal status of surrogacy arrangements, revision to provincial parentage laws, and review of federal AHR Act surrogacy provisions.
Implications of changes to fertility treatments provided to gestational surrogates
Over the period 2001 to 2012, IVF fertility treatment delivered to gestational surrogates became increasingly dependent on ova obtained from donors other than the intended mother. In the US, over 70% of gestational surrogacy cycles in 2012 involved the transfer of embryos comprised of third party ova (other than the intended mother).Citation43 In Canada, this phenomenon will likely increase given greater availability of donated gametes, reliance on gestational surrogacy by gay men, and the advanced age of intended mothers. The use of donor ova in gestational surrogacy raises two troublesome questions. The first concerns Canada’s gamete screening and testing regimes and the second pertains to the application of embryo transfer guidelines.
In 1996, Canada regulated the screening and testing of human sperm used in ART treatments.Citation55 It has been suggested that inconsistency exists in the manner in which donor sperm is screened and tested when used by traditional and gestational surrogates.Citation27 Regarding ova, to date no screening or screening regulations have been approved and no regulatory timetable has been provided by Health Canada, the federal department responsible for implementation of the federal AHR Act. In December 2012, Canada’s IVF clinics voluntarily adopted the Canadian Standards Association (CSA) standard Z900.2.1-12 Tissues for assisted reproduction. By mid-2015, the Standard was scheduled for review and revision. In 2016, the CFAS released Third Party Reproduction guidelines which outlined sperm and ova screening and testing procedures for surrogate patients.Citation27 No doubt, professional adherence to national standards and clinical practice guidelines offer a measure of comfort to IVF clinic staff and patients. However, neither the CSA standard nor the CFAS clinical guidelines have the force of federal law as envisaged by Parliament when amendments to the Assisted Human Reproduction Act were passed in 2012.
Multiple embryo transfers
IVF is costly and there exist economic as well as health care pressures to achieve success with each fertility treatment cycle. Multiple embryo transfers increase the chance of pregnancy as well as multiple births, but giving birth to more than one child at a time poses health risks for mothers and children. Infant low-birth weights, early births, and the increased incidence of stillbirths, neonatal deaths, and birth anomalies are all associated with multiple birth pregnancies.Citation56,57 Ontario’s Expert Panel on Infertility and Adoption concluded that multiple birth infants are 17 times more likely to be born pre-term, to require a caesarean delivery, and to need expensive care at birth and throughout their lives.Citation58
Yet, as this study reveals, Canadian gestational surrogates more frequently receive multiple embryos and until recently were more likely to experience multiple births compared with other IVF patients. This finding suggests that Canadian gestational surrogates may have been taking greater health risks than other IVF patients. It raises fundamental questions regarding patient autonomy and informed consent to medical treatment in addition to the duties of non-maleficence and beneficence owed to gestational surrogates. It also raises the issue of whether protections should be in place to limit the risks that surrogates may take, bearing in mind the strong pressures, including their own altruistic desires to assist others, that might influence a surrogate to pay insufficient regard to her own health and wellbeing.
Expensive IVF payments, intended parents’ strong desire for children, twin preference, and an underestimation of health risksCitation47,48,59 could be among the factors encouraging an altruistic surrogate, especially someone who is a close friend, relative, or co-worker, to acquiesce to multiple embryo transfer. In Canada, it is estimated that 25% of gestational surrogates are family members or friends of intended parents.Citation40 As Ashenden reminds us,Citation1 social coercion experienced by surrogates in altruistic circumstances can be subtle and mediated.
Given that gestational surrogates are younger and more likely to use embryos containing ova provided by donors younger than 35 years – factors which increase the chance of pregnancy and successful delivery – Citation33,48 it would have been expected that surrogates would be more likely to receive a single embryo transfer compared to non-surrogates who tend to be older and more often use their own ova. This has not been the case. In 2012 for example, just 26% of gestational surrogates received a single embryo transfer compared to 47% of other IVF patients. Yet, in more than half of all transfer cycles the embryos received by gestational surrogates contained ova provided by non-IM donors. When donor ova are used in fertility treatments, the age of the donor is to be used to determine the number of embryos to transfer.Citation50 For example in 2012, had the embryo transfer guidelines been followed, more than one-half of gestational surrogate cycles should have involved a single embryo transfer, yet less than one-quarter did. Based on this finding, we need to question why Canada’s embryo transfer guidelines have not been more consistently applied to gestational surrogates.
In light of the findings, the CFAS 2016 Clinical Practice Guidelines for Third Party Reproduction should provide much needed direction and guidance,Citation27 which will hopefully lead to a revision of the 2007 Canadian Medical Association’s advice to physiciansCitation60 regarding duty of care responsibilities for surrogates. In addition, Canada’s embryo transfer guidelinesCitation50 should be revised to reflect the recommendations made by the European Society of Human Reproduction and Embryology which since 2005 has called for gestational surrogacy IVF patients to receive one embryo, with two embryos being transferred in special circumstances only.Citation61,62 To provide needed oversight, the CFAS ought to provide an annual reporting of multiple births to surrogates and transfers of embryos containing IM and non-IM ova.
Lessons for law, policy and research
These findings challenge us to look more carefully at how fertility medicine is practiced and how it is delivered to surrogates, a group of patients often hidden from view and for whom the duty of care is high. While this study examined the situation of Canadian altruistic gestational surrogates, its findings may have salience in other jurisdictions. In particular, its focus on multiple embryo transfers and multiple births could be useful in research into commercial surrogacy practices occurring in less developed countries where out-of-country surrogacy is becoming a growing industry, an area recently identified as constituting a significant knowledge gap.Citation63
This paper shows that more information exists about Canada’s gestational surrogacy practices than has been acknowledged. Moreover, analysis of ART treatment trends over time can reveal changes in fertility treatments, highlight areas of differing medical practice, and pin-point topics meriting further investigation. However, the data source cannot fill the longstanding data gaps pertaining to traditional and foreign surrogacy practices. Nor can it replace in-depth case studies and qualitative research; research which often adopts approaches which deviate from the medical model of family-making which for too long has dominated our understanding of infertility and surrogacy.Citation3,20,40,53,64
ART-based studies have additional data limitations, including timeliness.Citation20,33,36,41 The findings of this study are based on CARTR-BORN registry data for the years, 2001 to 2012, hence, it has not been possible to identify changes that may have occurred since 2012. Also, due to confidentiality, no provincial-level data were made available for analysis. Not knowing provincial or even regional Canadian differences masks trends which in the context of surrogacy are important given differing provincial responses to the legalisation of parental status for intended parentsCitation29,38 and in the regulation of fertility medicine.Citation25,26
Several other confounding factors limit study findings, including a lack of socio-economic and demographic information about surrogates and intended parents. For example, surrogate age is not collected by CARTR-BORN and so could not be included in the analysis. As well, Canada’s surrogate population is relatively small, though this limitation is evident in other published surrogate studiesCitation63 (). In light of these weaknesses, additional research examining trends of multiple births and embryo transfer for gestational surrogates should be undertaken as more up-to-date data become available.
In conclusion, in highlighting the growth and changes in altruistic gestational surrogacy practices in Canada, the study reveals that Canada’s altruistic solution to the tensions raised by surrogacy does not diminish the need for oversight or for additional protections. An ironic yet particularly troubling concluding observation is that Canada’s ART legislation had been designed to protect women and the children born as a result of assisted reproductive techniques. This study’s findings cast doubt on its ability to achieve these objectives.
2013 UPDATE:
In 2013, there were 416 gestational surrogate IVF cycles resulting in 166 pregnancies, and 116 live births of which 28 were multiple births. Thus in 2013, the level of multiple births rose to 24.1% reversing the trend of declining multiple births. A total of 145 infants were born to gestational surrogates in 2013 bringing the total number of children born to gestational surrogates to 948 for the period 2001-2013.
Acknowledgements
Mr. Daniel Bédard and Ms. Jodi Wilding, CARTR-BORN; Dr. Sally Sheldon and anonymous reviewers.
Notes
* A treatment cycle is considered to have “started” when a woman undergoing ovarian stimulation receives the first dose of gonadotropins or, in a non-stimulated cycle (e.g., for Frozen Embryo Transfer (FET)), when monitoring is begun.
References
- S. Ashenden. Reproblematising relations of agency and coercion: Surrogacy. Madhock Phillips Wilson. Gender, Agency and Coercion. 2013; Palgrave Macmillan: Basingstoke, 195–218.
- E. Teman. Embodying Surrogate Motherhood: Pregnancy as a Dyadic Body Project. Body and Society. 15(3): 2009; 47–69.
- M.L. Shanley, S. Jesudason. Surrogacy: Reinscribing or Pluralizing understandings of Family?. Cutas Chan. Families: Beyond the Nuclear Ideal. 2012; Bloomsbury: London, 110–122.
- D. Dickenson. Property in the body: Feminist perspectives. 2007; Cambridge University Press: Cambridge.
- A. Phillips. Our Bodies, Whose Property. 2013; Princeton University Press: Philadelphia.
- Assisted Human Reproduction Act SC 2004 c-2. Amended 2012.
- J.C. Daniluk, E. Koert. Childless Canadian men’s and women’s childbearing intentions, attitudes towards and willingness to use assisted human reproduction. Human Reproduction. 27(8): 2012; 2405–2412.
- Lau, A. My co-worker gave birth to my baby. Chatelaine Magazine, April 18, 2014. http://www.chatelaine.com/health/coworker-gave-birth-to-my-baby/
- Treleaven S. What it feels like to have children by a surrogate. Chatelaine Magazine, November. 20, 2013.http://www.chatelaine.com/living/real-life-stories/what-it-feels-like-to-have-children-by-a-surrogate/.
- Ewart K, Tansey C, Moore T. Candid chat about surrogacy. Chatelaine Magazine, March 18, 2014. http://www.chatelaine.com/living/cityline/can-you-pay-a-surrogate-in-canada/
- Desrosiers S. A surrogacy story: Parts 1 &2. Parenting Times, February/March 2015; April/May 2015. http://www.ottawaparentingtimes.com/a-surrogacy-story-part-1/; http://www.ottawaparentingtimes.com/a-surrogacy-story-part-2/
- CBC News. Greg and Elaine Smith fight to bring surrogate-born twins home from Mexico. http://www.cbc.ca/news/canada/british-columbia/greg-and-elaine-smith-fight-to-bring-surrogate-born-twins-home-from-mexico-1.2933862. January 27, 2015
- Blackwell T. Canadian surrogates get hefty bills as hospitals start charging when babies heading to foreign parents. National Post, February 21, 2013. http://news.nationalpost.com/2013/02/21/ontario-surrogate-gets-1400-bill-after-giving-birth-as-hospitals-start-charging-third-party-carriers-for-post-natal-care/
- CBC News. Quebec to reimburse gay men for surrogacy costs, Celebrity radio host Joël Legendre and husband first to receive coverage in Quebec. http://www.cbc.ca/news/canada/montreal/quebec-to-reimburse-gay-men-for-surrogacy-costs-1.2620309. April 24, 2014
- E. Nelson. Global trade and assisted reproductive technologies: Regulatory challenges in international surrogacy. Journal of Law, Medicine & Ethics. 2013; 240–253. Spring.
- K. Busby, D. Vun. Revisiting ‘The Handmaid’s Tale’: Feminist theory meets empirical research on surrogate mothers. Canadian Journal of Family Law. 26(1): 2010; 13–93.
- K. Busby. Of surrogate mother born: Parentage determination in Canada and Elsewhere. Canadian Journal of Women & Law. 25: 2013; 284–314.
- K. Lozanski. Transnational surrogacy: Canada’s Contradictions. Social Science & Medicine. 124: 2015; 383–390.
- V. Panich. Surrogate Tourism and Reproductive Rights. Hypatia. 28(2): 2013; 274–289.
- C. Thompson. Making parents: The Ontological Choreography of Reproductive Technology. 2005; MIT Press: Cambridge, Mass.
- D. Proctor. Cancer Wars: How Politics Shapes What We Know and Don’t Know about Cancer. 2005; Basic Books: New York.
- 106 Stat. 3146 – Fertility Clinic Success Rate and Certification Act of 1992.
- Human Fertilisation and Embryology Act 1990 amended 2008.
- 2010 SCC 61, [2010] 3 S.C.R. 457.
- Quebec Government. An Act respecting clinical and research activities related to assisted procreation, CQLR.C-A-5.01. http://legisquebec.gouv.qc.ca/en/ShowDoc/cs/A-5.0. 2009 amended 2015
- Ontario Government. Building Ontario Up: Ontario Budget. 2015
- J. Havelock, K. Liu, Levitan. Guidelines for Third Party Reproduction. 2016; CFAS.
- BORN. websitewww.born.ca
- R. Tremblay. Surrogates in Quebec: The good, the bad and the foreigner. Canadian Journal of Women & Law. 27(1): 2015; 94–111.
- G. Bernstein. Unintended consequences: Prohibitions on gamete donor anonymity and the fragile practice of surrogacy. Indiana Health Review. 10(2): 2013; 291–324.
- F2013-001510 Surrogacy Treatments and information, 2007-2012. HFEA.
- Email exchange. BORN, March 16, 2016.
- Perkins KM, Boulet S, Jamieson D, et al. 2016. Trends and outcomes of gestational surrogacy in the United States. Fertility and Sterility, 2016 April 14. Pii:S0015-0282 (16)611057-9 .
- S. Sundaram, D.M. Kissin, S.B. Crawford. Surveillance Summaries, Assisted Reproductive Technology. Surveillance – United States, 2012. MMWR. 62(9): 2015
- Council for Responsible Genetics. Surrogacy in America. http://www.councilforresponsiblegenetics.org. 2010
- J. Gunby, F. Bissonette, C. Librach. 2001-2007, Assisted Reproduction Technologies (ART) in Canada. Fertility and Sterility. 2006-11 J. Gunby. 2008-2012 results for Canadian ART Register. www.cfas.ca
- E. Nelson. Law, Policy and Reproductive Autonomy. 2013; Hart Publishing: Oxford.
- B. Fauser, P. Devroey. Baby Making: What new Reproductive Treatments Mean for Families and Societies. 2011; Oxford University Press: Oxford.
- S. Dar, T. Lazer, D. Brasilie. Assisted reproduction involving gestational surrogacy: an analysis of the medical, psychosocial and legal issues: experience from a large surrogacy program. Human Reproduction. 30(2): 2015; 345–352.
- Commissaire à la santé et au bien-être. Avis détaillé sur les activités de procreation assistée au Québec. 2014; Gouvernement du Québec.
- Canadian Assisted Reproductive Technologies Registry. Better Outcomes Registry & Network Ontario. Ottawa ON, November. 2015
- Analyses of the National ART Surveillance System (NASS) data. Written communication with the Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, August 8, 2015 & March 16, 2016.
- C.O. Schmidt, T. Kohlmann. When to use the odds ratio or the relative risk?. International Journal of Public Health. 165–7: 2008
- Statistics Canada. CANSIM Tables: 102-4509; 053-001.
- HFEA. Trends in Fertility Treatment, 2013: Trends and Figures. 2014. www.hfea.gov.uk
- F. Price. Having triplets, quads or quins: Who bears the responsibility?. Stacey. Changing Human Reproduction: Social Science perspectives. 1992; Sage: London, 92–118.
- A.D. Kulkarni, D.J. Jamieson, H.W. Jones. Fertility treatments and multiple births in the United States. New England Journal of Medicine. 23: 2013; 2218–2225.
- H. Ragoné, Ragoné Franklin. Incontestable Motivations. 1998; University of Pennsylvania Press: Philadelphia, 118–131.
- J. Min, C. Sylvestre. Guidelines for the number of embryos transferred: Clinical Practice Guidelines. 2013; CFAS.
- R. v. Leia Picard and Canadian Fertility Consulting Ltd. Statement of Facts. http://noveltechethics.ca/files/files/ELA2/AHR/AHRA_Facts.pdf
- F. Baylis, C. Downie, D. Snow. Fake it till you make it: Policy making and assisted human reproduction in Canada. Journal of Obstetrics and Gynaecology. 3(6): 2014; 510–512.
- K. Horsey. Surrogacy in the UK: Myth busting and reform. 2015; Surrogacy UK: London.
- Manitoba Law Reform Commission Assisted Reproduction and Birth Registration: Issue Paper. http://manitobalawreform.ca, April. 2014
- Processing and Distribution of Semen for Assisted Conception Regulations. SOR/96-254.
- H.B. Jeng, L.S. Wilcock. Low and very low weight infants conceived with the use of assisted reproductive technology. New England Journal of Medicine. 346: 2002; 731–737.
- P.O. Pharoah. Risk of cerebral palsy in multiple pregnancies. Clinics in Perinatology. 33: 2006; 301–313.
- Expert Panel on Infertility and Adoption. Raising Expectations. 2009; Ontario Government: Toronto.
- H.W. Jones, J.A. Schnorr. 2001. Multiple pregnancies: Call to Action. Fertility and Sterility. 75(1): 2001; 11–13.
- D.R. Reilly. Surrogate pregnancy: A guide for Canadian prenatal health care providers. Canadian Medical Association Journal. 176(4): 2007; 483–487.
- F. Shenfield, G. Pennings, S. Cohen. ESHRE Task Force on Ethics and Law 10: Surrogacy. Human Reproduction. 20(10): 2002; 2705–2707.
- F. Shenfield, G. Pennings, S. Cohen. ESHRE’s good practice guide for cross-border reproductive care for centres and practitioners. Human Reproduction. 26(7): 2011; 1625–1627.
- V. Söderström-Anttila, U.B. Wennerholm, A. Loft. Surrogacy: Outcomes for surrogate mothers, children and the resulting families – a systemic review. Human Reproduction. 22(2): 2016; 260–276.
- S. Imrie, V. Jadva. The long-term experiences of surrogates: relationships and contact with surrogacy families in genetic and gestational surrogacy arrangements. Reproductive Biomedicine Online. 29: 2014; 424–435.